Medicare 2021 Changes to Know About
 Every year there are changes to Medicare. The changes are usually not as drastic as the television commercials would lead you to believe. The purpose of the advertisements is to stimulate fear, uncertainty, and greed. They hit it hard to motivate you to call the 800-number. They will claim to offer a free objective evaluation. I find their objective evaluation inevitably ends with you changing to their plan. Know about Medicare 2021 changes before they flip you.
Every year there are changes to Medicare. The changes are usually not as drastic as the television commercials would lead you to believe. The purpose of the advertisements is to stimulate fear, uncertainty, and greed. They hit it hard to motivate you to call the 800-number. They will claim to offer a free objective evaluation. I find their objective evaluation inevitably ends with you changing to their plan. Know about Medicare 2021 changes before they flip you.
Unique One-Time Medicare 2021 Changes
My grandmother used to say, ‘live long enough, and you will see everything.’ The changes this year are unique because of the pandemic. COVID tests will have no co-pays. The vaccine is free. The federal government wants to overcome the virus, so Medicare is reflecting that public health policy.
Many Medicare plans had already offering telehealth options. With the pandemic, insurance companies now hardwire their plans with these options–most with zero co-pays.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) changes began in 2015. CMS implemented the changes slowly over the years so Medicare, the insurance companies, and beneficiaries could more easily adjust. Starting in 2020, those turning 65 did not have the opportunity to purchase the Medigap F or C plan. Medicare fazed out those plans with plan G being the principal plan with the most comprehensive coverage. They grandfathered in those 65 and over before 2020. They can still own and purchase plan Fs and C’s.
Medicare Part B Premium in 2021
The most significant Medicare change to know about in 2021 for most people is the Part B premium. This year it will increase from $145.60 to $148.50 per month per person, which is a $2.90 increase. Each year the premium amount is a hard-fought debate in Congress. Usually, Congress threatens to raise it much more. Constituents call in, and advocacy groups lobby, so the price usually goes down.
Part B Deductible in 2021
Medicare Part B consists of many different services. It has its own deductible, which is separate and distinct from the Part A deductible. The deductible increased from $198 in 2020 to $203 in 2021, only $5. The deductible is a flat amount. The consumer pays the deductible before the 20% coinsurance starts. For plan G, the Part B deductible is the only payment, aside from the monthly premium. The Medigap policy fills the remaining gaps in Part A and Part B coverage.
COLA 2021
Social Security and Supplemental Security Income (SSI) benefits for approximately 70 million Americans will increase 1.3 percent in 2021. The 1.3 percent cost-of-living adjustment (COLA) will begin with benefits payable to more than 64 million Social Security beneficiaries in January 2021. The Social Security COLA increase should not be less than the Medicare Part B premium increase. There are exceptions around this. If you are receiving Social Security benefits, you will be held harmless on the increase, but those who do not take Social Security benefits will pay the increase.
Medicare 2021 Changes for Part A
Medicare Part A covers inpatient hospitals, skilled nursing facilities, and some home health care services. About 99 percent of Medicare beneficiaries do not pay a Part A premium since they have at least 40 quarters of Medicare-covered employment. The Medicare Part A inpatient deductible that beneficiaries will pay when admitted to the hospital is $1,484 in 2021, increasing $76 from $1,408 in 2020.
Part D Changes in 2021 (Senior Savings Model)
The Senior Savings Model is an experiment in modeling that tests the impact of offering beneficiaries an increased choice of enhanced alternative Part D plan options that offer lower out-of-pocket costs for insulin. One in every three Medicare beneficiaries has diabetes, and over 3.3 million Medicare beneficiaries use one or more of the common forms of insulin. For some of these beneficiaries, access to insulin can be a critical component of their medical management, with gaps in access increasing the risk of serious complications, ranging from vision loss to kidney failure to foot ulcers (potentially requiring amputation) to heart attacks.
Unfortunately, sometimes the cost of insulin can be a barrier to appropriate medical management of diabetes. CMS’s designed Senior Savings Model for Part D plans to address President Trump’s promise to lower prescription drug costs. The model provides Medicare patients with new choices of Part D plans that offer insulin at an affordable and predictable cost. A one-month supply of a broad set of plan-formulary insulins costs will be no more than $35 each.
