Original MedicareCategory:
Medicare Changes Part B Deductible
Medicare changes came out in December. The Medicare changes Part B deductible was an increase. The Medicare Part B deductible for 2016 was $166. The 2017 Part B deductible is $183. While the $17 increase is small in dollar terms, it was a 10% increase. That’s big!
 Part B Deductible
Part B Deductible
What is the Medicare Part B deductible? Medicare Part A and Part B have various deductibles and co-insurance costs that you pay. While Medicare covers the majority of medical cost, you have some significant responsibility, especially if there are frequent and/or high dollar medical need. Part B covers doctors visits and outpatient procedures, which is everything other than the hospital. Medicare will cover 80% of those costs. Your portion is 20%, but before the 20% starts, you have an annual deductible. The key to the Part B deductible is that it is an annual deductible. You pay the Part B deductible only once per year, which is different from the Part A hospital deductible.
Plan G Vs. Plan F
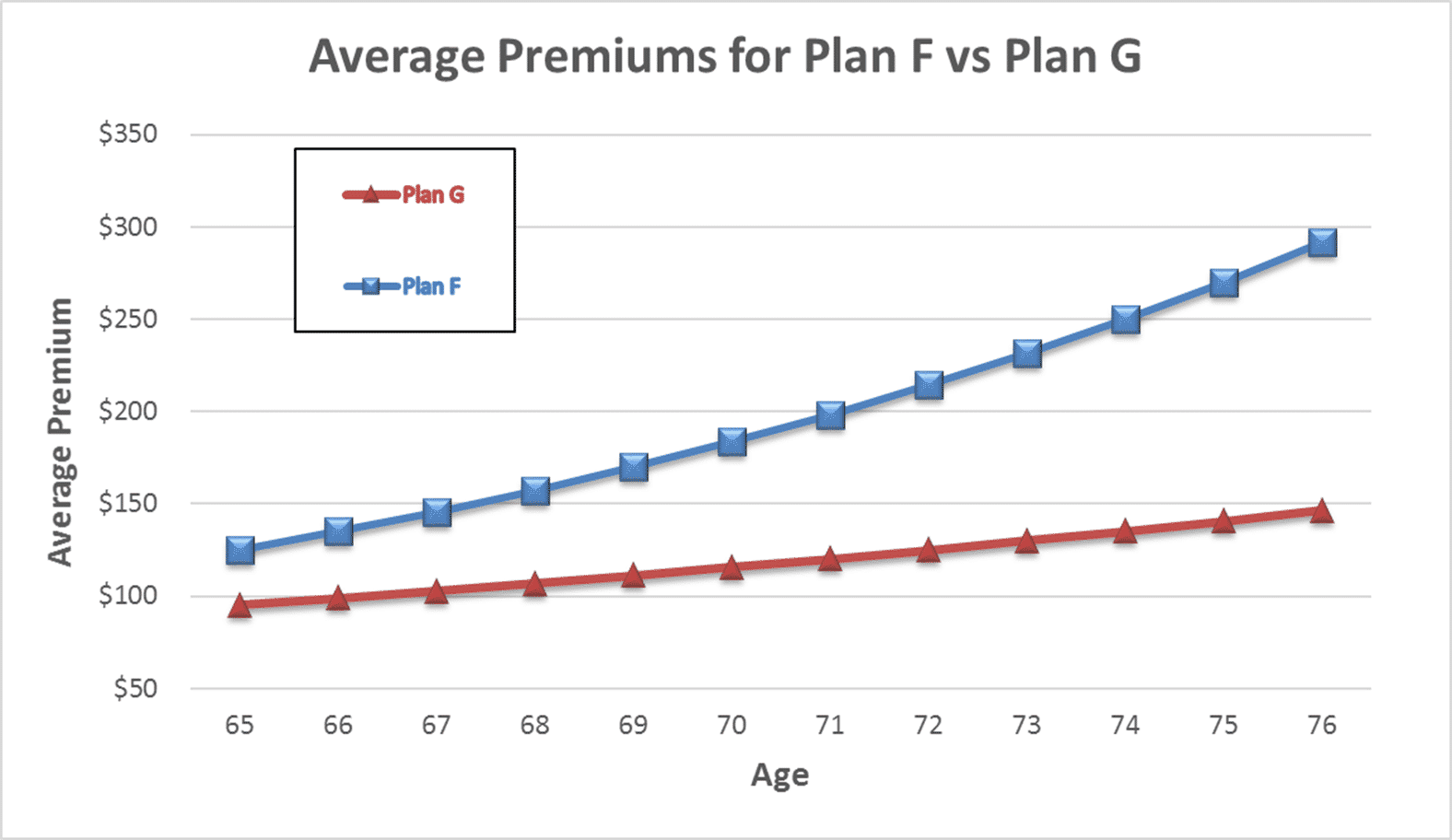 Medicare Supplement Plan G is becoming the most popular supplement plan available. Plan G covers all the Medicare Part A deductibles and Part B co-insurance EXCEPT the Medicare Part B deductible. You pay that directly to the provider after the Medicare discount. Once that is satisfied for the year, you pay nothing else out of pocket.
