Skilled Nursing FacilitiesCategory:
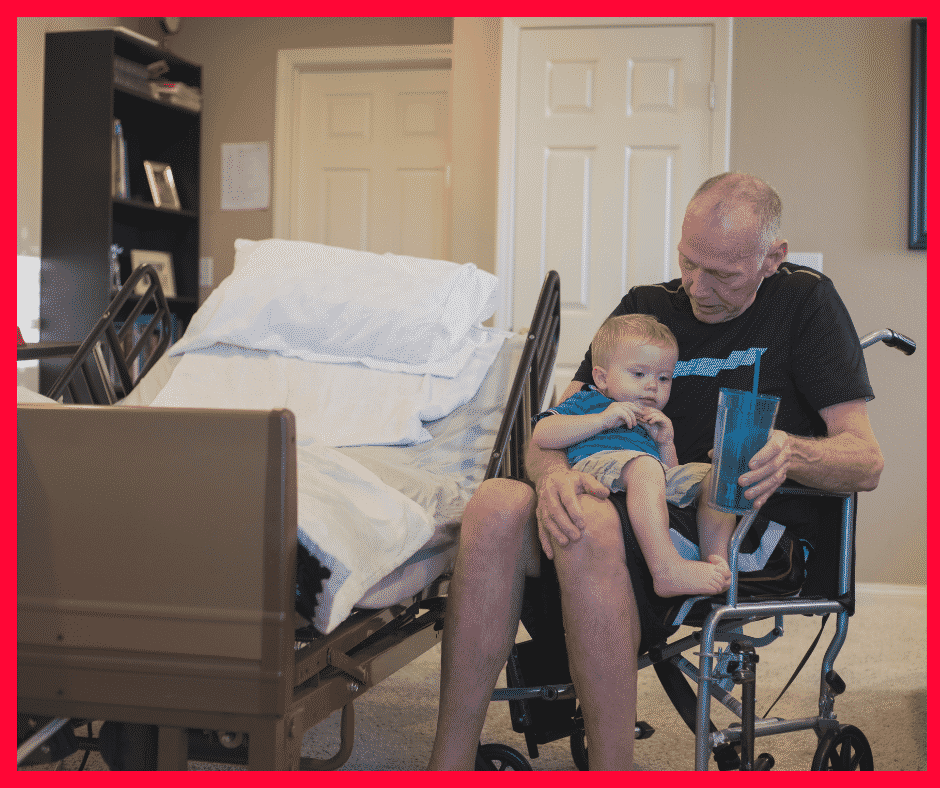
As people age, the value of good health becomes more important than ever. When you had a bad fall in your 40s, it would take a few weeks to recover. Now, a bad fall may result in a hip injury that takes months of recovery, doctor visits, physical therapy, or even surgery. Some must go to skilled nursing facilities to recover. The contrast is stark. Seniors’ health issues increase in frequency and complexity as they age. According to the National Council on Aging, nearly 95% of older adults have at least one chronic condition, and 3 million adults aged 65 or older are treated in emergency rooms due to fall-related injuries every year. So Medicare beneficiaries ask: How long Will Medicare Pay for nursing home care and home health care? 
Navigating the Complexities of Care: Medicare’s Coverage of Long-Term Care, Skilled Nursing Facilities, and Home Health Care
While preventative care is essential–annual physicals, screenings, and regular tests–and “fall-proofing” your home is critical, you must be prepared financially for the costs associated with extensive medical care if and when that occurs. If a health event puts you in a situation requiring special care or costly in-facility admittance, your first question will probably be, “How am I going to pay for this?”
If you are a Medicare recipient, navigating care in a long-term care facility can be complex and confusing. There are so many different types of care – long-term care (LTC), skilled nursing facility (SNF), and home healthcare (HH) – that it’s hard to know how it all works and how much Medicare is willing to pay for each.
My job is to make that journey a whole lot easier. I’ll break down each of these care types and dive into what Medicare will and won’t cover so that you know your options if you’re faced with a health challenge that requires ongoing care.
The Differences: LTC vs. SNF vs. HH
Understanding the different types of care offerings can feel like a full-time job for aging adults. Terms like assisted living facilities, senior living providers, and skilled nursing facilities are often used interchangeably, but the truth is, there are subtle differences in care and what and how much Medicare pays for the different types of “nursing home care.”
The three essential categories of care for seniors are long-term care (LTC), skilled nursing facilities (SNF), and home healthcare (HH). Understanding what each one does and its purpose can be beneficial when it comes time to finding care for your specific situation.
