Medicare FraudCategory:
Medicare has had an exciting history with prior authorization. Medicare prior authorization has become controversial over the years because of Medicare Advantage.
Have You Always Been Subject to Prior Authorization?
Health plans started using prior authorization in the 1960s. Hospital admittance grew after the creation of Medicare and Medicaid. At the same time, more employers began offering employees health insurance as part of their compensation package. Medical costs grew significantly, particularly hospital stays.
Insurance companies began implementing utilization reviews in the 1960s. Utilization reviews were a process to reduce the overutilization of resources and identify waste. Registered nurses initially performed utilization reviews in hospital settings. The skillset gained popularity within the health insurance industry as research grew around medical necessity, misuse, and overutilization of services.

Health plans reviewed claims for medical necessity and hospital length of stay. Health plans began to require physicians to certify the admission and subsequent days after admission to help contain costs. Prior authorization originated from the use of utilization reviews.
Fast-forward to the present day. You were subject to prior authorization when you entered the workforce and received employer-provided group health insurance as a benefit. The insurance company determines if it is “medically necessary” and covered by the policy your company purchased when you have any medical procedure. Then there is further discussion about the appropriate charges. Whether or not you were aware of it, prior authorization has always been part of your health insurance coverage.
Why Do Insurance Companies Use Prior Authorization?
Prior authorization is a medical management tool. Doctors and insurance companies work together to ensure that a specific treatment or service is the best option for the patient’s needs.
The purpose of prior authorization is to identify and discourage unnecessary and costly low-value services to reduce wasteful spending without impeding quality healthcare services.
Prior authorization, supervision, audits, and other compliance tools help identify and root out fraud, waste, and abuse in the healthcare system. The ultimate purpose is to reduce costs for the consumer and prevent unnecessary treatments.
The Department of Justice announced today (Feb 17, 2021) criminal charges against 138 defendants, including 42 doctors, nurses, and other licensed medical professionals, in 31 federal districts across the United States for their alleged participation in various healthcare fraud schemes that resulted in approximately $1.4 billion in alleged losses.
The charges target approximately $1.1 billion in fraud committed using telemedicine, $29 million in COVID-19 healthcare fraud, $133 million connected to substance abuse treatment facilities or “sober homes,” and $160 million connected to other healthcare fraud and illegal opioid distribution schemes across the country.

While most doctors, medical professionals, and medical facilities are honest and act with integrity, an element will always and continually seek illicit gain costing consumers and taxpayers untold amounts. This results in higher insurance premiums and medical costs. It is naive to believe all are good actors and that every recommended treatment and service is the best fit.
Why Does Original Medicare Not Use Prior Authorization?
In part, the Medicare prior authorization controversy is that “Original Medicare” does not require prior authorization for most procedures, and Medicare Advantage does. (Original Medicare is just Medicare Part A and Part B. The payment structure is called fee-for-service. Medicare Advantage (or Part C) is Medicare administered by a private insurance company contracted and approved by Medicare.)
At first glance, you probably ask, ‘Why does Original Medicare not require prior authorization’ because prior authorization is common practice in the health insurance world? No company will leave the decision to spend potentially tens of thousands of dollars, even millions, to one person without some oversight.
When Medicare was established, Congress included certain arrangements and excluded others. In Section 1862(a)(1)(A) of the Social Security Act:
“No payment may be made under Part A or Part B for any expenses incurred for items or service which . . .. are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed member . . ..”
The key phrase is “reasonable and necessary.” “Reasonable and necessary” has been interpreted over the years very broadly. If a submitted claim is in an allowed category and not excluded, the submission is “reasonable and necessary.”
The doctor authorizes an MRI of the shoulder because the patient complains of problems. MRIs are covered. This procedure is “reasonable and necessary” because it is not an uncommon practice, even if there may be less expensive diagnostic procedures or treatments.
As you can probably guess, this broad interpretation with no oversight or accountability will result in large amounts of fraud, waste, and abuse.
Why Is Medicare Advantage Prior Authorization So Controversial?

The short answer to why is that Original Medicare doesn’t require prior authorization. The controversy is some believe beneficiaries are being denied essential medical services and treatments. Beneficiaries and medical professionals do not even attempt to overturn denials because they believe the appeal process is so burdensome.
