What Is Medicare Hospice?

Medicare pays for hospice, but what is hospice exactly?
Medicare defines hospice as a program of care and support for people who are terminally ill. Terminal illness, as Medicare definites it, is a life expectancy of six months or less. The primary goal of hospice in Medicare is to help terminally ill people live a comfortable life and manage their pain and discomfort. Hospice care is palliative care versus skilled nursing and home health care. Hospice does not cure the patient but rather aids the person in the dying process.
Death & dying is an area most people do not wish to ponder, so there are many misconceptions about Medicare-covered hospice care.
What Medicare Hospice Is Not?
Hospice is not a place. When my mother was terminally ill with ovarian cancer, I was thinking of taking her to a place.
When I was in college in the 80s, I had volunteered in a hospice facility run by the Hawthorne Dominican sisters. The hospice facility was an actual place people went to die. The nuns took care of everything: medical, personal care, food & lodging; and patients stayed there until the end.
That is what I had in mind when the doctors spoke to my family about hospice for our mother. That is not, however, how Medicare thinks of hospice.
Medicare does not pay for a hospice facility that provides room & board unless the care is tied to something like a skilled nursing facility. Medicare does, however, pay for hospice personnel and the medications they administer during hospice.
Where Do You Go For Hospice?
Hospice can be given virtually anywhere. A Medicare beneficiary can receive hospice at a hospital, hospice in a skilled nursing facility, hospice in an assisted living residence, and hospice at home. Medicare will pay for hospice care in assisted living, nursing homes, and other facilities if it is a Medicare-approved facility.
The end of life movement that started in the ’70s sees passing at home as the ideal. Most Medicare patients, when surveyed, prefer hospice in the home. That is where people feel most comfortable, but because of the level of care required, hospice care may have to move to a hospital in the last few days or another location.
Hospice can be given virtually anywhere.
Medicare.gov
What Kind of Illness Makes You Hospice Eligible?
When we think of hospice, we usually think of cancer, but there are other illnesses that result in hospice.
Grandpa Joe was 98. Grandpa had beaten cancer 4 times, lockjaw, and the Second World War. Dying didn’t seem possible. He had always been there, and we grandkids assumed he would always be there. Terminal illness and Grandpa Joe didn’t fit.
When Grandma Hilda announced to the family, Grandpa had congestive heart failure and was going into hospice, it didn’t quite register with us grandkids.
Grandpa Joe seemed the same old Grandpa Joe. When I was home from college, we chatted about the Cornhuskers, baseball, and politics. Nothing seemed to have changed, but there was a procession of nurses and therapists who came in and out of their home.
When Grandma Hilda finally called to tell us Grandpa had passed in his sleep, his death hit me like a sledgehammer.
Grandpa’s passing was hard on everyone, but Medicare providing and paying for hospice lightened the burden, especially for my parents and grandparents.

Who Can Go Into Hospice?
Hospice is also not exclusively for the old. I have a number of clients who are in their twenties and thirties. Not everyone on Medicare is sixty-five and older, though the majority are.
Accidents or illnesses permanently disabled some, and some are terminal. Hospice is for them too.
How Much Is Hospice?
Hospice care is not expensive for those on Medicare. Medicare pays for the vast majority of the hospice costs under Medicare Part A with very little out-of-pocket costs. Medications, some equipment, and nurses are covered.
Like I said earlier, hospice does not usually include custodial care or housekeeping. That can be very costly if the family cannot provide that type of care themselves.
How Do You Get Medicare To Pay For Hospice?
A Medicare beneficiary is eligible for Medicare’s hospice care benefit if she is entitled to Medicare Part A and meets the following conditions.
- The hospice doctor and the person’s regular physician certify that the person is terminally ill with a life expectancy of six months or less if the illness runs its
 expected course.
expected course. - The person accepts palliative care for comfort instead of care to cure her illness.
- The person must sign a statement choosing hospice care instead of other Medicare-covered treatments for her terminal illness and related conditions.
- The care is provided by a Medicare-certified hospice agency.
When these 4 critical are met, Medicare pays for hospice. At any time, a person may choose to exit hospice.
Is Hospice Euthanasia?
Hospice does not accelerate the dying process.
