Medigap QuotesCategory:
A prospective client called me about saving money on her Medicare supplement. I asked her the basic supplement health questions and gave a quote. We set up a time to meet. At the meeting, I started going through the standard health questions on the application. When I came to the question about recommended future treatments, she said no, but the way she answered bothered me. So I asked it a different way. “Did the doctor suggest that you have anything done, like cataract surgery, knee or hip replacement?” Then she lit up. “My hips are really bad,” she said. “He thinks I should replace them sometime.” “So when you say sometime, are you talking about in a year or two?” “Oh no,” she said. “In the next couple of months.” I closed my notebook. We were done.
Supplement Health Questions Broken Down
Recommended treatments by a physician could potentially cause a problem when you switch supplements. Three things to know: 1.) what is a recommended treatment, 2.) why does it matter, 3.) what should you do about it.
Most of the time when we see the doctor it is because we are sick right now. She makes a diagnosis and recommends an immediate treatment. ‘Take this pill now.’ ‘Have open heart surgery next week.’ Sometimes the diagnosis leads to a recommendation for treatment sometime in the future. ‘Your knees are deteriorating. You should have a knee replacement in the next year or so.’ When your doctor puts a recommendation in your medical records for a future treatment, that is a big deal. To an insurance company, that means there will be a future big bill for whoever is insuring you at that time.
Understand the Supplement Health Questions
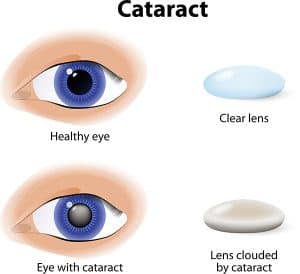 The problem is that you could get stuck with the bill instead of the insurance company if you don’t follow the rules. If you have something done that was recommend before you got the new policy, like cataract surgery within six months after getting a new Medicare Supplement, the insurance company will probably not pay their share of the expense. The health questions in the application are designed to disclose recommended treats and prevent the new insurance company from getting stuck with the bill. They would likely refuse payment and call for doctor’s records to see if there was a recommendation for treatment before you signed the application. After six months, you are less likely to have any trouble. They cannot hold back paying for treatment indefinitely. The bottom line is, if you have any recommended treatments, finish them up before switching supplements.
The problem is that you could get stuck with the bill instead of the insurance company if you don’t follow the rules. If you have something done that was recommend before you got the new policy, like cataract surgery within six months after getting a new Medicare Supplement, the insurance company will probably not pay their share of the expense. The health questions in the application are designed to disclose recommended treats and prevent the new insurance company from getting stuck with the bill. They would likely refuse payment and call for doctor’s records to see if there was a recommendation for treatment before you signed the application. After six months, you are less likely to have any trouble. They cannot hold back paying for treatment indefinitely. The bottom line is, if you have any recommended treatments, finish them up before switching supplements.
Manage the Supplement Health Questions
 This problem, of course, can be avoided. Check with your doctor. See if he is recommending any treatments and see if he put that in your medical records. Check with the insurance company if you recently switched supplements. Doctor’s offices will not usually check with an insurance company on a supplement because they will assume the insurance company will pay when Medicare pays. If you recently switched supplements, call and ask ahead of time if there will be any issues about a procedure. It is always good to cross your T’s and dot your I’s when it comes to new insurance plans.
This problem, of course, can be avoided. Check with your doctor. See if he is recommending any treatments and see if he put that in your medical records. Check with the insurance company if you recently switched supplements. Doctor’s offices will not usually check with an insurance company on a supplement because they will assume the insurance company will pay when Medicare pays. If you recently switched supplements, call and ask ahead of time if there will be any issues about a procedure. It is always good to cross your T’s and dot your I’s when it comes to new insurance plans.
Ask an Expert about Supplement Health Questions
A mistake around a recommended treatment when changing Medicare supplements could result in bills to you for thousands of dollars. Know whether you have any recommendations from a physician for future treatments in your records. Understand what that means in relationship to a new Medicare supplement. Talk with someone who can ask you the right questions when you are making a change to your supplement coverage 402-614-3389. OmahaInsuranceSolutions.com
For two years, my father was on dialysis. Those were tough years. When I got a client on dialysis, I wanted the best for him. Kidney dialysis is one of the pre-existing conditions that usually excludes you from a supplement. My client had a one-time opportunity. I was going to make sure he got it!