Medicare Supplement Plan G is becoming the most popular supplement plan available. Plan G covers all the Medicare Part A deductibles and Part B co-insurance EXCEPT the Medicare Part B deductible. You pay that directly to the provider after the Medicare discount. Once that is satisfied for the year, you pay nothing else out of pocket.
You may ask, ‘why don’t I do Plan F where the Part B deductible is also covered?’ If you were on a Plan F, your monthly premium would include the cost of the Part B premium and the increase. You also would pay a substantial fee to the insurance company for them to write the check for $183 for you. By being on Plan G as opposed to Plan F, you avoid the sizeable annual increase and the additional fee for paying the Part B deductible.
While the Medicare changes Part B deductible was not large in dollar terms, the reality is the cost of Medicare will continue to rise along with all medical costs. It is important to have an agent who can help you understand your plan and find the plan that best fits your needs at the lowest cost. Give us a call at 402-614-3389 for a free evaluation.
Medicare Changes Part A Deductible
Medicare changes for 2017 came out in December. One of the changes was for Medicare Part A. Part A is the hospital side of Medicare. It does not cost anything because you paid the Medicare Part A premium during your working years. It was part of your payroll taxes. The premium is zero if you have enough quarters of work and paid in to Medicare; however, Medicare Part A has a deductible. The deductible was $1,288 for 2016. The Part A deductible for 2017 is $1,316.
Remember the Medicare Part A deductible is for each event within a 60 day period. If you revisit the hospital 61 days later OR there is a different and separate event resulting in admittance to the hospital, you pay the $1,316 again.
 Increases Passed On To You
Increases Passed On To You
The significance of the increased Part A deductible will be an increase in the cost of your Medicare Supplement. Most Medicare supplements cover the Part A deductible as many times as it may occur in a given year. Because the insurance company will now be on for more deductible, it will have to offset that expense and risk with higher premiums. Your premium may not increase significantly, but it does cost the insurance company more. Consequently it will ultimately cost you more.
Medicare Advantage Is Different
 For those on Medicare Advantage plans, you are not directly effected. Your hospital co-pays, as well as the other co-pays, are determined by your individual plan. They are already set for 2017. Any increases may result in increases in hospital co-pays down the line because, like supplements, someone needs to pay for the additional expense. The actual co-pay is determined by your Medicare Advantage plan, and they are now set for 2017. Check the changes to your Medicare Advantage plan for 2017. You received your notification of changes in October. If you cannot find it, call the customer service phone number on the back of your card. They will send you a new statement of understanding with all the 2017 co-pays, deductibles, and co-insurance.
For those on Medicare Advantage plans, you are not directly effected. Your hospital co-pays, as well as the other co-pays, are determined by your individual plan. They are already set for 2017. Any increases may result in increases in hospital co-pays down the line because, like supplements, someone needs to pay for the additional expense. The actual co-pay is determined by your Medicare Advantage plan, and they are now set for 2017. Check the changes to your Medicare Advantage plan for 2017. You received your notification of changes in October. If you cannot find it, call the customer service phone number on the back of your card. They will send you a new statement of understanding with all the 2017 co-pays, deductibles, and co-insurance.
Consult with your agent or give us a call to see how any changes to Medicare may affect your situation.
 Medicare Part B
Medicare Part B
Medicare changes almost every year. Medicare changes for 2017 are significant. The Medicare Part B monthly premium is the change that hits people first. For Medicare beneficiaries who were on Medicare before 2016, the increase will be from $104.90 to $109 per month. For those who began Medicare Part B in 2016, the premium will move from $121.80 to $134. There are some minor variations on these numbers out there. Eventually Medicare will catch everyone up to the same amount. I am getting a lot of calls as clients see the higher premium. For those with annual individual incomes above $85,000 and joint incomes above $170,000, the increases are much larger.