The facts, however, do not paint such a sad picture. The Office of the Inspector General reviewed a large number of Medicare Advantage Organizations (MAO), reviewing 448 million preauthorization requests in 2016. Of those, MAOs denied about 1 million preauthorization requests for a denial rate of 4 percent—4 percent is tiny.
The September 2018 Office of Inspector General report found that Medicare Advantage Organizations (MAO) overturned 75 percent of their own denials from 2014-2016, overturning approximately 216,000 yearly. During that same period, independent reviews discovered additional requests that had been inappropriately denied.
The most surprising finding, however, is that only one percent of beneficiaries and providers appealed their denial, which raised the question: how many were denied necessary treatment because the process is so arduous?
Unfortunately, the study does not give a coherent explanation of the denials. From my experience of doing Medicare planning for a decade with thousands of beneficiaries, doctors’ offices do not always submit requests with detailed documentation in support. When the request is denied, they blame the insurance company, and the effort stops unless the patient pushes the issue.
The other reason I find for denial is the doctor’s office uses the wrong billing code. Quite often, the insurance company does not give any explanation in those cases. The response is “denied.” The solution requires the doctor’s office to call and talk with the claims department about billing codes, documentation, and supporting tests. In the absence of these items, nothing happens.
Unfair Statistics and Sensational Journalism
The Department of Health and Human Services Office of Inspect General (OIG) conducted a study of Medicare Advantage Organizations’ (MAO) denial of prior authorizations during one week (June 1-7, 2019). In that week, there were 250 denials. The OIG discovered that 13 percent of these prior authorizations were incorrect. This amounted to 33 cases.
Later in the same report, they admitted the usual national average is 5 percent. No reason was given why the study was not expanded when the conclusions from their study did not coincide with other long-standing evidence, particularly when the study was so microscopic–one week and 250 cases.

In the same study, they did not review the cases where the prior authorization was approved when it should have actually been denied. There was also no control group to compare against. The OIG did not study fee-for-service Medicare billing for fraudulent or wasteful claims or denials on their part.
The New York Times piled on in an April 2022 article. They presented a very slanted view of the study, beginning the article with “Medicare Advantage plans often deny needed care, federal report finds.” Only toward the very end of the article did the author get into any of the facts of the report. The general impression during the first half of the article is Medicare Advantage denies its clients the necessary medical care they need.
Why Are Medicare Prior Authorization Denials Overturned?
Denials may be overturned for many reasons. First, there were errors on the part of the insurance company. The decision was incorrect.

Errors on the part of the doctor’s office or medical facility. They did not include sufficient documentation or incorrect information. The denial is reversed, then. The provider may add new information from additional tests in the appeal process that contributes to an overturn.
The overturn does not necessarily mean the MAO acted inappropriately, but the process and extra steps critics claim create friction in the system. Patients may wish to avoid going through the trouble of appeal. Doctors may not make recommendations because of a history of denials.
Did Medicare Ever Use Prior Authorization?
The Medicare practice of accepting bills from providers at face value without question as “reasonable and necessary” was an established and haloed practice from the beginning of Medicare. All parties who benefited the most—except U.S. taxpayers—were unmotivated to change until the wheelchair scandal.
In 1999 it was discovered that Medicare spent $8.2 billion to procure power wheelchairs and “scooters” for 2.7 million people. A large portion was paid to scammers because they discovered that Medicare not only did not require prior authorization for wheelchairs, but Medicare did not even review the authenticity of the claims.
A Washington Post article published in August 2014 highlighted the massive fraud of Medicare’s resources. The article chronicled the sensational scams and trials of many Medicare swindlers. The outrageous theft of public funds and the massive fraud shamed CMS to amend its regulations to finally require preauthorization for some “durable medical equipment,” i.e., electric wheelchairs.
Bureaucrats inside CMS admitted they knew how the wheelchair scheme worked as early as 1998. But it was not until 15 years later that officials finally did enough to curb the practice significantly. Durable medical equipment—electric wheelchairs—is the only exception to the “reasonable and necessary” practice. They must be preapproved.