Obama Care Confuses Pre-Existing Conditions
![]() Pre-existing conditions are confusing when it comes to Medicare. The ACA (Affordable Care Act) a.k.a. Obama Care made it more confusing because ACA covers pre-existing conditions, but ACA is not Medicare. Different rules govern Medigap policies. ACA applies to everyone 64 and younger. Medigap policies are for everyone 65 and older.
Pre-existing conditions are confusing when it comes to Medicare. The ACA (Affordable Care Act) a.k.a. Obama Care made it more confusing because ACA covers pre-existing conditions, but ACA is not Medicare. Different rules govern Medigap policies. ACA applies to everyone 64 and younger. Medigap policies are for everyone 65 and older.
Medicare Has No Pre-Existing Conditions
Medicare itself cannot deny coverage to anyone because of pre-existing conditions. Medicare means Original Medicare. Original Medicare is Medicare Part A for hospital and Part B for doctors and outpatient. Medicare Part D cannot be denied for pre-existing conditions no matter the condition or cost of the medications. Medicare Part C (or Medicare Advantage) must accept you as well, but for one exception–ESRD (End Stage Renal Disease). You can be denied entrance to Medicare Advantage if your kidneys are permanently shut down and you are on dialysis. All Medicare beneficiaries may enroll in a Medicare Advantage plan, except for that one pre-existing condition.
Medigap Has Pre-Existing Conditions–Sometimes
 An insurance company, however, can deny you a Medicare Supplement/Medigap plan because of pre-existing conditions, except during your Open Enrollment Period or Guaranteed issue. The rules around your Open Enrollment Period are confusing. You can enroll in Medicare when you turn 65 and enroll in Medicare Part B. That is called your Open Enrollment. The time period for that is 3 months before the month of your birthday, the month of your birthday, and 3 months after your birthday. The same term–Open Enrollment–is used for enrolling in a Medicare supplement, but the time period is different. Open Enrollment for a supplement is from the month of your birthday and five months after. Same term–Open Enrollment Period–but different time periods that apply to different things. Isn’t that nice!
An insurance company, however, can deny you a Medicare Supplement/Medigap plan because of pre-existing conditions, except during your Open Enrollment Period or Guaranteed issue. The rules around your Open Enrollment Period are confusing. You can enroll in Medicare when you turn 65 and enroll in Medicare Part B. That is called your Open Enrollment. The time period for that is 3 months before the month of your birthday, the month of your birthday, and 3 months after your birthday. The same term–Open Enrollment–is used for enrolling in a Medicare supplement, but the time period is different. Open Enrollment for a supplement is from the month of your birthday and five months after. Same term–Open Enrollment Period–but different time periods that apply to different things. Isn’t that nice!
During your Open Enrollment Period for a supplement, the insurance company may not ask you health questions. They must give you the best possible rate. Even your weight is not counted against you if you are a few pounds over the normative height/weight charts. You can be on chemo, dialysis, recovering from a stoke. It doesn’t matter. The insurance company MUST take you during this time period. AFTER the six month Open Enrollment Period, they can ask health questions when you go to purchase a Medicare supplement, and based upon your answers, the insurance company could rate or even deny you.
 What are some of the health questions? Are you in a wheel chair? Are you an insulin dependent diabetic? Have you had a heart attack, stroke, or cancer in the past two years? All of these questions are “knock out” questions. If you answer in the affirmative, you will be denied a Medicare supplement. You cannot be denied Medicare, but you can be denied the ability to purchase a Medicare supplement at any price.
What are some of the health questions? Are you in a wheel chair? Are you an insulin dependent diabetic? Have you had a heart attack, stroke, or cancer in the past two years? All of these questions are “knock out” questions. If you answer in the affirmative, you will be denied a Medicare supplement. You cannot be denied Medicare, but you can be denied the ability to purchase a Medicare supplement at any price.
Know the Rules or Find Someone Who Does
The ACA changes that permit acceptance into a health plan with pre-existing conditions created confusion in the Medicare world. Beneficiaries need to clearly understand that a pre-existing condition can count you out of a supplement unless it is your Open Enrollment Period or Guarantee issue situation. It is critical that persons with serious health issues be vigilant about these Medicare rules and/or find someone who will be vigilant for you.