Medicare changes to know in 2021 are your drugs listed in the formulary. Part D premiums for 2021 will probably rise an average of 9%. The average stand-alone Part D premium is $41 in 2021. The premiums range from $7 a month for the SilverScript SmartRx plan to a high of $89 for the AARP MedicareRx Preferred plan.

Part D Deductible 2021
The Part D drug deductible went up from $435 to $445 on most plans. That is the max deductible CMS allows insurance companies to set the deductible. They can set it lower, though few plans did this year, and for those plans with zero deductible or a lower deductible, the cost is offset by either higher monthly premiums or co-pays or both.
Most of the time, that deductible is only applicable to tiers 3, 4 & 5 medications.
The first of the year is the time when I get the distressed phone calls because people must meet their deductibles. Many forget the deductible starts over again in January, and they are shocked when they show up at the pharmacy counter. I have to remind clients they need to meet the deductible first to get to the lower copay.
Medicare Advantage Changes in 2021
In the nine years, I have offered Medicare Advantage plans, I have seen the number and especially the quality of the plans increase significantly. Nationally more Medicare Advantage plans are offered now than ever before. In Nebraska and Iowa, I have seen the number of counties offering quality plans explode.
There are now over 4,800 Medicare Advantage plans, an increase of 76% over 2017. The average person will choose from 33 plans offered by eight different insurance companies, with some areas having as many as 60 different plans.
Besides, the number of Special Needs Plans (SNP) also increased to nearly 1,000 in 2021, a sizable jump. The increase in SNP means more people have access to low-cost plans with extra benefits to manage chronic conditions and diseases.
Medicare Advantage Premiums in 2021
Average Medicare Advantage premiums dropped for the fourth consecutive year to $21 in 2021, down from $25 in 2020. Nearly 90% of all Medicare Advantage plans include Part D prescription drug coverage.
Of note, the Medicare Advantage out-of-pocket maximum will increase to $7,550 in 2021, up significantly from $6,700 in 2020. However, the vast majority of insurance companies set their out-of-pocket max well below the government limit. In 2020, the average Medicare Advantage out-of-pocket maximum was $4,900.
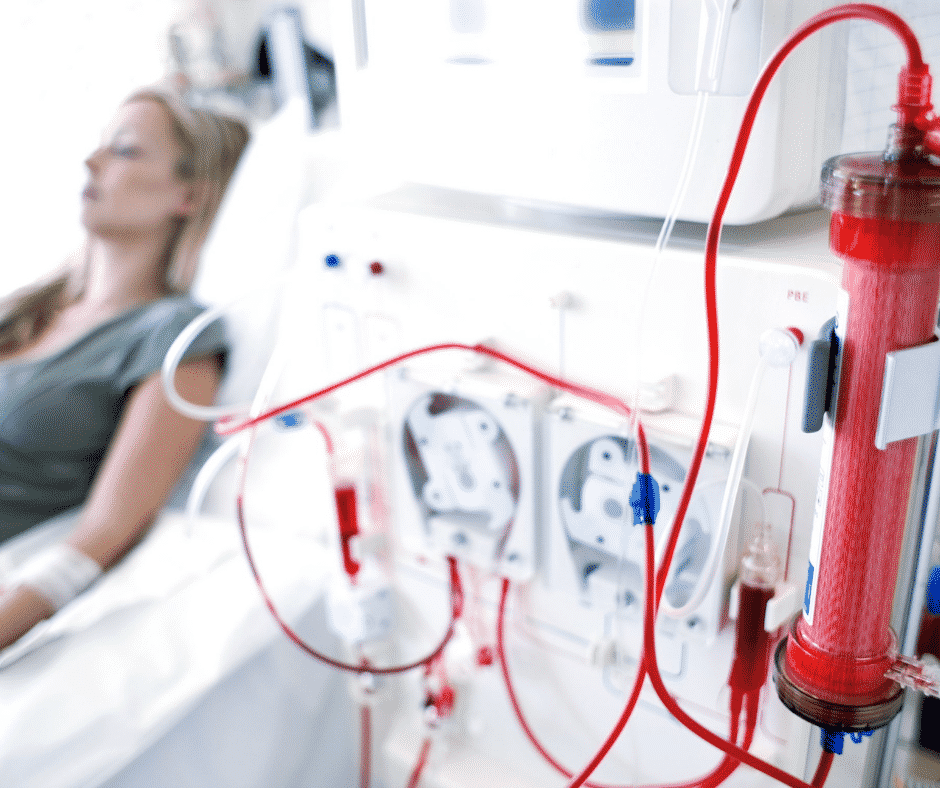 Medicare Advantage and ESRD
Medicare Advantage and ESRD
The most heartening plan change for Medicare Advantage is ESRD (End-Stage Renal Disease). When I first started, the only pre-existing condition that excluded me from enrolling someone in a Medicare Advantage plan was ESRD. While I didn’t have that situation very often, it was sad when I couldn’t offer Part C to clients.