Long Term Care (LTC)
Long-Term Care facilities are the places we think of as “nursing homes.” A person may go to a long-term care facility for several reasons and lengths of stay. Permanent residents generally go to LTC facilities primarily because they can no longer perform the activities of daily living.
The 5 activities of daily living are:
- Feeding
- Dressing
- Personal Hygiene (bathing, brushing teeth, clipping nails, etc.)
- Continence (control of bladder and bowels)
- Toileting
If you struggle with any of the above, a Long-Term Care facility may be the right choice for you.
Staffed with caregivers, such as certified nurse assistants, registered nurses, various types of therapists, and doctors–these facilities focus more on providing meals, custodial care like dressing and feeding, and offering social environments for their patients. While also providing health care, the primary focus is custodial care because residents can no longer perform those functions for themselves, their families cannot care for them, and they cannot afford to provide those services in their own homes economically.
 Skilled Nursing Facility (SNF)
Skilled Nursing Facility (SNF)
Skilled nursing facilities are often in the same physical location as long-term care facilities. The difference comes down to the reason behind your stay. If you need care because of a medical condition – such as a broken hip from a fall, car accident, stroke, or heart attack – then an SNF can provide the medical care you need–intense nursing care, physical therapy, speech pathology. Custodial care, such as feeding or toileting, comes with a stay in the skilled nursing facility, but it is secondary to the primary reason for the stay–intense and daily treatment.
Seniors needing intense physical therapy, speech therapy, occupational therapy, or continuous medical support should reside in Skilled Nursing Facilities until they are recovered, reach a certain level, or plateau. Then you return home, where home healthcare takes over. The nurses, physical & occupational therapists, and speech pathologists come to your home. Eventually, when you have progressed in your recovery and do not need treatment as often, home healthcare stops, and you go to providers’ offices for an appointment.
Home Healthcare (HH)
Home Healthcare providers allow their clients to continue living in the comfort of their homes while providing care. The person still cannot get out and go to appointments easily, so the skilled providers come to you in your home two or three times a week or less, depending upon need. Ideally, in the recovery process, you eventually leave your home and go to their offices to receive treatment until you fully recover. Again, home healthcare does not provide custodial care in the home, except on rare occasions for short periods of time.
Understanding that Medicare is health insurance. It covers and pays for doctors, nurses, tests, hospitals–all the things you associate with medical treatment and recovery. Medicare does not provide custodial care, housekeeping, meal & laundry service, or taxis.
Will Medicare Cover Long-Term Care?
When someone says “long-term care” or “nursing home,” they generally mean the person is residing permanently in a facility because she cannot take care of herself–she cannot perform the 5 activities of daily living. Medicare does not pay for nursing home care. Even when medical necessity requires admittance to a nursing home (skilled nursing facility), the length of stay is capped at 100 days. There are rules around stopping and starting this coverage, coming from a hospital stay, and restarting a stay, but essentially, Medicare will only pay for 100 days per year in a nursing home. And Medicare approval for a stay of that length is rare. Again, Medicare pays for “nursing home” care for purposes of intense but temporary medical treatment.
Will Medicare Cover Skilled Nursing Facilities?
Medicare provides “Skilled Nursing Facilities” coverage, but patients must qualify based on stringent requirements. Medicare will only cover SNF care if all of the following are true:
- You are a recipient of Medicare Part A and have days of coverage remaining in your benefit period.
- A qualifying hospital stay preceded the need for SNF. An inpatient stay of at least 3 consecutive days in the hospital followed by admission into an SNF within 30 days of leaving the hospital is required for coverage.
- A doctor must have ordered inpatient SNF care based on medical necessity.
- Your condition requires skilled care daily.
- You need skilled services for an ongoing condition that was treated during your 3-day hospital stay OR a new condition that started while you were already receiving SNF care for an ongoing condition.
- The services must be reasonable and necessary for the treatment of your condition.
- You obtain care through a Medicare-certified SNF.
Even if you qualify, your stay will not last indefinitely.
How Many Days Will Medicare Pay for Skilled Nursing Care?
After qualifying for SNF care, your progress will be closely monitored for the length of your stay, the care you are receiving, and the above requirements to ensure Medicare will continue providing coverage. At a high level, Medicare will cover up to 100 days of SNF coverage within a single benefit period. Again, approval for that length of stay is rare. Medicare wishes to move you to less costly home healthcare as soon as medically possible.
In those 100 days, Medicare will cover the cost of the following:
- A semi-private room
- Meals
- Skilled nursing care
- Medical social services
- Medications
- Medical supplies and equipment usage
- Ambulance transport when required
- Dietary counseling
- Physical therapy, occupational therapy, and speech-language pathology when required to meet your health goal
It’s important to note that while Medicare will provide coverage for 100 days, you will have to supplement the coverage starting on day 21.