Don’t miss your Open Enrollment Period. If there are any questions, give us a call at 402-614-3389 or even call Medicare 800-633-4227. Make sure you understand the rules that apply to you.
Contact: Omaha Insurance Solutions
One of the most painful calls I get is from a client who is calling on behalf of a parent. They want to know if there is anything I can do for a parent who is paying huge monthly premiums for her Medicare supplement. The agent who signed them up is long gone. The supplement has increased over the years due to age and rate increases. Now the parent is in her 80’s and in poor health, and the monthly premium is financially crushing. Many times there is nothing I can do because their mom or dad cannot pass the underwriting questions to change to a supplement that would be significantly less. They missed out on one of the keys to unlocking Medicare–an agent who shops her policy each year.
Five Keys to Unlocking Medicare
 There are five keys to unlocking Medicare. First you need to do some research yourself. The bible for Medicare is Medicare & You. It is the official Medicare Handbook that the Center for Medicare & Medicaid Services publishes each year. The Medicare.gov website is an endless source of resources. It is important to do your own research so you are familiar with the proper Medicare terminology. That way, you can better understand a serious discussion around Medicare.
There are five keys to unlocking Medicare. First you need to do some research yourself. The bible for Medicare is Medicare & You. It is the official Medicare Handbook that the Center for Medicare & Medicaid Services publishes each year. The Medicare.gov website is an endless source of resources. It is important to do your own research so you are familiar with the proper Medicare terminology. That way, you can better understand a serious discussion around Medicare.
The Big Key
Key number two: search for an experienced, independent agent. Experience means they have been doing this for years. Ask them when they got their insurance license. They should be able to spit that out without thinking. Ask if they do this fulltime. There are a lot of insurance companies and agencies who hire part-time people to increase their production. They give them little education or training. Even less support. Most drop out of the business after six or nine months. That probably is not the person you want. Ask if they are independent. Some insurance agents can only offer one company. They cannot shop the world of Medicare plans. Ask them to list the companies they offer. If they change the subject or only list one or two, you have your answer.
 Key number three: ask questions. As I tell my clients who are aging into Medicare, you turn 65 once in a lifetime. I help people turning 65 going on Medicare four or five times in a day. I am excited when someone asks me a question I haven’t heard before. An experienced agent should be able to quickly and easily explain the details of Medicare, supplements, advantage plans, prescription drugs, etc. If not, you may wish to look somewhere else.
Key number three: ask questions. As I tell my clients who are aging into Medicare, you turn 65 once in a lifetime. I help people turning 65 going on Medicare four or five times in a day. I am excited when someone asks me a question I haven’t heard before. An experienced agent should be able to quickly and easily explain the details of Medicare, supplements, advantage plans, prescription drugs, etc. If not, you may wish to look somewhere else.
Price Compare Med Sups
Key number four: compare every year. I talk to my clients at least once a year. I want to know that everything is going well. Part of the conversation is the price of their supplement. With age and rate increases, what are you currently paying? I shop their supplement right then and there over the phone. I tell them if there is a plan of equal or better value at a lower price. That prevents you from getting into the situation in your later years of a plan with back breaking premiums.
 Key number five: stay healthy! Go to the gym. Eat healthy. Chase grandchildren, pets, moving cars, anything that will get your heart rate up. One of the keys to unlocking Medicare supplements is your ability to pass underwriting questions so you can change plans and pay less. I can try different companies that have more liberal underwriting guidelines, but ultimately there are limitations for serious health issues.
Key number five: stay healthy! Go to the gym. Eat healthy. Chase grandchildren, pets, moving cars, anything that will get your heart rate up. One of the keys to unlocking Medicare supplements is your ability to pass underwriting questions so you can change plans and pay less. I can try different companies that have more liberal underwriting guidelines, but ultimately there are limitations for serious health issues.
Medicare and Medicare supplements are awesome health insurance, but to enjoy the greatest benefits from this awesome resource, you need to follow these simple five keys. Call me 402-614-3389 or the American Association of Medicare Supplements to find an experienced, independent agent near you.
 People constantly ask me, ‘What should I do about Medicare?’ They are overwhelmed with all the brochures from insurance companies. They look through the 162 pages of the Official Medicare Handbook and are further confused. Some go to the Medicare.gov website, and are confounded in attempts to navigate through the endless ocean of information. They simply ask in bewilderment, “What does everyone else do?’ A huge number of people choose a Medicare supplement, or Medigap plan, as the solution, but more of an answer is needed than just ‘everyone is doing it.’ Some thoughtful consideration is required.