I have had people describe hospice to me as akin to euthanasia where someone actively terminates a life. Hospice is not euthanasia or assisted suicide. You do not intentionally cut short a person’s life. Hospice is about allowing the dying process to take its natural and inevitable course without assistance. Hospice care is about alleviating the suffering and providing comfort while the person dies.

An uncle of mine was a retired Omaha police captain. Uncle Bill had a severe stroke with many complications. He was put on a ventilator.
Uncle Bill was a strong and courageous individual. A vegetative existence was not for him not to mention impoverishing his wife with medical bills. He ordered the ventilator turned off.
Without the ventilator, he would quickly stop breathing. He knew it. The doctors made him as comfortable as possible with heavy sedation. His body fought hard against the loss of breath.
We gathered around his hospital bed. Over the course of a day, he passed peacefully from this life to next surrounded by his loving wife and children.
Hospice Is Up To You
I’ve known many individuals over the years who have gone on hospice for a time. Instead of dying, their health improved, or they resumed a normal life and quit hospice because the decline stopped. You are free to remove yourself from hospice at any time.
Hospice Is Also For The Living
Hospice is the option when all other alternatives have been exhausted. It is the option to bring the highest possible quality of life to a person’s remaining time. The hope is family members will look back on their time and know that everything was done to preserve, prolong, and then peacefully say goodbye.

While you may struggle with the challenge of terminal illness, the end of your life and hospice is as much about your loved ones as it is about you. Watching you suffer and your family’s grief afterward will be their burden. Dying is equally about them. Understanding that there is something for them as well as you in a scary time can give you all hope that the last great challenge in life will be a little less daunting.
While hospice ends with a patient’s death, family grief counseling can continue for up to a year. Medicare pays for that hospice care too.
One’s mortality is difficult to face, but the chance you will go on Medicare hospice at the end of your life is more than 50%. That is an extraordinary number, so having confidence Medicare will pay for hospice is critical.
 Medicare Advantage and Home Health Care
Medicare Advantage and Home Health Care
All Medicare Advantage (MA) plans must provide at least the same level of coverage for home health care as does Original Medicare, so Medicare Advantage pays for home health care. However, an MA plan may have different rules, costs, and restrictions on services. For example, depending on a person’s MA plan, it may require him to:
- Obtain care from a home health agency that has contracted with the plan.
- Receive prior authorization or a referral before receiving home health care.
- Pay a copayment for home health care.
Coverage of Non-Skilled Care and Other In-Home Support Services
Center for Medicare & Medicaid Services (CMS) recently announced that Medicare Advantage plan will be able to cover certain types of home health care related services that were not previously able to be offered, beginning in 2019. This will be possible because CMS has expanded the definitional scope of “supplemental benefits” that Medicare Advantage plans can offer. Starting in 2019, insurers can offer additional services to help improve enrollees’ health and quality of life.
Medicare Advantage Can Pay for Home Health Care Supplemental Benefits
Medicare Advantage plans may offer additions benefits not offered by Original Medicare. Previously, CMS did not allow any item or service to qualify as a supplemental benefit. Supplemental benefits were items of “daily maintenance.” In other words, MA plans could not offer items and services that were not directly for medical treatments. The agency has now reinterpreted the requirement for supplemental benefits to include a “primarily health-related” definition as follows:
an item or service that is used to diagnose, prevent, or treat an illness or injury, compensate for physical impairments, act to ameliorate the functional/psychological impact of injuries or health conditions, or reduce avoidable emergency and healthcare utilization
Some Medicare Advantage Supplemental Benefits
Accordingly, this reinterpretation of supplemental benefits will allow Medicare health plans to offer coverage or benefits for the following:
- Adult daycare services are services provided outside the home, such as assistance with activities of daily living (ADLs) and instrumental activities of daily living (IADLs)
- In-home support services are services a personal care attendant provides. She assists disabled or medically needy individuals with activities of daily living, such as eating, bathing, and transferring, and instrumental activities of daily living. These activities may include managing money, preparing meals, and cleaning a house. Services must be performed by individuals licensed to provide personal care services, or in a manner that is otherwise consistent with state requirements.
- Home-based palliative care services Medicare does not cover if life expectancy is more than six months. Palliative care (“comfort care”) is to diminish symptoms of a terminally ill patient.