- Days 1 – 20: Medicare will pay the total cost; you pay nothing.
- Days 21 – 100: You pay the daily coinsurance, which can be up to $204 per day in 2024.
- Days 101+: Medicare pays nothing; you incur the total cost of care if you remain.
A detailed breakdown of coverage details can be found in Medicare’s SNF handbook. Medicare does not pay for nursing home care unless it is tied to a treatment program while you are in residence.
Will Medicare Cover Home Health Care?
Home healthcare falls under both Medicare Part A and Part B. Home healthcare is defined as part-time or intermittent skilled care when you are “homebound.” Homebound means you cannot leave your home without assistance. Assistance could be using a walker, wheelchair, crutches, or even a cane. You may need special transportation because of your condition. Your doctor may advise you not to leave your home because of your medical condition. These all constitute reasons Medicare will accept for home healthcare.
The usual services home healthcare provides on a part-time basis are: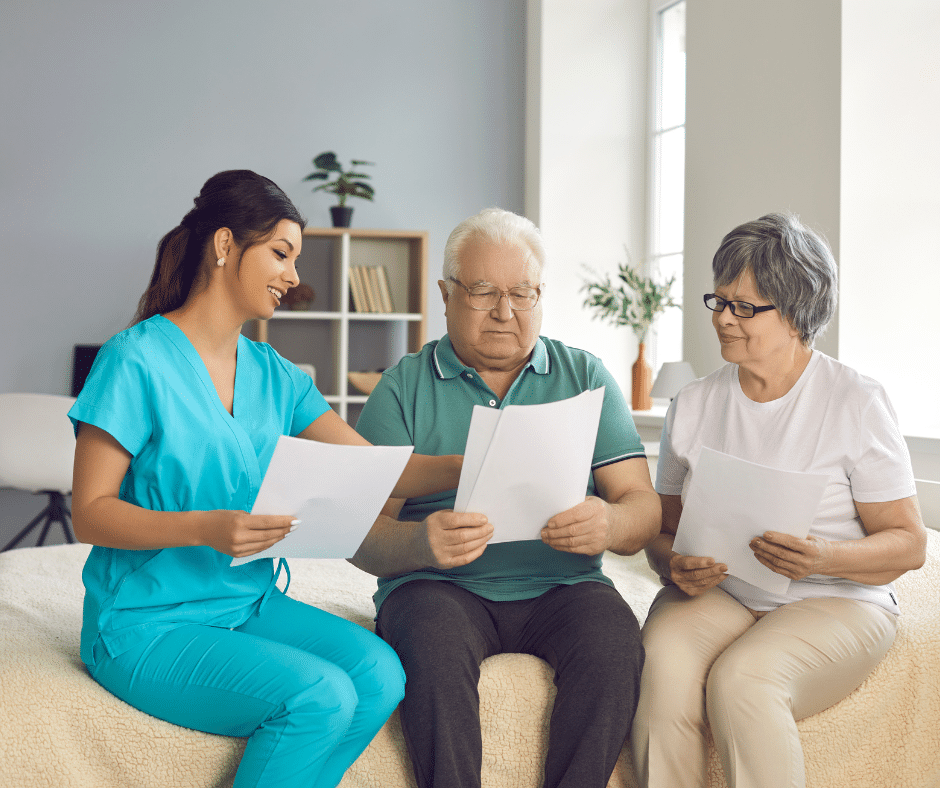
- physical therapy
- occupation therapy
- speech-language pathology services
- Injectable osteoporosis drugs
- durable medical equipment
A doctor must certify you need home health care through a face-to-face meeting. You need part-time or intermittent care, which may be up to 8 hours per day but with a maximum of 28 hours per week.
Home Healthcare does not include:
- 24-hour adult day care at home
- Meals delivered to the home
- Homemaker services
- Custodial (or personal) care help.
If you do attend adult day care in a facility, you can still qualify for home healthcare.
Getting the Most from Your Medicare: Which Direction?
 There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
Original Medicare
Original Medicare is Part A for inpatient hospital stays and Part B for outpatient services and doctor visits. There are no networks for Original Medicare. It is fee-for-service (FFS), which means if the doctor or facility accepts Medicare–accept assignment for Medicare is the proper terminology–then Medicare will reimburse the provider for medically necessary services rendered.
Original Medicare does not include Part D for prescriptions, and Orignal Medicare has big gaps in coverage. A quarter of people purchase some sort of supplemental insurance policy, such as Medigap, to fill in the gaps in coverage.