People constantly ask me, ‘What should I do about Medicare?’ They are overwhelmed with all the brochures from insurance companies. They look through the 162 pages of the Official Medicare Handbook and are further confused. Some go to the Medicare.gov website, and are confounded in attempts to navigate through the endless ocean of information. They simply ask in bewilderment, “What does everyone else do?’ A huge number of people choose a Medicare supplement, or Medigap plan, as the solution, but more of an answer is needed than just ‘everyone is doing it.’ Some thoughtful consideration is required.
Part A Deductible
Medicare is a generous health plan. It covers a majority of the hospital and doctor costs, but there is some important exposure to be aware of. Medicare Part A covers the hospital, but only after you pay the deductible of $1,288. That deductible is not an annual deductible. It is per event within a 60 day period. While you would have to be very unlucky, very sick, or both, you could pay that deductible an endless number of times. That is your exposure.
Part B Co-Insurance
Medicare Part B covers 80% of the doctor and outpatient procedures. While that is quite generous, 20% of a big number is still a big number. Heart attacks, strokes, cancer treatment can run into the hundreds of thousands of dollars. Twenty percent of a $200,000 bill is $40,000. Most people would find that beyond the family budget.
MOOP
And with Part A & B, there is NO maximum-out-of-pocket (MOOP). In other words, you continue to pay as the bills roll in. You do not stop paying on deductibles and co-insurance if all you have is Original Medicare without anything else.
So comes the questions from clients: ‘What should I do about Medicare?’ Medicare supplements or Medigap plans fill in those gaps in Medicare. They cover the hospital deductibles and 20% co-insurance for doctor and outpatient use. Depending on how much you wish to cover, the Medigap plan can cover everything 100%, most of everything, or a potion. You choose. There are ten plans available.
12,200,000 Satisfied Medigap Clients
The fact that 22% of people on Medicare choose a supplement and stay on a supplement for 20-30 years tells you the level of satisfaction. There are currently 55,200,000 Medicare beneficiaries. Of that number 12,200,000 chose a supplement. That number grows each year: 9.7 million in 2010 to 12.2 million in 2015. The key number is that 9 out of 10 Medigap beneficiaries say that they are satisfied with their coverage and keep their coverage. Med Sup Conference Stats
While Medicare is a wonderful health insurance program for seniors, it doesn’t cover everything. You still have exposure to significant financial loss if you only have Medicare alone.
 One of the things that holds people back from purchasing a Medicare supplement is that they don’t know. That is, they don’t investigate what Medigap plans are, what the costs are, how much or little they cover. It is simple as making a phone call 402-614-3389. A quote will not cost you anything, but you will have some real, solid information for your decision making process. Take a couple minutes, answer a few questions, and you will be surprised how easily you can find out what you should do about your Medicare @ OmahaInsuranceSolutions.com.
One of the things that holds people back from purchasing a Medicare supplement is that they don’t know. That is, they don’t investigate what Medigap plans are, what the costs are, how much or little they cover. It is simple as making a phone call 402-614-3389. A quote will not cost you anything, but you will have some real, solid information for your decision making process. Take a couple minutes, answer a few questions, and you will be surprised how easily you can find out what you should do about your Medicare @ OmahaInsuranceSolutions.com.
You may have been caught up in the recent political circus on TV and missed the political power play behind the scenes. Congress voted to eliminate a Medicare supplement that provides first dollar coverage. (First dollar coverage means you pay no co-pays, deductibles, or co-insurance. Medicare and the Medicare supplement pay everything.) This will change everything about how you approach your Medicare, and it is a cause for re-evaluation of your Medicare Supplement plan.
Congress’s change potentially creates a problem for beneficiaries who have a Plan F supplement. Or, at least, it is reason for re-evaluation. There are other supplement plans, but which one should you choose?