Part B Premium Increase
The reason for the increase is the rising cost of Medicare. Fewer persons are working in relationship to the number of new beneficiaries going on Medicare. The baby boomer population turns 65 at a rate of 10,000 per day in our country. The cost of health care also consistently grows at a rate well above inflation. The CPI (Consumer Price Index) is currently about 2%. It is safe to say that Medicare Part B premiums will continue to rise in coming years.
 Protection Again Medicare Changes
Protection Again Medicare Changes
Medicare Part B premium is just one of the costs that are going up. Other deductibles, co-insurance, and co-pays are increasing as well. More and more of the burden of health care is being placed upon consumers, so it makes it even more critical that you select the plan that best fits your needs and budget each and every year. It may make sense to take on some deductibles, co-pays, and/or co-insurance so that the monthly premium is not so burdensome, especially if your monthly income is limited. Medical emergencies do not occur regularly, but premiums do. You must pay them every month. One of the most common calls I get is ‘how do I reduce my monthly health care expenses?’
What is Medicare? A basic question. Or rather, why should anyone care about Medicare? The reason people should care is that most bankruptcies are medical bankruptcies. In other words, if you wish to protect your retirement nest egg from bill collectors, Medicare is important to know about. There are few things that are more disturbing than a pile of medical bills sitting on the kitchen table. The golden years could be tarnished with worrying about actual or potential medical expenses. Medicare–if implemented proper–will protect you from a potential catastrophe. It is critical for people entering into retirement to understand what is Medicare.
What is Medicare?
 Medicare is a Federal health insurance program for people who are 65 and older (or on Social Security disability). It began in 1965 when President Johnson signed it into law. It was designed to provide medical covered to the elderly at a reasonable price. In 1965, few people had health coverage once they stopped working. As a result, many seniors fell into poverty because of burdensome medical expenses. Medicare was a solution to a national problem.
Medicare is a Federal health insurance program for people who are 65 and older (or on Social Security disability). It began in 1965 when President Johnson signed it into law. It was designed to provide medical covered to the elderly at a reasonable price. In 1965, few people had health coverage once they stopped working. As a result, many seniors fell into poverty because of burdensome medical expenses. Medicare was a solution to a national problem.
Medicare Part A
Medicare is divided into two parts: Medicare Part A and Medicare Part B. Medicare Part A has everything to do with the hospital. It doesn’t cost anything because you paid for it during your working years. It was one of the deductions in your payroll taxes. Medicare Part A covers a 100% of the medical expenses incurred in the hospital, but there is deductible that many people are not aware of. The Medicare Part A deductible is currently $1,288. This is NOT an annual deductible. It is a deductible per benefit period, and a benefit period is 60 days. So each event has a deductible, and the time for the event is 60 days. In other words, you could have multiple events and pay multiple deductibles because the event is not limited to just a 60 day period. Each new event, even if it overlaps with another event, has its own 60 day timeline. While rare, it could happen, and probably more importantly, you could pay the Part A $1,288 deductible more than once in any given year.
Medicare Part B
Medicare Part B, however, does cost something. For most people going on Medicare and Social Security in 2016, the Medicare Part B premium is $121.80 per month. It is generally taken out of your Social Security check. Medicare Part B covers doctors’ visits and outpatient procedures, such as X-rays, blood work, emergency room visits, etc. Medicare Part B covers 80% of the cost. Your portion is 20%. The 20% coinsurance, however, is unusual. There is no cap. There is no maximum out-of-pocket. Most group plans you were ever on probably had a maximum out-of-pocket. It may have been $1,000, $2,000, even $10,000, but at some point, you stopped paying and the insurance company covered everything. Medicare Part B does not have that, so 20% of a big number will be a big number. You keep paying your 20% coinsurance as long as the bills come in.
These are the basic building blocks to what is Medicare. You must understand Medicare, Medicare Part A, and Medicare Part B to understand the rest that follows. In the next blogs and videos, we will cover how to get Medicare, how to cover the Part A deductible, and how to fill the unlimited 20% gap in Part B coverage.