Medicare Advantage/Part C
The other direction is Medicare Advantage (or Part C). These plans are provided by a private insurance company that is Medicare-approved to provide health coverage that is equal to or better than Original Medicare.
The gaps in coverage are structured differently than Original Medicare. Medicare Advantage plans have a maximum out-of-pocket. Original Medicare does not. For example, the most popular Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs have a maximum out-of-pocket of less than $4,000. Original Medicare, on the other hand, does not have a maximum. The sky is the limit for your out-of-pocket costs.
Medicare Advantage is also built on provider networks. The Omaha, Lincoln, Council Bluffs metro area has four healthcare networks: CHI (Catholic Health Initiative), Nebraska Medicine, Methodist Health Systems, and Bryan Hospital. All these networks work with the Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs. Access to providers is a non-issue for us. In other places and with other Medicare Advantage plans, there can be issues and problems, but not here.
Home healthcare is zero for both Original Medicare and most Medicare Advantage plans.
Skilled nursing is zero for the first 20 days for both. On the 21st day, Original Medicare has a copay of $204 during the potential 100 days of coverage–again with no cap on expenses for Part B. Medicare Advantage plans have copays of various sizes, but the key is a limit to what you could pay– a maximum out-of-pocket.
For those who pay the additional premium for the Medigap plan, the skilled nursing facility copay will usually be covered entirely.
Medicare Part D
Medicare Part D prescription drug plans are another premium. Most Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs include the prescription drug plan and are mostly at zero cost.
Neither Original Medicare with a Medigap plan nor Medicare Advantage provides long-term care, custodial care, housekeeping, or adult day care. They may cover some of these services as incidental to providing skilled nursing care in a facility or home but for short periods.
Alternative Ways to Pay for the Care You Need
In 2021, the average cost of long-term care services ranged from $20,280 to $108,405 annually. These prices are exorbitant, and they’re only going up. As you age, the best thing you can do for your health and your wallet is to ensure you have the coverage you can rely on if you need long-term care. Since Medicare doesn’t pay for many long-term care scenarios–“nursing home care”–knowing your other options for coverage is crucial.
 Private Pay
Private Pay
Although challenging, some people will pay for their nursing home care from their savings and assets. By dipping into retirement accounts, tapping into assets such as property or investments, or simply saving up over their lifetimes, some seniors pay out-of-pocket for all the care they receive. This is rare.
One major benefit to this approach is that LTC facilities often prioritize private pay clients when space is limited. With the looming senior care crisis, this will get even more important in the years to come.
Long-Term Care Insurance
A separate long-term care insurance policy can pay the cost of residing in a long-term care facility. In most scenarios, these policies require that you need help with two or more of the activities of daily living (feeding, dressing, hygiene, continence, and toileting) before they take effect. There are usually elimination periods of 30, 60, 90, and 120 days before a policy will pay. The premiums for these insurance plans are not cheap. As you age, like life insurance, the price goes up and can be beyond the budget of many people. You also need to pass underwriting when you apply for the policy, though it will be guaranteed renewal for the rest of your life, no matter your health, as long as you continue to pay the monthly premium.
Veteran Benefits
If you served in the military, you may qualify for some sort of long-term care benefits from the Department of Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Medicaid
Often confused with Medicare, Medicaid is an entirely different health program. It’s partially funded by the federal government but funded and managed by the state.
Medicaid provides low-income seniors with financial help for long-term care. Each state has its own eligibility guidelines, but you’ll need to demonstrate financial need to qualify.
Many times people will tell me that so-in-so is in a “nursing home,” and they pay nothing. That is because all their assets have been depleted, and they are on county assistance. Medicaid is paying the bill, and all their assets are gone or will be upon death. The state takes homes and any other assets to offset the loss to the taxpayer who covers the expense.
 Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
LTC, SNF, and HH are a jungle of terms, regulations, insurance, and costs. It is even confusing for experts. Like figuring out your income tax or finances, consulting an insurance professional will be helpful. You need someone who knows Medicare, Medicare insurance, the CMS rules and regulations, and possesses years of experience dealing with Medicare. He can guide you through the maze of Medicare and help you take your health care into your own hands and plan for the best outcome.
You’re in the right place if you’re unsure where to start. Every week, I spend time helping those on Medicare just like you find the right coverage for their needs. At Omaha Insurance Solutions, we can help you figureout the best direction for you, enroll you in Medicare, choose a plan, and get all the T’s cross and I’s dotted on forms and applications. Each year, we will review your needs and the plans available to maximize your Medicare benefits.