- Transportation for nonemergency medical services is transportation to obtain Part A, Part B, Part D, and supplemental benefit items and services. The
 transportation must be used to accommodate the enrollee’s health care needs: it cannot be used for nonmedical services, such as groceries or errands.
transportation must be used to accommodate the enrollee’s health care needs: it cannot be used for nonmedical services, such as groceries or errands. - Home safety devices and modifications are safety devices to prevent injuries in the home and/or bathroom. The modifications must be non-structural and non-Medicare covered. This benefit can include home and/or bathroom safety inspection to identify any need for safety devices or modifications.
A physician or licensed medical professional must recommend these home care services.
Medicare’s expansion of MA plan benefits, like adult days care, helps patients remain in their homes as they age rather than being institutionalized, which could also result in lower costs for Medicare and Medicaid.
 The Advantage of Medicare Advantage for Home Health Care
The Advantage of Medicare Advantage for Home Health Care
Medicare Advantage plans may impose different rules, limitations, and costs than Original Medicare, but they must provide at least the same level of home health care benefits.
Starting in 2019, Medicare Advantage plans may offer supplemental benefits that help enrollees with daily maintenance, including transportation for medicare services, in-home support services, and home-based palliative care. Consult the individual MA plan for the details of coverage.
In the Omaha metro area, the MA plans offer some of these benefits. Currently, the plans that do offer a lot of these benefits are the “Dual” or “Special Needs” plans. Those plans are for a person on full Medicaid as well as Medicare or have some special needs because of chronic illness, such as COPD, Diabetes, etc.
In other areas with high population densities, many of the MA plans are much richer with benefits. As it stands in eastern Nebraska and western Iowa, principally Omaha, Lincoln, Bellevue, and Council Bluffs, the supplemental benefits seem to be growing in number and scope each year. A couple of insurance companies recently added transportation to their health plans. More insurance companies are developing Medicare Advantage plans and including this type of home health services.
 Navigating the Complexities: What You Need to Know About Medicare and Home Healthcare Coverage
Navigating the Complexities: What You Need to Know About Medicare and Home Healthcare Coverage
Are you confused about Medicare and home health care coverage? If so, you’re not alone. Navigating the complexities of these topics can be overwhelming. It’s essential to understand your options and ensure you receive the care you need.
Does Medicare pay for home health care services?
This article will delve into the ins and outs of Medicare and home healthcare coverage, providing the information you need to make informed decisions. We’ll explore the different types of Medicare plans and how they relate to home healthcare services, eligibility requirements, coverage limitations, and common misconceptions.
Whether you’re a senior seeking assistance or a caregiver supporting a loved one, understanding how long Medicare pays for home health care is crucial. By the end of this article, you’ll clearly understand what options are available and how to navigate the complex healthcare landscape.