Congress Tinkers with Medicare Supplement
Congress is constantly trying to fund government programs. The balancing act is to generate sufficient revenue to pay for adequate benefits without over burdening the taxpayer. Congress discovered that Medicare beneficiaries who do not pay any co-pays, co-insurance, or deductibles unnecessarily over use the medical system and consequently Medicare. The Medicare Trust Fund is stressed to the breaking point. Congress found that beneficiaries who pay co-pays, deductibles, and co-insurance do not over use the medical system. Their solution is to stop first dollar coverage. That means, supplement plans cannot pay everything. Beneficiaries must pay some kind of co-pay, deductible, or co-insurance. There must be some disincentive to over using the system.
Medicare Supplement Plan F Going Away
 The Medicare supplement plan that covers all co-pays, deductibles, and co-insurance is Plan F. You will not be able to purchase a new Plan F after December 2019. Those who have Plan F will be grandfathered in and may keep the plan. The consequence of this change is that no new beneficiaries will be joining Plan F. Insurance is built upon pools of people. Of the 10,000 people turning 65 each day in the U.S., no one will be purchasing Plan F’s after 2019. Those who have Plan F will age and die, reducing the number of persons who pay premiums. If there are fewer people paying in less premium but more and larger medical claims being paid out, the insurance company will be forced to raise rates on the existing members of the plan to keep the plan viable. While it is hard to know the future, it would be hard to say Plan F’s future will be positive after 2019.
The Medicare supplement plan that covers all co-pays, deductibles, and co-insurance is Plan F. You will not be able to purchase a new Plan F after December 2019. Those who have Plan F will be grandfathered in and may keep the plan. The consequence of this change is that no new beneficiaries will be joining Plan F. Insurance is built upon pools of people. Of the 10,000 people turning 65 each day in the U.S., no one will be purchasing Plan F’s after 2019. Those who have Plan F will age and die, reducing the number of persons who pay premiums. If there are fewer people paying in less premium but more and larger medical claims being paid out, the insurance company will be forced to raise rates on the existing members of the plan to keep the plan viable. While it is hard to know the future, it would be hard to say Plan F’s future will be positive after 2019.
Plan G is the New Plan F
 The next plan up is Plan G. The two differences between Plan F and G are: you pay the Part B deductible, which is currently $166. It is a one time annual deductible. After you pay the Part B deductible of $166, there are no more co-pays, deductibles, or co-insurance for the year. Everything will be covered 100%. Second, Plan G premium is noticeably less than Plan F’s. The other point of interest is that Plan G’s have fewer and smaller rate increases than Plan F’s.
The next plan up is Plan G. The two differences between Plan F and G are: you pay the Part B deductible, which is currently $166. It is a one time annual deductible. After you pay the Part B deductible of $166, there are no more co-pays, deductibles, or co-insurance for the year. Everything will be covered 100%. Second, Plan G premium is noticeably less than Plan F’s. The other point of interest is that Plan G’s have fewer and smaller rate increases than Plan F’s.
Shrinking Pool of Insured
Medicare trustees are trying to slow the drain on the trust fund. Eliminating first dollar coverage that Plan F’s afford was the solution. The problem is that no new members will join the pool of insured who have Plan F. Traditionally, insurance companies raise premium rates when the pools of people who pay premiums becomes smaller. Plan F members will be forced to look other places for more affordable coverage. Plan G will likely become the new Plan F.
You may wish to reconsider your supplement plan if it is Plan F. The ground is shifting. Visit OmahaInsuranceSolutions.com for the most current education on Medicare.
When I was 23, I fell down a mountain while jobbing in Mexico. It was my 2nd trip. My tumble resulted in some serious scrapes and cuts. The nurse at the school I was studying strongly suggested that I get a tetanus shot since I couldn’t remember the last time I had had one. I found a doctor who under stood a little English and I supplied the rest in Spanish. I think he injected me with the right stuff because I didn’t die or turn green. I paid him $10 US dollars. I was no worse for the wear. It is easy to bounce back when you are 23.
I’m currently 53. I don’t think I would have bounced back as readily now, but I also probably would not been running up a mountain. Accidents, however, do happen. They happen at home, and they happen abroad. A common question I get from baby boomers who travel is: ‘what will Medicare cover abroad?’ The answer is fairly simple. Nothing. Now let me offer some nuance.
Medicare and Foreign Travel
Original Medicare will cover you if you find an American hospital in a foreign country. Not very likely. You could claim Medicare when you are on a cruise if you are within 6 hours of the mainland. Original Medicare is not your solution for medical coverage in a foreign land.