Christopher Grimmond
Get in touch with us today at 402-614-3389 for a free, no-obligation consultation about your Medicare options.
 Navigating the Complexities: What You Need to Know About Medicare and Home Healthcare Coverage
Navigating the Complexities: What You Need to Know About Medicare and Home Healthcare Coverage
Are you confused about Medicare and home health care coverage? If so, you’re not alone. Navigating the complexities of these topics can be overwhelming. It’s essential to understand your options and ensure you receive the care you need.
Does Medicare pay for home health care services?
This article will delve into the ins and outs of Medicare and home healthcare coverage, providing the information you need to make informed decisions. We’ll explore the different types of Medicare plans and how they relate to home healthcare services, eligibility requirements, coverage limitations, and common misconceptions.
Whether you’re a senior seeking assistance or a caregiver supporting a loved one, understanding how long Medicare pays for home health care is crucial. By the end of this article, you’ll clearly understand what options are available and how to navigate the complex healthcare landscape.
Stay tuned to discover everything you need about Medicare and home healthcare coverage. Don’t let the confusion hold you back from accessing the care you deserve.
Different Types of Medicare Coverage
Medicare is a federal health insurance program that covers people over 65 and those with specific disabilities or chronic conditions. There are several types of Medicare plans, each with benefits and limitations. Knowing how long each Medicare plan pays for health care is critical. 
Original Medicare, also known as Medicare Part A and Part B, provides coverage for hospital stays, doctor visits, home healthcare, and some medical equipment. Medicare Part C, also known as Medicare Advantage, is a private insurance option combining Parts A and B, often including additional benefits such as prescription drug coverage and dental care. Both provide home healthcare coverage, but in specific ways unique to the plans.
Medicare Part D provides coverage for prescription drugs, while Medicare Supplement plans, also known as Medigap, help cover the costs of out-of-pocket expenses not covered by Original Medicare.
Understanding the differences between these plans is essential because they approach home health care differently.
 Understanding Home Healthcare Services
Understanding Home Healthcare Services
As the name suggests, home healthcare services provide medical care and support to individuals in their homes. This can include services such as nursing care, physical therapy, and speech-language therapy. Home health care is often a more convenient and cost-effective option than hospital or skilled nursing facility (SNF) care and can provide a higher level of comfort and independence for patients. It is skilled nursing care but provided in the home for those who would not have access to medical care otherwise.
The purpose of home health care is short-term treatment for an illness or injury, such as a stroke or broken hip. It is about getting back your health and independence again.
For the chronically ill and disabled, the goal of home health care is to maintain the highest level of ability and health.
Home healthcare services can be provided by a variety of healthcare professionals, including registered nurses, licensed practical nurses, physical therapists, occupational therapists, and speech-language pathologists. A physician typically orders services, and they are covered by Medicare and/or private insurance.
Home health care is not home care. Home care would be custodial services like housekeeping, bathing, feeding, etc. Medicare does not usually provide those types of personal services, strictly speaking. There are exceptions, however. On occasion, Medicare allows for a temporary home health aide to assist in the healing process.
Some injuries and illnesses may last for a long time. While home health care is a necessary service, the bigger question is: how long does Medicare pay for home healthcare?
Medicare Eligibility for Home Healthcare Coverage
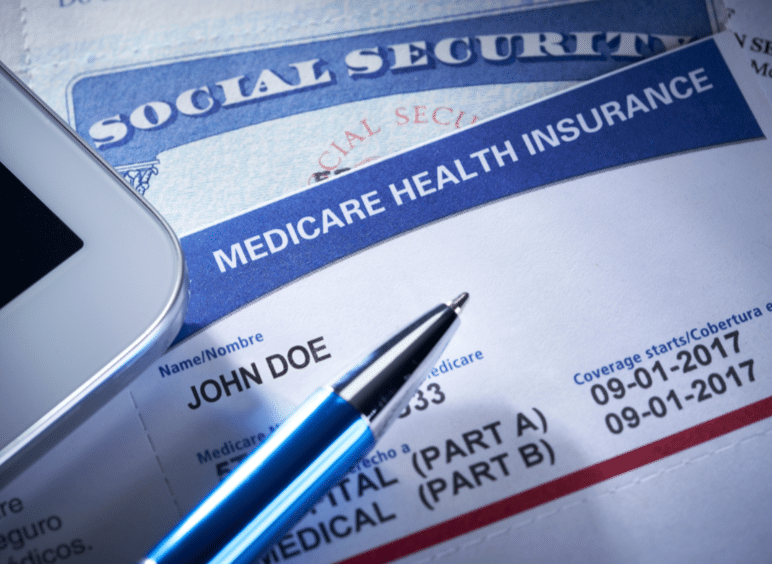
Individuals must meet specific requirements to be eligible for Medicare home healthcare coverage. First, they must be enrolled in Medicare Part A and/or Part B. Both Medicare Part A and Part B provide home healthcare coverage.