ESRD is one of the health issues that almost always automatically makes you Medicare eligible. Still, if you are younger than 65 in Nebraska and Iowa, you are not eligible for a Medicare supplement. The dialysis falls under the unlimited 20% coinsurance of Part B. The cost can be incredible. Even for those on Medicare Advantage, beneficiaries can easily hit the maximum out of pocket.
At least now those with ESRD can get on a Medicare Advantage plan and limit their out-of-pocket costs.
There’s good news for people with ESRD in 2021. In the past, those with ESRD could not join Medicare Advantage unless there was an ESRD Special Needs Plan available. However, new rules grant guaranteed issue rights to people with ESRD for any Medicare Advantage plan offered in their service area.
Access to Medicare Advantage when you have ESRD is massive. Long-standing rules allowed Medigap companies to deny coverage to people with ESRD outside their Medigap Open Enrollment Period. Even many states that enacted laws forcing insurers to offer Medigap to people under age 65 failed to extend that protection to people with ESRD.
What this means is that, for the first time, people with ESRD have low-cost options to control their health care expenses with a Medicare Advantage plan. If that applies to you, you could have used the 2020 Annual Election Period to shop for a new Medicare Advantage plan.
Provider Compensation
Congress made significant changes to the billing process behind Medicare in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA changes how Medicare rewards providers for qualify over volume inpatient care. It streamlines provider reimbursements through the Merit-Based Incentive Payments System (MIPS) and even grants bonuses for participation in alternative payment models (APMs). Still, the change that gets the most attention is the eliminating of Plan F and C in the Medigap lineup. The plans completely covered the Part A deductibles and Part B co-insurance, so beneficiaries did not have to pay anything aside from their monthly premiums. Congress found the lack of co-pays and deductibles was an incentive for waste and abuse of the Medicare system. Starting in 2021, you could no longer purchase Plan F or C when you turned 65. Those who turned 65 before that period were grandfathered into Plan F and C.
through the Merit-Based Incentive Payments System (MIPS) and even grants bonuses for participation in alternative payment models (APMs). Still, the change that gets the most attention is the eliminating of Plan F and C in the Medigap lineup. The plans completely covered the Part A deductibles and Part B co-insurance, so beneficiaries did not have to pay anything aside from their monthly premiums. Congress found the lack of co-pays and deductibles was an incentive for waste and abuse of the Medicare system. Starting in 2021, you could no longer purchase Plan F or C when you turned 65. Those who turned 65 before that period were grandfathered into Plan F and C.
The other most obvious change was the Medicare number is no longer your Social Security number, but a unique eleven-digit number combining letters and numbers. Everyone’s card should have been replaced by the end of 2019, though I still have some clients who have their old numbers and card. It is a simple matter of calling Medicare for a replacement card.
Medicare makes slight changes over time. Many times the Medicare changes to know about in 2021 do not apply to you, but you, or your agent, still need to be aware of what is going on to always maximize your benefits and avoid disadvantaging yourself temporarily or permanently.