Medicare Advantage may cover you for emergency and urgency care needs worldwide with some plans. You need to check your specific Medicare Advantage plan. Check under emergency and urgent care.
Medicare supplements or Medigap plans offer some minimal coverage. You generally have a $250 deductible. They will pay 80% of the medical cost up to a $50,000 LIFETIME limit. Of course, any serious accident, heart attack, stroke etc. will eat into that amount very quickly. Check the specifics of your plan.
So what is the solution? One of two things. Cash. Don’t leave home without it, and travel insurance. You can purchase travel insurance for the duration of your trip to cover anything devastating at a reasonable rate.
Vacation is about fun, so plan. Planning for the worst will insure that you have the best time during your time in the sun.
Sheep get sheared. They follow the other sheep into the pen, down the shoot, then in to the hands of the shearer and are fleeced. The ram is a alert. He doesn’t go with the flow he leads the way and butts heads when he is force to go where he doesn’t want to go.
How do people pick their Medicare supplement plan and company? They talk with their buddy on the left and their buddy on the right. ‘They both can’t be wrong.’ Everyone says Plan F is “the best.” “I never have to pay anything”—no co-pays. That’s great! Sign me up. That is the thought process of the sheep. Insurance companies love it. Insurance agents love it. Plan F is the most expensive plan in all kinds of way.
There are ten possible Medicare supplement plan types that an insurance may offer–A–N. In reality, they usually only offer 4 or 5. Plan F is the most popular as well as the most expensive. Insurance companies and agents like that because it brings in the most money and pays the highest commission. But is it the best for a client?
Plan F does cover all the deductibles and co-insurance that Medicare doesn’t cover. That is nice, but you pay a price for that convenience. It raises the question whether Plan F is the best.
Is there an alternative? How about Plan G? Plan G is very close to Plan F. The difference is that you pay the Part B deductible of $147. It is a one-time annual deductible. Once you pay your Part B deductible of $147, for let’s say a doctor’s visit, you are done for the year. Everything else will be covered 100% which is similar to a Plan F. So why plan G? Because the premium is lower—quite a bit.
Let’s do some simple math. Let’s say that a plan F is $150 per month for a 65 year old male and a plan G is $110 for the same person. The difference is $40 per month and $480 per year less for the Plan G. Subtract the $147 Part B deductible, and you are still ahead $333. Putting it another way, you are paying $333 for the convenience of having the insurance company pay your Part B deductible so that you don’t have to write a check IF you go to the doctor or have some other procedure. Multiply that times 10 years and you are at $3,330.
The second and more important consideration about Plan G is that the rate increases are smaller and less frequent. Yes premiums go up because medical costs go up, but the unusual reality about Plan G policy holders is that they generally do not go to the doctor or emergency room as frequently as Plan F policy holders. There is something about the $147 deductible that causes people to pause and think. ‘Is this really medically necessary?’ The result is that, because Plan G policy holders do not over use medical benefits to the extent Plan F policy holders do, the claims and cost are not has high. Consequently the rate increases for Plan G’s are fewer and smaller than Plan F. Plan F is the best?
Don’t be a sheep. Don’t follow the herd. Stop and look at the different plans. Ask yourself the hard question in light of the facts whether Plan F is the best. Do some analysis, and you will save money in the short, long, and longer run.
 402-614-3389; [email protected]
402-614-3389; [email protected]
Would you be interested in a service that you must absolutely have? As a matter-of-fact, almost everyone has it. It’s not free. You will have to pay, but let’s say you could get the same thing for 400% less than what most people pay. Would you be interested in a bargain like that? Most people would enthusiastically say ‘YES!’ You ask, ‘what is the bargain?’ Medicare. Medicare is a bargain!
 Everyone needs health care because everyone gets sick and needs doctors, hospitals, drugs, treatment, etc. The average cost of a decent group health plan is going to be $1,000+ per month per person. If you go into the exchange to purchase an individual plan, you are looking at $500-$600 per month WITH a $2,500 deductible, and that is not including the maximum out of pocket.
Everyone needs health care because everyone gets sick and needs doctors, hospitals, drugs, treatment, etc. The average cost of a decent group health plan is going to be $1,000+ per month per person. If you go into the exchange to purchase an individual plan, you are looking at $500-$600 per month WITH a $2,500 deductible, and that is not including the maximum out of pocket.