Under Part B, a person is eligible for home health care if she is homebound, requires skilled care, and is certified as needing care by a physician. The added benefit is Part B does not require a qualifying hospital stay.
The essential requirements of eligibility and access to Medicare home healthcare services are: homebound, physician certification, and Medicare-certified agency care.
Homebout, in Medicare terms, means that leaving the home requires a considerable and taxing effort. A physician is the gatekeeper of Medicare home healthcare. The physician certifies and/or recertifies a patient for access to home healthcare. Finally, a Medicare-certified agency must provide home healthcare services, not any healthcare provider.
Medicare Part A Coverage
In contrast, Medicare Part A provides home health care coverage in some situations. A hospital or skilled nursing facility stay triggers Part A. If a person has a three-day inpatient stay at a hospital or has a Medicare-covered Skilled Nursing Facility (SNF) stay, Part A will cover up to 100 days of home health care.
Note that a person must still meet the other eligibility requirements to receive home health care, such as needing skilled care, being homebound, and having a doctor certify that such care is necessary.
A person also must receive home health services within 14 days of being discharged from a hospital or SNF. If a person doesn’t meet all of the requirements for Part A coverage but is otherwise eligible for home health care benefits, her care will be financed under Part B.
Medicare Coverage For Home Healthcare Services Amounts
Regardless of whether Part A or Part B covers a person’s care, Medicare will pay:
- The entire approved cost of all covered home health services.
- Eighty percent of the Medicare-approved amount is for durable medical equipment.
Medicare covers a wide range of home health care visits, including skilled nursing care, physical therapy, occupational therapy, speech-language pathology, and medical social services. These services are typically provided part-time or intermittently, depending on the individual’s needs.
Medicare also covers specific durable medical equipment and supplies, such as wheelchairs, hospital beds, and oxygen equipment.
However, coverage limitations and restrictions may apply, and it’s essential to understand what services are covered and how much you may be responsible for paying out of pocket. The agencies providing the equipment and supplies can give details of costs.
 Limitations and restrictions of Medicare coverage for home health care
Limitations and restrictions of Medicare coverage for home health care
While Medicare provides coverage for many home healthcare services, there are limitations and restrictions to be aware of. For example, Medicare typically only covers part-time or intermittent care and may not cover 24-hour or long-term care.
In addition, Medicare may not cover certain services considered custodial care, such as help with bathing, dressing, and eating. Finally, there may be coverage limitations based on the individual’s medical condition. Some coverage is subject to annual or lifetime caps.
Certified Home Health Agency Disclosure of Covered Costs
Before home health care starts, the certified home health agency must tell the person how much Medicare will pay. The agency must also disclose if Medicare does not cover needed items or services. Then tell how much the person will have to pay for them.
For example, charges to a person may be:
- Medical services and supplies that Original Medicare doesn’t cover, such as prescription drugs or routine foot care
- 20 percent of the approved amount for Medicare-covered durable medical equipment such as wheelchairs, walkers, and oxygen equipment
Tips for Navigating Medicare and Home Healthcare Coverage
Navigating the complexities of Medicare and home healthcare coverage can be challenging, but several tips help make the process easier. First, it’s important to understand your needs and choose the Medicare plan that best fits them.
Second, work with your healthcare provider to ensure that a Medicare-certified agency orders and provides home healthcare services.
Finally, read the fine print and understand any coverage limitations or restrictions that may apply. The Medicare-certified agency is well versed in the cover limitations and costs. Be sure to consult with them ahead of time.
Alternative options for home health care coverage
While Medicare provides coverage for many home health care services, alternative options may be available to better meet your needs. For example, private insurance plans may offer more comprehensive coverage for certain services. Medicaid is another route for low-income individuals.
Private Home Health Care Insurance Policies
Home health care insurance is typically a private insurance policy purchased ahead of time to assist Medicare in caring for someone receiving home health care. The policy covers activities of daily living in the home, such as bathing, feeding, transportation, and housekeeping. Like any insurance, these alternative options must be purchased before the health issues arise. Many insurance carriers offer a variety of these types of policies.
In addition, a variety of community-based programs and organizations offer support and assistance to seniors and individuals with disabilities. These programs may include meal delivery, transportation services, and assistance with daily living activities.