Stay tuned to discover everything you need about Medicare and home healthcare coverage. Don’t let the confusion hold you back from accessing the care you deserve.
Different Types of Medicare Coverage
Medicare is a federal health insurance program that covers people over 65 and those with specific disabilities or chronic conditions. There are several types of Medicare plans, each with benefits and limitations. Knowing how long each Medicare plan pays for health care is critical. 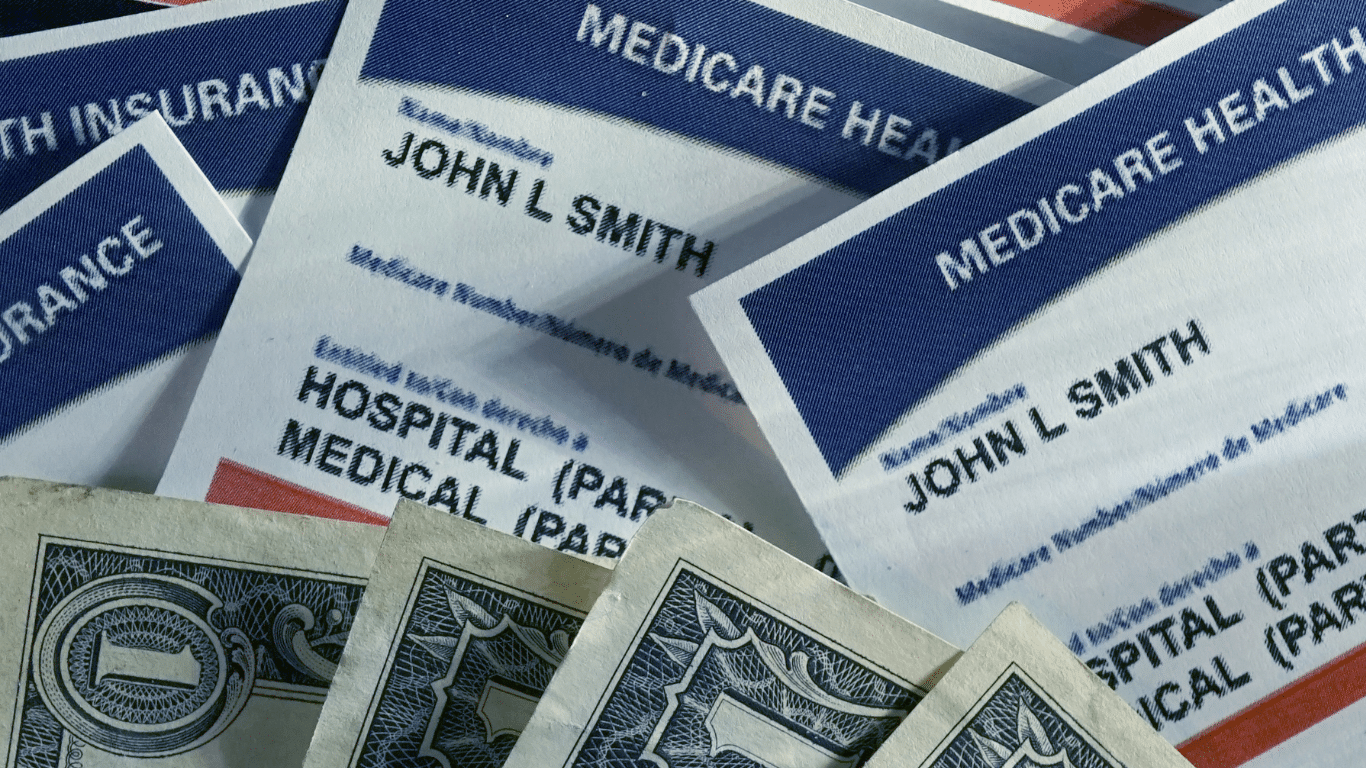
Original Medicare, also known as Medicare Part A and Part B, provides coverage for hospital stays, doctor visits, home healthcare, and some medical equipment. Medicare Part C, also known as Medicare Advantage, is a private insurance option combining Parts A and B, often including additional benefits such as prescription drug coverage and dental care. Both provide home healthcare coverage, but in specific ways unique to the plans.
Medicare Part D provides coverage for prescription drugs, while Medicare Supplement plans, also known as Medigap, help cover the costs of out-of-pocket expenses not covered by Original Medicare.
Understanding the differences between these plans is essential because they approach home health care differently.
 Understanding Home Healthcare Services
Understanding Home Healthcare Services
As the name suggests, home healthcare services provide medical care and support to individuals in their homes. This can include services such as nursing care, physical therapy, and speech-language therapy. Home health care is often a more convenient and cost-effective option than hospital or skilled nursing facility (SNF) care and can provide a higher level of comfort and independence for patients. It is skilled nursing care but provided in the home for those who would not have access to medical care otherwise.
The purpose of home health care is short-term treatment for an illness or injury, such as a stroke or broken hip. It is about getting back your health and independence again.
For the chronically ill and disabled, the goal of home health care is to maintain the highest level of ability and health.
Home healthcare services can be provided by a variety of healthcare professionals, including registered nurses, licensed practical nurses, physical therapists, occupational therapists, and speech-language pathologists. A physician typically orders services, and they are covered by Medicare and/or private insurance.
Home health care is not home care. Home care would be custodial services like housekeeping, bathing, feeding, etc. Medicare does not usually provide those types of personal services, strictly speaking. There are exceptions, however. On occasion, Medicare allows for a temporary home health aide to assist in the healing process.
Some injuries and illnesses may last for a long time. While home health care is a necessary service, the bigger question is: how long does Medicare pay for home healthcare?
Medicare Eligibility for Home Healthcare Coverage
Individuals must meet specific requirements to be eligible for Medicare home healthcare coverage. First, they must be enrolled in Medicare Part A and/or Part B. Both Medicare Part A and Part B provide home healthcare coverage.