More Than Medicare Supplement Plans
I help people sign up for Medicare Part A and Medicare Part B. We go to Medicare.gov and run their medications. I check to make sure their doctors and hospitals are in network for the Medicare Advantage plans. I explain their Medicare eligibility and show All the Medicare supplement plans, Medicare Advantage Plans, and Medicare Part D Plans, but there is much more to being an independent insurance agent who offers Medicare insurance. It is about a long term relationship with my clients. It is more than Medicare supplement plans.
Losing a Medicare Client
I recently lost a couple of clients. They passed away suddenly. I happened to have spoken with one of them a few days before her passing. She had called about some photos she had seem on my personal Facebook page. It is painful when a client dies because I get connect with my clients, especially over time.
More Than Apply for Medicare
The recent loss also reminded me of the nature of my relationship with my Medicare clients. It is a relationship that is meant to last over time. It is more than helping them apply for Medicare. I tell my clients when I enroll them that this is a relationship until “Death do us part.” I will be checking in on them every six months to make sure their plan is working well. I check in especially during Open Enrollment Period when beneficiaries may make changes to their plans. I want to make sure that clients have the best possible plan that fits their needs at the best possible price because we know three things for certain. Medicare will change, the Medicare plans will change, and their needs will change. I want to be on top of those changes for them.
If you want someone who will take care of your Medicare needs over the years, give us a call 402-614-3389.
Delay Medicare Enrollment
Many people work past 65. They continue on with them employer group coverage. They delay Medicare enrollment. At 66+, they wonder what to do about Medicare.
How to Enroll after 65
Here is what to do. Go to Medicare.gov. Click on “Forms, Help, Resources” on the top right. Then click on “Medicare Forms” on the left middle. You will see the enrollment forms in the middle of the page in PDF form. There are two forms: one to enroll in Medicare Part B and a second for your employer to sign off on your coverage. You fill out the enrollment in Part B. Give the second form to your employer. Your employer will verify that you have had health coverage as good as Medicare since you turned 65. They will sign the form. It is important for you to write in the date that you wish your Medicare Part B to start. Give yourself enough time to find a Medicare plan and prescription drug plan. (There are much shorter and restrictive time limits when you have delayed Medicare Part B enrollment.) Drop the forms in the mail or hand deliver them to the local Social Security office.
Medicare Employer Enrollment Forms
Why do you want to involve your employer with your enrollment in Medicare Part B? If you do not have your employer verify that you had health coverage from the time you could have enrolled in Medicare until the time you did take Part B, Medicare will assume you did not have creditable coverage and will asset a penalty. The penalty is a 10% increase in Part B premium for every year you did not have coverage. That can be significant over time and completely unnecessary. Delay Medicare enrollment at your own risk. Get the form. Your employer is required to verify. The human resource department will know exactly what to do. It is a very simple matter.
At Omaha Insurance Solutions, we help clients who delay Medicare enrollment all the time. We can get this done quickly and easily. Give us a call 402-614-3389. We can email you the forms, walk you through filling them out, and explain what to do.
A distressed prospective client told me that Medicare did not cover mental health treatment. I stammered a bit because the subject had never come up before, and I was surprised. I said that it did. She had read that it only covered a one time welcome visit to Medicare. I then showed her in the Medicare & You Handbook on pages 40 and 59 where it detailed the coverage. There is the welcome to Medicare screening, an annual screening, and complete medical coverage. She was surprised and relieved there was Medicare mental health care.
Seniors Need Mental Health Care
Mental health is a serious problem in society, and it is growing among seniors. The World Health Organization documents how important among seniors this issue is. Depression is under reported, little recognized, and often an untreated illness; but Medicare mental health cares for beneficiaries with mental health concerns, like depression. It probably does it better than most employer plans do.
Medicare Mental Health Part A
Medicare Part A deals with the hospital. The same rules around hospital deductibles and co-insurance apply to psychiatric hospitals as to other hospitals. There is, however, one difference. Medicare only allows a lifetime amount of 190 days for a stand alone psychiatric hospitals.
Medicare Mental Health Part B
Medicare Part B covers psychiatrists, counselors, treatment groups. Again the same 20% co-insurance applies as to any other Part B doctor visit. If you have a long standing relationship with a psychologists before Medicare, you may keep that relationship going after you go on Medicare if the medical professional takes assignment for Medicare.