 Home Health Agency Advance Beneficiary Notice of Noncoverage
Home Health Agency Advance Beneficiary Notice of Noncoverage
When a certified home health agency believes that Medicare may not pay for some or all of a person’s home health care, it must give the person a written notice called an Advance Beneficiary Notice of Noncoverage (ABN). The ABN might occur, for example, if the home health agency thinks that Medicare will not pay for items or services because:
- The care is not considered medically reasonable and necessary.
- The care is only unskilled, a home health care aide, like help with bathing or dressing.
- The person is not homebound.
- The person does not need skilled care on an intermittent basis.
The ABN must describe the service and/or items that may not be covered and explain why Medicare probably won’t pay. The notice must also include an estimate of the costs for the items and services so that the beneficiary can decide whether to receive the services, understanding that she may have to pay out-of-pocket for such care.
The ABN also gives directions for getting an official decision from Medicare about payment for home health services and supplies and for filing an appeal if Medicare won’t pay.
How Long Does Medicare Pay for Home Health Care?
There is no limit to the length of time that a person can receive home health care services. Once the initial qualifying criteria are met, Medicare will cover home health care as long as it is medically necessary. However, care is limited. There are a maximum number of visits per week and a certain amount of hours per day of care.
When a person first begins receiving home health care, the plan of care will allow for up to 60 days. At the end of this period, the physician must decide whether to recertify the patient for another 60 days. The patient must be recertified at least every 60 days if home health care is to continue.
Medicare does not limit the number of times a physician may recertify a patient. Provided all eligibility requirements continue, he can recertify an unlimited number.
What Happens When Medicare Stops Paying for Home Health Care?
A home health agency must give a beneficiary a written Home Health Change of Care Notice (HHCCN) when the patient’s plan of care changes because the home health agency decides to reduce or stop providing some or all of the home health services or supplies. Or, the patient’s doctor has changed the orders, which may reduce or stop certain home healthcare services or supplies that Medicare covers.
doctor has changed the orders, which may reduce or stop certain home healthcare services or supplies that Medicare covers.
For example, the doctor changes the care plan from five to three days a week. The agency issues an HHCCN. The beneficiary receives a notification in writing of the change.
The HHCCN lists the services or supplies that will be changed and gives the beneficiary instructions on what to do if she disagrees. The home health agency is not required to give a person an HHCCN when a Notice of Medicare Noncoverage is issued.
Notice of Medicare Noncoverage
When a person’s Medicare-covered services end, the home health agency must give the beneficiary a Notice of Medicare Noncoverage (NOMNC). This notice states when services will end as well as how to appeal the decision. The NOMNC also provides information on contacting the Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) to request an expedited appeal.
Once a person decides to appeal and has reached the BFCC-QIO, the home health agency must give the patient a detailed notice explaining why it believes Medicare-covered care should end. The agency should tell the applicable coverage rules and other information about the person’s situation.
A physician must submit a statement of appeal to the BFCC-QIO. It says the patient’s health will be jeopardized if care is discontinued. These factors determine how long Medicare pays for home health care. Knowledge of these rules is vital to maximize benefits and avoid costly mistakes.
Importance of understanding Medicare and home health care coverage
Understanding Medicare and home health care coverage is crucial for seniors and individuals with chronic conditions or disabilities. These programs provide access to essential medical care. They support individuals to maintain their independence and quality of life.
By understanding the different types of Medicare plans, eligibility requirements, coverage limitations, and alternative options, individuals can make informed decisions about their healthcare and ensure they receive the care they need.
Bottomline: Taking Advantage of Medicare and Home Healthcare Benefits
In conclusion, navigating the complexities of Medicare and home healthcare coverage can be challenging, but it’s essential for seniors and individuals with chronic conditions or disabilities. By understanding the different types of Medicare plans, eligibility requirements, coverage

Christopher J. Grimmond
limitations, and alternative options, individuals can make informed decisions about their healthcare and ensure they receive the care they need.
Whether you’re seeking home healthcare services for yourself or a loved one, working with your healthcare provider and understanding the coverage options available is essential. By taking advantage of Medicare and other home healthcare benefits, you can maintain your independence, improve your quality of life, and ensure you receive the care you deserve.
At Omaha Insurance Solutions, we help you understand the many Medicare rules. We navigate you through the forms and get the care you need. Call us at 402-614-3389 to speak with an experienced, licensed insurance agent professional.
Jimmo vs. Sebelius On Skilled Nursing
Skilled Nursing Care is amazingly complex. Because the Medicare coverage of Skilled Nursing Facility stays is so confusing, patients sued. The case went all the way to the Federal Courts. Jimmo vs. Sebelius, a class-action lawsuit, challenged the Center For Medicare & Medicaid Services (CMS) interpretation of the “improvement stand” that many used to interpret Medicare coverage of Skilled Nursing Facility booklet.