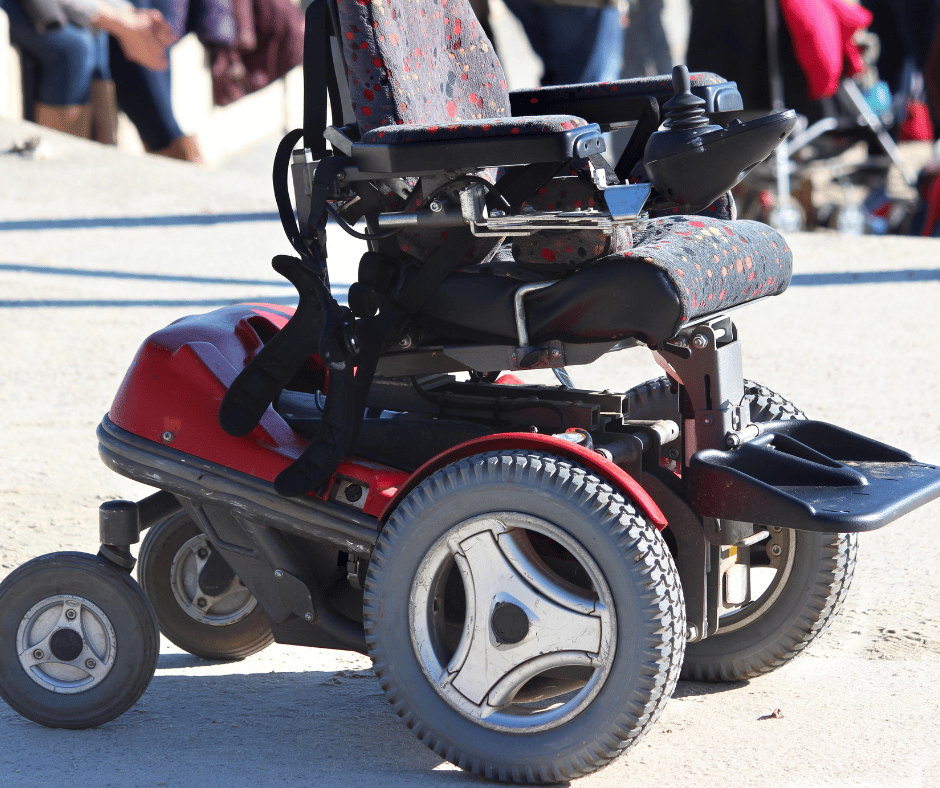
Consequently, hundreds of millions of false and unnecessary claims were paid over many years in a massive Medicare fraud. Once the bureaucratic problem was fixed, and claims were more thoroughly reviewed, an enormous shift occurred. Medicare reimbursements for motorized wheelchairs fell from $32 million every month to $7 million—a 78 percent decrease.
The Medicare Claims System Is Designed for Fraud, Waste, & Abuse
By law, Medicare must pay most of its claims within 30 days. In that short window, it is supposed to filter out the fraud and uncover claims where the diagnosis or the prescription is bogus.

The system attempts to ameliorate the damage through a “pay and chase” policy. The bill is paid, then it is reviewed. Only a tiny fraction of claims — 3 percent or less — are reviewed by a live person before they are paid. The rest are reviewed only after the money is spent. If at all.
The whole Medicare claims process is set up as an honor system for the richest program managed by the U.S. government. It is a thief’s dream.
Medicare Prior Authorization Test Program
In March 2017, CMS (Center for Medicare & Medicaid Services) designed a test program for preauthorization for fee-for-service Original Medicare. In the month of March, the GAO (U.S. Government Accountability Office), in a Senate report, estimated a savings of $1.1 to $1.9 billion when preauthorization was used that month. The report estimated the federal government made an estimated $36.2 billion in improper payments for the Medicare fee-for-service program from July 2015 to June 2016.
The committee’s recommendation became the report’s title— “CMS Should Take Actions to Continue Prior Authorization Efforts to Reduce Spending.” The prior authorization programs created to monitor and measure improper payments were discontinued and never recommissioned.
Original Medicare Fee-For-Service vs. Medicare Advantage
The government created Medicare in 1965. It had been a long-time project of the Democratic Party. CMS (Center for Medicare & Medicaid Services), Department of Health & Human Services, and Social Security Administration are government agencies. Politicians of all political parties exercise control and funding over these agencies and programs. The agencies are staffed by thousands of bureaucrats and government union workers. A tremendous amount of various and conflicting self-interests, power, and money are all mixed together.

To save Medicare from ballooning budgets and to offer an alternative to citizens, the same politicians, programs, and agencies partnered with private insurance companies to control spending and improve patient care. What is now known as Medicare Advantage began back in the 90s.
The two ways of doing government healthcare for seniors are in competition. Politicians view the world through different ideologies and support policies and programs based upon their political views. Those who support the various political ideologies will support or attack these two platforms accordingly.