Medicare Supplements will cover Medicare mental health issues and professionals the same as other fees in accordance with your particular Medicare supplement plan. Medicare Advantage will have the same co-pays for psychiatrists and psychologists as for other specialists.
No need to be stressed or depressed about Medicare mental health. You are covered.
Medicare Quote Honesty
People ask for Medicare quotes from insurance agents and companies, but people really don’t know what they are asking for or what they should be looking for. It’s not your fault. You only enroll in Medicare once in a lifetime, so its hard to be an expert. Here are some tips when you are asking for a Medicare quote.
Medicare Part D Quote
 How do you know that the agent is showing all the Medicare Part D plans? Make sure she is showing you the Part D plans on the Medicare.gov website. There will be a number indicating how many plans are available in your state. When she proceeds to the page with the quote, all the plans will be listed in order of cost to you beginning with the least. Make sure she enters ALL of your medications and they appear on the medication list. That is how you know that you have a real Part D quote.
How do you know that the agent is showing all the Medicare Part D plans? Make sure she is showing you the Part D plans on the Medicare.gov website. There will be a number indicating how many plans are available in your state. When she proceeds to the page with the quote, all the plans will be listed in order of cost to you beginning with the least. Make sure she enters ALL of your medications and they appear on the medication list. That is how you know that you have a real Part D quote.
Medicare Part C Quote
 How do you know that the agent is showing all the Medicare Part C plans? Again there will be a number on the Medicare.gov quoting mechanism indicating the total number of plans in your area. When you proceed to the list, they will be listed in the order of the plan most favorable to you in terms of the medications listed. It may or may not be the best plan when looking at the medical side.
How do you know that the agent is showing all the Medicare Part C plans? Again there will be a number on the Medicare.gov quoting mechanism indicating the total number of plans in your area. When you proceed to the list, they will be listed in the order of the plan most favorable to you in terms of the medications listed. It may or may not be the best plan when looking at the medical side.
Medicare Supplement Quote
How do you know that the agent is showing you all the Medicare supplements? You see the usual companies, like United Health Care, Aetna, and Blue Cross. What you should also see is a ![]() number of lesser known companies. Many of those companies will be the lower cost plans. Some agents don’t include the lower price plans because they get paid less. If you see a number of unfamiliar names, that is good. You are probably seeing a complete list of supplements
number of lesser known companies. Many of those companies will be the lower cost plans. Some agents don’t include the lower price plans because they get paid less. If you see a number of unfamiliar names, that is good. You are probably seeing a complete list of supplements
Call us at Omaha Insurance Solutions 402-614-3389 for a quote. We will show you everything. We are not concerned about selling you one company over another. We are concerned about you getting what is best for you.
The Big Lie
The “Big Lie” is a phrase and idea that Adolph Hitler and then Joseph Goebbels promoted in their propaganda war. They observed that if you told a lie about the opposition, made the lie an outrageous claim, and repeated the claim, people would believe it. This technique existed before the Nazis and will continue on to the end of time. Some politicians and sales people are particularly adept at this technique. Center for Medicare & Medicaid Services (CMS) refer to phenomena such as this as Medicare scare tactics. CMS dictates client and agent interaction and strongly discourages insurance agents and companies from engaging in Medicare scare tactics.
Medicare Scare Tactics
 Some insurance agents who offer Medicare supplements and plans use Medicare scare tactics to promote their themselves and their products. They will make outrageously negative claims about opposing companies, products, or agents. “That company had a 40% rate increase.” “That company uses lower initial rates; then jacks them up when you are older.” Some agents who only offer Medicare supplements will dump on Medicare Advantage plans. “Those co-pays will bankrupt you.” Some agents who offer Medicare Advantage plans exclusively will rip on Medicare supplements. “Why waste your money on premiums when you hardly go to the doctor.” I’ve seen agents falsely accuse another agent of illegal or unethical business practices. “He is not even properly licensed” or “he got himself into trouble.” The more outrageous the accusation, the more it is believed by some.
Some insurance agents who offer Medicare supplements and plans use Medicare scare tactics to promote their themselves and their products. They will make outrageously negative claims about opposing companies, products, or agents. “That company had a 40% rate increase.” “That company uses lower initial rates; then jacks them up when you are older.” Some agents who only offer Medicare supplements will dump on Medicare Advantage plans. “Those co-pays will bankrupt you.” Some agents who offer Medicare Advantage plans exclusively will rip on Medicare supplements. “Why waste your money on premiums when you hardly go to the doctor.” I’ve seen agents falsely accuse another agent of illegal or unethical business practices. “He is not even properly licensed” or “he got himself into trouble.” The more outrageous the accusation, the more it is believed by some.