Under Part B, a person is eligible for home health care if she is homebound, requires skilled care, and is certified as needing care by a physician. The added benefit is Part B does not require a qualifying hospital stay.
The essential requirements of eligibility and access to Medicare home healthcare services are: homebound, physician certification, and Medicare-certified agency care.
Homebout, in Medicare terms, means that leaving the home requires a considerable and taxing effort. A physician is the gatekeeper of Medicare home healthcare. The physician certifies and/or recertifies a patient for access to home healthcare. Finally, a Medicare-certified agency must provide home healthcare services, not any healthcare provider.
Medicare Part A Coverage
In contrast, Medicare Part A provides home health care coverage in some situations. A hospital or skilled nursing facility stay triggers Part A. If a person has a three-day inpatient stay at a hospital or has a Medicare-covered Skilled Nursing Facility (SNF) stay, Part A will cover up to 100 days of home health care.
Note that a person must still meet the other eligibility requirements to receive home health care, such as needing skilled care, being homebound, and having a doctor certify that such care is necessary.
A person also must receive home health services within 14 days of being discharged from a hospital or SNF. If a person doesn’t meet all of the requirements for Part A coverage but is otherwise eligible for home health care benefits, her care will be financed under Part B.
Medicare Coverage For Home Healthcare Services Amounts
Regardless of whether Part A or Part B covers a person’s care, Medicare will pay:
- The entire approved cost of all covered home health services.
- Eighty percent of the Medicare-approved amount is for durable medical equipment.
Medicare covers a wide range of home health care visits, including skilled nursing care, physical therapy, occupational therapy, speech-language pathology, and medical social services. These services are typically provided part-time or intermittently, depending on the individual’s needs.
Medicare also covers specific durable medical equipment and supplies, such as wheelchairs, hospital beds, and oxygen equipment.
However, coverage limitations and restrictions may apply, and it’s essential to understand what services are covered and how much you may be responsible for paying out of pocket. The agencies providing the equipment and supplies can give details of costs.
 Limitations and restrictions of Medicare coverage for home health care
Limitations and restrictions of Medicare coverage for home health care
While Medicare provides coverage for many home healthcare services, there are limitations and restrictions to be aware of. For example, Medicare typically only covers part-time or intermittent care and may not cover 24-hour or long-term care.
In addition, Medicare may not cover certain services considered custodial care, such as help with bathing, dressing, and eating. Finally, there may be coverage limitations based on the individual’s medical condition. Some coverage is subject to annual or lifetime caps.
Certified Home Health Agency Disclosure of Covered Costs
Before home health care starts, the certified home health agency must tell the person how much Medicare will pay. The agency must also disclose if Medicare does not cover needed items or services. Then tell how much the person will have to pay for them.
For example, charges to a person may be:
- Medical services and supplies that Original Medicare doesn’t cover, such as prescription drugs or routine foot care
- 20 percent of the approved amount for Medicare-covered durable medical equipment such as wheelchairs, walkers, and oxygen equipment
Tips for Navigating Medicare and Home Healthcare Coverage
Navigating the complexities of Medicare and home healthcare coverage can be challenging, but several tips help make the process easier. First, it’s important to understand your needs and choose the Medicare plan that best fits them.
Second, work with your healthcare provider to ensure that a Medicare-certified agency orders and provides home healthcare services.
Finally, read the fine print and understand any coverage limitations or restrictions that may apply. The Medicare-certified agency is well versed in the cover limitations and costs. Be sure to consult with them ahead of time.
Alternative options for home health care coverage
While Medicare provides coverage for many home health care services, alternative options may be available to better meet your needs. For example, private insurance plans may offer more comprehensive coverage for certain services. Medicaid is another route for low-income individuals.
Private Home Health Care Insurance Policies
Home health care insurance is typically a private insurance policy purchased ahead of time to assist Medicare in caring for someone receiving home health care. The policy covers activities of daily living in the home, such as bathing, feeding, transportation, and housekeeping. Like any insurance, these alternative options must be purchased before the health issues arise. Many insurance carriers offer a variety of these types of policies.
In addition, a variety of community-based programs and organizations offer support and assistance to seniors and individuals with disabilities. These programs may include meal delivery, transportation services, and assistance with daily living activities.