It is vital to find all the relevant facts, make your own comparisons and analysis, and determine where lies the truth and the better path.
 What is Medicare Fraud?
What is Medicare Fraud?
The Medicare Fraud definition is knowingly collecting money from the Medicare program when you are not entitled to the reimbursement. Fraud occurs when someone knowingly deceives Medicare to receive payment when they should not, or they receive a higher payment than they should.
The three keys to a definition of Medicare fraud are the person and/or institution must knowingly carry out the act. It cannot be by accident, a mistake, or because of misinformation. Fraud requires the person to know that they are committing fraud, and they still actively choose to do so.
Fraud requires deception. If Medicare knew what was happening, Medicare would not pay the claim. Somehow the perpetrator disguises the act so that Medicare is not aware of the fraud being committed and thus pays the criminal.
Third, there needs to be some remuneration or favor gained from the act. The fraud often results in payments or overpayments, but it could also include referrals or business directed to a particular entity under the auspices of Medicare where the entity benefits from the additional business.
Medicare Fraud can manifest itself in many ways. Some Medicare fraud is straightforward. Other activities may not appear as fraudulent at first glance.
What Are Medicare Fraud Red Flags?
- Using another person’s Medicare number or card is clearly fraud.
- Knowingly billing Medicare for appointments patients fail to keep is Medicare fraud.
- Knowingly billing for services not furnished, supplies not provided, or both, including falsifying the records to show delivery of such items, is fraud.
- Knowingly billing for services at a level of complexity higher than services actually provided or
documented in the medical records is fraud. - Knowingly ordering medically unnecessary items or services for patients is Medicare fraud.
- Continuing to bill Medicare for rented medical equipment after the item was returned is Medicare fraud.
- Paying for referrals by the rules of Medicare is fraud, or directing business to certain vendors for compensation is Medicare fraud.
Medicare Fraud Billing
A common fraudulent practice is “Phantom billing.” Phantom billing, as it sounds, is fake bills. A medical provider bills Medicare for a procedure that was never performed. It could be a test that was performed but completely unnecessary.
A provider bills for medical equipment that was never delivered–CPAP machine. The doctor prescribes a CPAP, but the patient chooses not to get it. The facility orders the machine and bills for it, but it is delivered to the facility and resold later. Or the vendor bills for a new machine, but it is a used or repurposed machine delivered to the patient. The patient is led to believe that the machine is brand new.
A client of mine called me a few years ago to complain about his doctor. He had gone in for a physical. The doctor didn’t perform all the blood work for a normal physical by Medicare’s standards, but he submitted the bill for a physical, a larger payment than just an office visit. The doctor was caught. The insurance company told the doctor he had to notify the client he had not performed the complete physical. My client was given a choice to come back at no charge to complete the physical, or the doctor had to resubmit the bill as an office visit at a lower reimbursement.
My client was on a Medicare Advantage plan, so the insurance company caught it right away. Regular Medicare is not so vigilant in monitoring billing, as you will read further down.
Patients can also get in on the scam. A Medicare beneficiary may provide her number for a kickback or share in an illegitimate reimbursement.
Insurance agents can play the game too. An insurance agent lets it be known that he will pay a certain amount of money contingent on someone signing an application for a Medicare plan or supplement. There seems to be no end to the schemes and scams people will go to for an easy buck.
What Are Instances of Medicare Fraud News?
My favorite Medicare Fraud detection case is the electric wheelchair caper. (This article does not intend to impugn legitimate medical supply companies or discount persons who truly need electric wheelchairs.) This particular scam ran for 15 years before it was discovered. Eventually, Medicare woke up and prosecuted the criminals.
Medicare had a blind spot in its processing systems. Human beings did not process claims for motorized wheelchairs. Only 3 percent of electric wheelchair claims were ever reviewed by Medicare personnel. The claim was automatically paid upon request when submitted through the Medicare billing system.
Consequently, hundreds of millions of false and unnecessary claims were paid over many years. Once the bureaucratic problem was fixed and claims were more thoroughly reviewed, an enormous shift occurred. Medicare reimbursements for motorized wheelchairs fell from $32 million every month to $7 million. A 78 percent decrease. That was one big glitch in the system!