Counter with Facts
 Facts, however, are stubborn things. To counter Medicare scare tactics, ask them to show you the facts from a reputable third party source. I show my clients the insurance company’s history of rate increases. I show clients BOTH supplement and advantage plans side by side. They make the determination which is better for them. All licensed insurance agents are listed on the insurance department website by all states. You can check them out and see if that person has any complaints. When a person makes accusations, have them produce the evidence.
Facts, however, are stubborn things. To counter Medicare scare tactics, ask them to show you the facts from a reputable third party source. I show my clients the insurance company’s history of rate increases. I show clients BOTH supplement and advantage plans side by side. They make the determination which is better for them. All licensed insurance agents are listed on the insurance department website by all states. You can check them out and see if that person has any complaints. When a person makes accusations, have them produce the evidence.
Scare Tactics are Flashing Signals
Medicare scare tactics, a.k.a., trash talk, is a signal. It is like someone who gossips about a co-worker. You know they will be gossiping about you when you walk away. Agents who talk trash about other companies, agents, agencies, and products don’t really have something better to offer. There is no need to talk someone or something down if you are offering something better. Let the facts speak for themselves. The process of selecting a Medicare solution should be an educational process, not propaganda.
If someone is trying to scare or rush you, they probably don’t want you to really see who they are or what they are offering. Cut through the noise. Brush aside the smoke. Look for the facts. “The Truth will set you free.”
A gentleman called me who was losing his group health coverage from a former employer. He was a retiree from a Fortune 100 company. You would recognize the name of the company immediately. As part of his retirement package, he had a very generous health plan for himself and his wife. He had been on it for decades, but the company could no longer afford to maintain it. They canceled the plan, so my client found himself cast out into the Medigap world at 92 not knowing what to do, and he didn’t realize that he would need a Medigap guarantee issue to be get a plan.
Medigap Guarantee Issue Solution
When you are a Medicare beneficiary and you loss group coverage, you have what is called a guarantee issue period. It is a very limited opportunity that has an exasperation date on it. It is an incredibly important guarantee for those who have pre-existing conditions.
What is Medigap Guarantee Issue?
What is guarantee issue for a Medigap policy? How does it work? What should you do to make sure you don’t miss out? Guarantee issue for a Medigap policy applies to a number of situations. I will just speak to one—when you involuntarily lose your group health coverage while on Medicare Part A & B. Guarantee issue means that an insurance company must offer you a Medigap plan—usually plans A, B, C, & F—without asking health questions. They must sell it to you no matter your health condition. For those with pre-existing conditions that would exclude them, this is a treasure. (Each state may handle guarantee issue situations somewhat differently, but this is the general concept.)
 How Does Medigap Guarantee Issue Work?
How Does Medigap Guarantee Issue Work?
How does guarantee issue work for a Medigap policy when you have involuntarily lost your group health coverage? The company that is ending group health coverage will usually give you sufficient time to find other coverage. You are able to purchase a supplement as early as 90 days ahead of time. After coverage has ended, you usually only have 63 days to find coverage without going through underwriting. If you miss that time frame and you have a serious health issue, you will not find a Medigap policy. You will only have Medicare.
What Should You Do to Get Your Medigap Guarantee Issue?
What should you do if you are losing your group plan that covers your Medicare deductibles and coinsurance? First get educated about Medicare. Second get a quote and start looking for a Medigap plan. Third see if you can pass underwriting so you are not restricted to the more expensive plans, but please don’t doddle. There is a clock ticking in terms of your guaranteed issue period.
To summarize, you have a special opportunity to get a Medigap plan when you lose your group plan. The special opportunity is that you do not have to answer health questions for a defined period and the insurance company has to sell you a plan. You need to be aware of the rules and follow them so you do not miss out. Still try underwriting so you have more options, but you have the guarantee provision to fall back on. There are rules and time limits around guaranteed issues. Make sure you fully understand these rules and the ramifications. Call to find out the facts so you don’t miss out. 402-614-3389 OmahaInsuranceSolutions.com