 Home Health Agency Advance Beneficiary Notice of Noncoverage
Home Health Agency Advance Beneficiary Notice of Noncoverage
When a certified home health agency believes that Medicare may not pay for some or all of a person’s home health care, it must give the person a written notice called an Advance Beneficiary Notice of Noncoverage (ABN). The ABN might occur, for example, if the home health agency thinks that Medicare will not pay for items or services because:
- The care is not considered medically reasonable and necessary.
- The care is only unskilled, a home health care aide, like help with bathing or dressing.
- The person is not homebound.
- The person does not need skilled care on an intermittent basis.
The ABN must describe the service and/or items that may not be covered and explain why Medicare probably won’t pay. The notice must also include an estimate of the costs for the items and services so that the beneficiary can decide whether to receive the services, understanding that she may have to pay out-of-pocket for such care.
The ABN also gives directions for getting an official decision from Medicare about payment for home health services and supplies and for filing an appeal if Medicare won’t pay.
How Long Does Medicare Pay for Home Health Care?
There is no limit to the length of time that a person can receive home health care services. Once the initial qualifying criteria are met, Medicare will cover home health care as long as it is medically necessary. However, care is limited. There are a maximum number of visits per week and a certain amount of hours per day of care.
When a person first begins receiving home health care, the plan of care will allow for up to 60 days. At the end of this period, the physician must decide whether to recertify the patient for another 60 days. The patient must be recertified at least every 60 days if home health care is to continue.
Medicare does not limit the number of times a physician may recertify a patient. Provided all eligibility requirements continue, he can recertify an unlimited number.
What Happens When Medicare Stops Paying for Home Health Care?
A home health agency must give a beneficiary a written Home Health Change of Care Notice (HHCCN) when the patient’s plan of care changes because the home health agency decides to reduce or stop providing some or all of the home health services or supplies. Or, the patient’s doctor has changed the orders, which may reduce or stop certain home healthcare services or supplies that Medicare covers.
doctor has changed the orders, which may reduce or stop certain home healthcare services or supplies that Medicare covers.
For example, the doctor changes the care plan from five to three days a week. The agency issues an HHCCN. The beneficiary receives a notification in writing of the change.
The HHCCN lists the services or supplies that will be changed and gives the beneficiary instructions on what to do if she disagrees. The home health agency is not required to give a person an HHCCN when a Notice of Medicare Noncoverage is issued.
Notice of Medicare Noncoverage
When a person’s Medicare-covered services end, the home health agency must give the beneficiary a Notice of Medicare Noncoverage (NOMNC). This notice states when services will end as well as how to appeal the decision. The NOMNC also provides information on contacting the Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) to request an expedited appeal.
Once a person decides to appeal and has reached the BFCC-QIO, the home health agency must give the patient a detailed notice explaining why it believes Medicare-covered care should end. The agency should tell the applicable coverage rules and other information about the person’s situation.
A physician must submit a statement of appeal to the BFCC-QIO. It says the patient’s health will be jeopardized if care is discontinued. These factors determine how long Medicare pays for home health care. Knowledge of these rules is vital to maximize benefits and avoid costly mistakes.
Importance of understanding Medicare and home health care coverage
Understanding Medicare and home health care coverage is crucial for seniors and individuals with chronic conditions or disabilities. These programs provide access to essential medical care. They support individuals to maintain their independence and quality of life.
By understanding the different types of Medicare plans, eligibility requirements, coverage limitations, and alternative options, individuals can make informed decisions about their healthcare and ensure they receive the care they need.
Bottomline: Taking Advantage of Medicare and Home Healthcare Benefits
In conclusion, navigating the complexities of Medicare and home healthcare coverage can be challenging, but it’s essential for seniors and individuals with chronic conditions or disabilities. By understanding the different types of Medicare plans, eligibility requirements, coverage

Christopher J. Grimmond
limitations, and alternative options, individuals can make informed decisions about their healthcare and ensure they receive the care they need.
Whether you’re seeking home healthcare services for yourself or a loved one, working with your healthcare provider and understanding the coverage options available is essential. By taking advantage of Medicare and other home healthcare benefits, you can maintain your independence, improve your quality of life, and ensure you receive the care you deserve.