Medicare Fraud Examples: Electric Wheelchairs
- In San Francisco, a 71-year-old doctor was sentenced to 24 months in prison for her role in a wheelchair scam. Medicare paid $1.6 million between 2006 and 2011 for non-existent wheelchairs. The Prosecutors found the doctor received $100 for each bogus prescription she wrote for a patient who did not need a wheelchair.
- In Los Angeles, a medical supply company owner was sentenced to 30 months in prison for $1.5 million in fraudulent payments for wheelchairs between 2006 and 2009. The patients did not need the chairs.
What Are Signs of Medicare Fraud?
Upcoding is another fraudulent scam that some health care professionals run. Healthcare providers use more than 7,800 CPT (Current Procedural Technology) submission codes. Collectively, these codes represent all of the procedures, conditions, and drugs that are currently reimbursable by the insurance industry. Each of them has an associated cost for individuals and insurance companies, based upon the urgency of the issue and the complexity of the decision-making required of the healthcare provider. Medicaid and Medicare providers are reimbursed based on these codes.
currently reimbursable by the insurance industry. Each of them has an associated cost for individuals and insurance companies, based upon the urgency of the issue and the complexity of the decision-making required of the healthcare provider. Medicaid and Medicare providers are reimbursed based on these codes.
For example, a five-minute consultation with a nurse for a minor medical question would receive a different, less expensive CPT (Current Procedural Technology) submission code than the one for a complete examination by a doctor lasting 45-minutes. When a physician charges Medicare or Medicaid for the more expensive 45-minute examination when the five-minute consultation is what actually occurred, this will constitute upcoding and thus fraud.
What Are The Most Common Forms of Medicare Fraud?
Unbundling is another very widespread form of Medicare fraud. This fraudulent scheme involves billing for individual procedures usually performed and billed together under a single CPT code. The billing codes for complicated medical operations have associated components built into their CPTs.
For example, a hip replacement surgery may factor in the surgeon’s costs and the use of the operating room together. There is one code for one single procedure.
Unbundling occurs when a healthcare provider submits each component within a CPT to Medicare or Medicaid separately. The multiple components create a cost redundancy where wrongdoers can unlawfully seek more reimbursement for the same procedure several times over. Unbundling is an upcoding that is a type of Medicare fraud.
More Medicare Fraud News
In April 1998, GlaxoSmithKline (GSK) settled with the DOJ (Department of Justice) over civil charges. With the critical aid of GSK employees and Medicare fraud whistleblower Robert Marena, the government learned of a scheme where the lab “bundled” many blood tests together under one cheaper billing package, assuring providers that this would not raise Medicare prices. However, once the lab had processed the tests, GSK “unbundled” the package and billed the federal program for each one separately, including the ones that the doctors had never ordered. Five years later, a Medicare fraud qui tam settlement was reached with GSK for $325 million. Marena and the two other chief relators split $52 million as their Medicare fraud whistleblower reward.
The Medicare whistleblower reward program pays out $690,000 on average per case.
 How to Prevent Medicare Fraud?
How to Prevent Medicare Fraud?
To stop Medicare Fraud, CMS (Center for Medicare & Medicaid Services) started a Medicare fraud prevention campaign several years back called “Guard Your Card.” They ran public service announcements about never giving out your Medicare or Social Security Number to anyone except those you know should have it.
Guard Your Medicare Card
Clients will sometimes call to tell me that someone tried to get their Medicare number, claiming to be from Medicare. I tell my clients repeatedly Medicare will not call you. It is either a scammer or an insurance agent trying to sound like he is from Medicare. His goal is to sell you something. Know with whom you are speaking. If you are confused or concerned about the conversation, just hang up.
I tell my clients to call me when these situations occur. I got an email from one of my Texas clients this morning. He had received a letter he thought was from the government. He attached the letter to the email. The card looked official, I must admit, but it was typical marketing material from a salesman to get you to call in. Then the agent makes the conversation sound official as they move you toward a new Medicare product.
To prevent Medicare Fraud, you need to report suspicious activity. That is the primary way Medicare catches these criminals. Medicare’s investigators will verify the credibility of the accusation, and there will be no blowback on you when the report is done in good faith.
Remember, Medicare will never call you uninvited for your information which they already have.
Fraudulent Medicare Bills
Double-checking your billing statement is an excellent way to find fraud. You get a Medicare Summary Notice (MSN) from Medicare or an Explanation of Benefits (EOB) from the Medicare insurance company. Go down the itemized list of services and products. If something looks wrong or suspicious, call Medicare or the insurance company to verify any charges. Mistakes happen, so it’s good to review your statement.