You may say that you only pay $50 or a $100 per month for your health plan at work. That is because your employer is paying the majority of the cost. You are not getting it for free. You’re not even getting it for a reduced price. It still costs $1,000. Your employer is taking your compensation and applying a portion to your health insurance instead of paying the money to you. It’s your money, your compensation. You are not given a choice on how to receive it. That employer portion is just part of your total compensation. And it is still part of your employer’s total expense for an employee.
You might complain that now I have to pay the full cost of health care myself. Yes, your employer is not paying for your health care because you are not working any longer. Your employer is also not paying you a salary any longer. When you go to the grocery store, you can’t use your salary to pay for the groceries. You have to use your Social Security check, savings, investments, IRA’s, etc. Your source of earned income stopped when you retired, which includes your employer subsidy for your health insurance.
The realization of the true costs of services, like health care, doesn’t diminish the fact that Medicare is a bargain!
 What does Medicare cost? For most people, you paid for Medicare Part A during the working years, so there is no charge. Medicare Part A covers the hospital. Medicare Part B is for doctor and outpatient procedures and that is generally $104.90 per month currently. With a Medicare supplement—let’s say a plan F—you will pay around $100-$140 when you turn 65 depending on male or female and location (Omaha, Lincoln, Council Bluffs). Add in a Part D prescription drug plan. It is possible to come in around $250 per month in total for your Medicare health coverage. With a plan F, there will be no deductibles, co-pays, or co-insurance. Incredible Cadillac health insurance for approximately $250 per month. Much better than a group plan or an individual plan on the ACA (Affordable Care Act) exchange that costs $1,000+ per month which also includes deductibles, co-pays, and co-insurance.
What does Medicare cost? For most people, you paid for Medicare Part A during the working years, so there is no charge. Medicare Part A covers the hospital. Medicare Part B is for doctor and outpatient procedures and that is generally $104.90 per month currently. With a Medicare supplement—let’s say a plan F—you will pay around $100-$140 when you turn 65 depending on male or female and location (Omaha, Lincoln, Council Bluffs). Add in a Part D prescription drug plan. It is possible to come in around $250 per month in total for your Medicare health coverage. With a plan F, there will be no deductibles, co-pays, or co-insurance. Incredible Cadillac health insurance for approximately $250 per month. Much better than a group plan or an individual plan on the ACA (Affordable Care Act) exchange that costs $1,000+ per month which also includes deductibles, co-pays, and co-insurance.
Medicare is a bargain! Medicare is something that you should be excited to become a part of when you turn 65. I am 53 as of the writing of this blog. I purchase my own insurance on the exchange as a self-employed individual. I would happily pay triple what Medicare beneficiaries pay for that same coverage, and it would still be a bargain for me.
 Most people show up at the steps of Medicare without any idea about how to buy Medigap insurance. If they have health insurance company A at their work, they call up health insurance company A and buy their Medigap insurance from company A. They don’t shop, and most pay more without getting more.
Most people show up at the steps of Medicare without any idea about how to buy Medigap insurance. If they have health insurance company A at their work, they call up health insurance company A and buy their Medigap insurance from company A. They don’t shop, and most pay more without getting more.
Amateur Or Professional?
A few years ago, a friend of mine told me that he was going to finish off his basement himself. His wife wanted it done because she was going to host her large family for Thanksgiving that year. Tom thought he could save some money by doing it himself.
himself.
He figured out a design, went to the hardware store, and bought some lumber. It sat there for several months because he got busy with coaching the kids, work, and other projects. His wife got on him because there was a deadline. He started the project, but because he wasn’t an experienced carpenter, he made a few mistakes. The mistakes started adding up.
Mistakes are expensive. The deadline was looming. Finally, he called in a professional. The basement was done in six weeks, just in time for Thanksgiving. He also realized that the basement was much nicer than what he could have done.
What does this have to do with how to buy Medigap Insurance?
How Do You Find The Lowest Price?
A true insurance professional will show you how to buy Medigap insurance at the lowest cost for the coverage you want. He will have the knowledge and experience to better serve you than doing Medigap insurance yourself, visiting with a friend of a friend who does Medigap insurance part-time, or talking to someone in a call center thousands of miles away.