At Omaha Insurance Solutions, we help you understand the many Medicare rules. We navigate you through the forms and get the care you need. Call us at 402-614-3389 to speak with an experienced, licensed insurance agent professional.
 Medicare covers Home Health Care, but the Medicare beneficiary must meet particular criteria, maintain a status of medical need, and follow Medicare regulations and processes to enjoy the benefits.
Medicare covers Home Health Care, but the Medicare beneficiary must meet particular criteria, maintain a status of medical need, and follow Medicare regulations and processes to enjoy the benefits.
Eligibility For Medicare Home Health Care Benefits
- A physician must certify that skilled care is needed and must prescribe the plan of care.
- A participating Medicare-approved home health care organization must provide the care.
- The patient must need at least one of the services: intermittent skilled nursing care, physical therapy, speech-language pathology, and continued occupational therapy.
- The patient must be confined to the home.
Plan of Care
A physician must meet face-to-face with the patient 90 days before the start of home health care or within 30 days after the start of home health care. She must sign and date a certification that the patient needs skilled care and meets all the Medicare eligibility criteria for home health care. As part of the certification, she must determine from the in-person meeting a plan of care.
- A plan of care describes the type of services and care a person will receive for their health concerns. The program will list:
- the variety of services, supplies, and equipment needed.
- the health care professional who will deliver these services
- how often services will be needed
- the beneficiary’s function limitations
- nutritional requirements]
- the results that the physician expects from the treatment
The home health agency is responsible for providing all of the care listed in a person’s plan of care. The agency may do this through its staff or an arrangement with another agency.
The doctor certifies the person as eligible for an initial 60-day benefit period. At the end of the period or before, the doctor may recertify the person, or if the person’s condition has changed, determine the care is no longer needed. Only the doctor can certify the patient or make changes to the plan of care, not the home health agency.
 Medicare-Certified Home Health Care Agency
Medicare-Certified Home Health Care Agency
Medicare will pay for home health care only if a Medicare-certified home health care agency provides it. Medicare approves agencies that meet specific federal health and safety requirements as well as Medicare standards necessary for reimbursement. To ensure that these standards met, Medicare regularly inspects home health agencies. However, Medicare certification does not guarantee a legal warrant of the individuals performing the services.
A Medicare-certified home health agency agrees to:
- be paid by Medicare
- accept only the amount that Medicare approves for its services.
The patient has the right to choose any agency to provide the services as long as they are Medicare certified. The agency is not required to accept the person if it cannot meet that person’s medical needs.
Skilled Care Required But Intermittent
To qualify for Medicare provided home health care, the person needs specialized care. Skilled care means services, such as skilled nursing care, physical therapy, speech therapy, and/or continuing occupational therapy.
The key to determining home health care versus skilled nursing care in a facility is the quantity of care. Home health care must be intermittent. That is, the care must be part-time, meaning less than eight hours each day for up to 21 days–although coverage may be extended in particular circumstances when the need for additional skilled nursing is finite and predictable.
Required Homebound
The homebound criterium does not mean the person is a prisoner in her home. It means leaving is an undue burden. She has trouble leaving home without help because she must use a cane, wheelchair, walker, crutches, or specialized transportation.
It does not mean that person does not leave home on occasion because of important family events, specific medical tests, funerals, or weddings. Even attending adult daycare would not be a violation of being homebound.
Home Health Care May Cover A Health Aide
Home health aide services get a great deal of play. Medicare will cover a health aide for short periods. The aide service must be coupled with home health care  services. Medicare does not cover it exclusively.
services. Medicare does not cover it exclusively.
The home health aide is in support of the healing process with the other skilled nursing professionals. The home health aid does not have a nursing license. For example, a home health aide might help a person with personal care, such as bathing, using the toilet, or dressing–in other words, services that do not require the skills of a licensed nurse.
Other services are help with medications that are self-administered, assistance with activities that are directly supportive of skilled therapy. The aide may help with routine exercises and/or practicing functional communication skills. Where appliable, she may help with regular care of prosthetic and orthotic devices. Medicare will not cover the home health aide if the patient is not receiving skilled care.
Home Health Care Can Cover Social Services
Many injuries and illnesses come with an emotional cost. A patient of my wife recently was hospitalized because his son assaulted him while under the influence of illegal drugs. He was defending his wife, who was likewise being assaulted. The father was hospitalized with broken bones. He is also currently going through chemotherapy treatment and is eighty-six years old.