But fraud also happens. A provider could use your Medicare number to get reimbursed for a supply or service that was not performed or more services than you received.
Medicare is now using forensic auditing to detect variants in numbers and find incidents of fraud, much like credit card companies use modeling to catch criminals purchasing items with your credit card. This type of forensic auditing saved Medicare $60 billion from 2013 to 2015.
Medicare $60 billion from 2013 to 2015.
Medicare Fraud Reporting?
There are four ways to report Medicare fraud.
-
- Medicare Fraud Hotline – 800-447-8477
- Online – Health & Human Services Office of the Inspector General
- Fax – 800-223-8164
- Mail – Office of Inspector General – ATTN: OIG HOTLINE OPERATIONS P.O. Box 23489 Washington, DC 20026
Each of the Medicare Advantage and Part D prescription drug plans has the same list of contact as well as its own internal anti-fraud infrastructure to address Medicare fraud cases. Medicare Advantage insurance companies are highly motivated to catch fraud because it directly impacts their bottom line.
 More Medicare Fraud Examples
More Medicare Fraud Examples
In April 2019, Federal officials charged Philip Esformes with paying and receiving kickbacks and bribes in the most significant Medicare fraud case in U.S. history. The most prominent fraud case brought to the Department of Justice occurred between 2007 and 2016. Philip Esformes, 48, owner of more than 20 assisted living facilities and skilled nursing homes, was the ring leader.
Fraud Is A Team Sport
Former Director of the Outreach Program at Larkin Hospital in South Miami, Odette Barcha, 50, was Esformes’ accomplice along with Arnaldo Carmouze, 57, a physician assistant in the Palmetto Bay Area. These three recruited a team of corrupt physicians, hospitals, and private practices in South Florida.
The scheme worked as follows: bribes and kickbacks were paid to physicians, hospitals, and practices to refer patients to the facilities owned and controlled by Esformes. The assisted living and skilled nursing facilities would admit the patients and bill Medicare and Medicaid for unnecessary, fabricated, and sometimes harmful procedures.
Some of the charges to Medicare and Medicaid include prescription narcotics prescribed to patients already addicted to opioids. The purpose was to entice the patients to stay at the facility longer so the billing could continue.
Another technique used by the scammers was to move patients in and out of facilities when the patients had reached the maximum number of days allowed by Medicare and Medicaid. The musical beds technique was accomplished by using one of the corrupt physicians to see the patients and coordinate for readmission in the same or a different facility owned by Esformes. Per Medicare and Medicaid guidelines, a patient is allowed 100 days at a skilled nursing facility after a hospital stay. The patient is given an additional 100 days if they spend six days outside of a facility or are readmitted to a hospital for three additional days.
The facilities not only fabricated medical documents to show treatment was performed on a patient, but they also hiked up the prices of equipment and medications that were never consumed or used.
Anti-Kickback Statute or Stark Law
The role of Barcha as the Director of the Outreach program was to expand the group of corrupt physicians and practices. She would advise the community physicians and hospitals to refer patients to the facilities owned by Esformes, and physicians and hospitals received monetary gifts in return. The law against kickbacks is called the Anti-Kickback Statute or Stark Law. This law makes it illegal for medical providers to refer patients to a facility owned by the physician or a family member for services billable to Medicare and Medicaid. It also prohibits providers from receiving bribes for patient referrals.
The involvement of Carmouze in the grand scheme was to prescribe unnecessary prescription drugs to patients who did not need the medications. He also facilitated unnecessary physician visits to the patients in the assisted living facilities owned by Esformes for the physician to bill Medicare and Medicaid. Esformes then received kickbacks. Carmouze also assisted in falsifying medical documentation to represent proof of the medical necessity for many of the medications, procedures, visits, and equipment charged to the government. In 2019, he was convicted of charges that added up to 20 years in prison.
Why is Medicare Fraud Bad?
Medicare fraud is real. It drastically increases the cost of Medicare that we, as taxpayers, fund. Being aware of how Medicare fraud works and reporting the fraud is critical to keeping our Medicare safe, secure, and vibrant for the future.
Individuals and institutions also abuse Medicare and are wasteful. Those are two other categories of activity that negatively impact the quality and cost of Medicare, but they are different from Medicare Fraud which requires knowledge and intention. Medicare Abuse & Waste will be addressed in a separate article.