The benefits of working with an experienced and independent local Medigap insurance professional are that he or she understands the laws and regulations around Medicare in that state and county. The Medicare Handbook is over 150 pages. It takes a while to absorb all the regulations, and that is just from Medicare. Each insurance company has its underwriting guidelines, policies, and procedures. In other words, buying Medigap insurance is complicated.
And all of these organizations are run by humans, and humans make mistakes—lots of mistakes. Have you ever had an insurance company make a mistake that affected you? I’ve seen a few, and an experienced Medigap insurance agent can quickly and easily help you resolve snags that inevitably will arise when you’re trying to figure out how to buy Medigap insurance.
How Do You Buy Medigap Insurance With So Many Choices?
Showing you how to buy Medigap insurance means shopping for Medicare supplements and plans for you. In Nebraska or Iowa, there are over 30+ insurance companies offering hundreds of supplements, 20 Medicare Part C Advantage plans, and 28 Medicare Part D prescription drug plans, which all interact with Medigap insurance.
That is a tremendous amount of information, and prices and information are not easily available to persons not licensed and appointed with Medigap insurance companies. A truly independent agent will be able to show you all the plans and pricing, not just one company with a few plans or a handful of cherry-picked companies. Using sophisticated software, he or she can line up the Medigap insurance plans in your area down to the zip code, showing you how to buy Medigap insurance.
A Plan G is a Plan G
A dirty little secret that most people do not know is all the Medigap insurance plans are the same. By law and regulation, the plans are exactly the same. 
“It’s important to compare Medigap policies since the costs can vary between insurance companies for exactly the same coverage . . . .” The Official U.S. Medicare Handbook: Medicare & You
A Plan G is a Plan G is a Plan G. The only difference is the price. An independent Medicare insurance broker should be able to line up all the Plan G’s and Plan N’s in a row from the least expensive to the most for you to see. How to buy Medigap insurance should be straightforward.
Lowest Price vs. Biggest Brand
While brands are not unimportant, saving money is more important. Some companies trade on their name. You pay more, but the Medigap insurance you buy does not cover anymore, pay any faster, or do anything extra.
There are other things to consider when you think about how to buy Medigap insurance. You will hopefully be using Medicare for twenty or thirty years. Picking a Medicare plan is not like getting a tattoo. It is not a one-and-done thing. Each year Medicare makes changes in rules. Medigap insurance policies go up in price because of age or rate increases. The insurance companies are constantly adjusting plans based upon Medicare, markets, inflation, pharmaceutical companies, etc.
Medigap Age & Rate Increases
How to buy Medigap insurance should also consider the history of age increases to the policy and rate increases. For an insurance company to stay alive, not to mention be profitable, it must be able to adjust its prices. The two ways an insurance company adjusts are through age and rate increases. An independent Medicare insurance broker should be able to show you the age increases. In other words, what will your Medigap insurance policy be at 66, 67, 68, etc.
An independent Medicare insurance agent should also have access to the history of rate increases. Some companies will increase their rates each year a little bit. Other companies will wait a couple of years. Those increases can be quite large. Either way, the price will go up. While past performance does not guarantee the future, you still get an idea of how any insurance company handles prices and inflation. With inflation over 4% this quarter, prices will definitely be going up.
How To Buy Medigap Insurance?
An experienced and independent agent lives in this world and can guide you through the changes to supplements and plans that are most beneficial to you. She can shop Medicare supplements each year and show you how to buy Medigap insurance at the lowest price.
New people are constantly recruited to sell Medigap insurance. Some last a few days, a few months, or a few years. Most do not last at all. The Medicare rules are confusing and unforgiving. Insurance companies follow strict underwriting guidelines and are constantly changing prices. Do you really want to do it yourself or entrust yourself to an amateur?
A Professional Will Show You How to Buy Medigap Insurance
The insurance companies will not give you a discount for going direct. When you do that—and the insurance companies love that—your agent is now whoever answers the 800-number you call. You will speak to a different person each time. That person may be in the insurance industry for two days, two months, or two years. You’ll never know. Or would you rather have an experienced and independent local insurance professional who will be your advocate for the next twenty or thirty years, to help you learn how to buy Medigap insurance? He can show you how to buy Medigap insurance at the best price for you.
for two days, two months, or two years. You’ll never know. Or would you rather have an experienced and independent local insurance professional who will be your advocate for the next twenty or thirty years, to help you learn how to buy Medigap insurance? He can show you how to buy Medigap insurance at the best price for you.