As you can imagine, the emotional trauma to this couple was extensive and may require counseling and other intervention when the gentleman returns home. Home health care provides these types of services as well.
 Durable Medical Equipment
Durable Medical Equipment
Home health agencies will also help with durable medical equipment. A patient may need a hospital bed, walker, wheelchair, or oxygen. Medicare also covers Medicare supplies, like wound dressings or catheters that are ordered as part of a patient’s care.
If a home health agency doesn’t supply durable medical equipment directly, its staff will typically arrange for a home equipment supplier to bring the items need to the person’s home.
Does Medicare Exclude Some Home Health Care Services?
Medicare does not pay for the following:
- 24-hour-per-day care at home
- meals delivered to the home
- homemaker services like shopping, cleaning, and laundry
- personal care given by home health aides (like bathing, using the toilet, or help in getting dressed)when this is the only care needed.
Does Medicare cover home health care? It certainly does when the patient meets the established criteria. Home health care is a rich source of benefits to beneficiaries that are delivered in a variety of ways and circumstances as needed.
We know what hospitals are. We all have been to a doctor’s office. Many have experienced a relative in a nursing home, but what is home health care?
Home health care is like it sounds. It is the care that takes place in the home. It consists of a wide range of services, like physical therapy, occupational therapy, speech therapy, and nursing care.
The purpose of home health care is short term treatment for an illness or injury, such as a stroke or broken hip. It is about getting the person healthy and independent again. Or, it is for the chronically ill and disabled. The goal is to maintain the highest level of ability and health.
Home health care is not home care. Home care would be services, like housekeeping, bathing, feeding, etc. Medicare does not usually provide those types of personal services, strictly speaking, though there are exceptions at times that allow for a temporary home health aide. It is skilled nursing care provided in the home for those who would not have access otherwise.
Does Medicare Cover It?
Four criteria must be met for Medicare to pay for home health care.
- A physician must certify home health care is necessary.
- The home health care provider must be a Medicare-approved organization.
- The patient must need at least one of the following: skilled nursing care, physical therapy, occupational therapy, or speech therapy.
- The patient must be homebound.
Doctor Certifies Patient For Home Health Care
The doctor must certify a patient needs home health care during an in-person meeting. He signs a certificate certifying that the person meets the Medicare qualification. The doctor lays out a plan of care that care professions implement, and the certification is for 60 days. At the end of the 60 days, or before, he can recertify that patient for an additional 60 days.
The doctor can continue to recertify the patient indefinitely as long as the person qualifies for the medically necessary treatment, and Medicare will continue to cover them.
Home Health Agency Medicare Certified
The home health agency providing the care must be certified by Medicare for the service to be Medicare-covered. In my office building as you come in, a care agency is in the lobby. On the office door, the home health agency lists the various services, and in even bigger letters, it states, “Medicare Certified.”
Medicare certification of a home health agency is an extensive process. Because accreditation is arduous and a source of considerable revenue, home health agencies are very careful about maintaining their certification and advertising their Medicare certification as well. The Omaha metro area has some excellent home health care agencies.
Intermittent Care
Home health care must also be intermittent care. That is, it consists of fewer than seven days a week, or daily care for less than 8 hours each day for up to 21 days. Otherwise, a skilled nursing facility would most likely be recommended for a more intense regimen of care.
Homebound
 The patient must be homebound, which means she cannot leave her home without great difficulty and requires help, such as a wheelchair, walker, crutches, or specialized transportation. It doesn’t mean she can never leave her home for important things, like family events, hairdressing appointments, some doctors’ appointments, but getting regular health services outside the house would be an undue burden.
The patient must be homebound, which means she cannot leave her home without great difficulty and requires help, such as a wheelchair, walker, crutches, or specialized transportation. It doesn’t mean she can never leave her home for important things, like family events, hairdressing appointments, some doctors’ appointments, but getting regular health services outside the house would be an undue burden.
People are living longer. Tremendous advances in technology have enabled seniors to stay out of expensive skilled nursing care. Nowadays, patients may receive very sophisticated treatment at home and do not need to be institutionalized, keeping the cost of treatment lower. It is an important and essential service that Medicare covers.