Medicare Coverage of Skilled Nursing Facility Stays: Improvement Standard
 This one hit home for me because of how it affected my mother and our family. My mother was in the last stages of ovarian cancer. It became clear that no treatment was going to work. She was on palliative care. During one of her episodes, she was in extreme pain. The hospital admitted my mother because intravenously administered pain killers were the only way to get her pain under control. After that, she was supposed to come home. But her condition was such that we were not going to be able to care for her adequately. We talked about a nursing home—skilled nursing—but one of the criteria at the time was the patient must be able to improve. Because she was terminal, improvement was definitely not in the cards. We were initially told that Medicare would not pay for her stay in a skilled nursing facility. However, that was not accurate. The people we were talking with were operating off old, outdated information.
This one hit home for me because of how it affected my mother and our family. My mother was in the last stages of ovarian cancer. It became clear that no treatment was going to work. She was on palliative care. During one of her episodes, she was in extreme pain. The hospital admitted my mother because intravenously administered pain killers were the only way to get her pain under control. After that, she was supposed to come home. But her condition was such that we were not going to be able to care for her adequately. We talked about a nursing home—skilled nursing—but one of the criteria at the time was the patient must be able to improve. Because she was terminal, improvement was definitely not in the cards. We were initially told that Medicare would not pay for her stay in a skilled nursing facility. However, that was not accurate. The people we were talking with were operating off old, outdated information.
Slow Deterioration of a Condition
On January 24, 2013, the class action lawsuit Jimmo vs Sebelius settled in favor of the patient, and the Center for Medicare & Medicaid Services (CMS) clarified its policy. Medicare coverage of Skilled Nursing Facility stays no longer required “improvement.” Instead, care could be prescribed to maintain the status of an individual’s condition, or slow the deterioration of a condition, as well as to improve the person’s condition.
Jimmo Website Explains New Medicare Coverage
As ordered by the federal judge in Jimmo v. Sebelius, the Centers for Medicare and Medicaid Services (CMS) published a new webpage containing important  information about the Jimmo Settlement on its CMS.gov website. The Jimmo webpage is the final step in a court-ordered Corrective Action Plan. The action reinforces the fact that Medicare does cover skilled nursing and skilled therapy services needed to maintain a patient’s function or to prevent or slow decline. Improvement or progress is not necessary as long as skilled care is required. The Jimmo standards apply to home health care, nursing home care, outpatient therapies, and, to a certain extent, for care in Inpatient Rehabilitation Facilities.
information about the Jimmo Settlement on its CMS.gov website. The Jimmo webpage is the final step in a court-ordered Corrective Action Plan. The action reinforces the fact that Medicare does cover skilled nursing and skilled therapy services needed to maintain a patient’s function or to prevent or slow decline. Improvement or progress is not necessary as long as skilled care is required. The Jimmo standards apply to home health care, nursing home care, outpatient therapies, and, to a certain extent, for care in Inpatient Rehabilitation Facilities.
In my mother’s case, the skilled nursing facility admitted my mother, even though she was terminal, to help slow the deterioration of her health. As it turned out, she passed away within two weeks of her admittance, and the personnel at her skilled nursing facility were outstanding! They made her last days as bearable as the situation would allow.
Medicare Coverage of Skilled Nursing Facilities Changed
 Medicare coverage of Skilled Nursing Facility stays practices have changed. Researchers assessed the impact of the Jimmo settlement by looking at changes to the number of physical therapy and/or occupational therapy visits per year, per patient, focusing specifically on the number of individuals who had 12 or more therapy visits during a 12-month timespan.
Medicare coverage of Skilled Nursing Facility stays practices have changed. Researchers assessed the impact of the Jimmo settlement by looking at changes to the number of physical therapy and/or occupational therapy visits per year, per patient, focusing specifically on the number of individuals who had 12 or more therapy visits during a 12-month timespan.
Healthcare is very expensive. There are many conflicting groups and interests. The rules, policies, and mechanisms are complex. Some of the people you deal with can be frustrating. The complexity of the system is driven home to me daily as I talk with clients and deal with issues that arise. You need to be aware of the rules and regulations around Medicare coverage and nursing home care. Or have someone who knows them and can help.
Medicare Coverage For Skilled Nursing Facilities
Skilled Nursing Facilities—or better known in the jargon of Medicare as SNF—is the cause of much consternation among people on Medicare. The reason for the  distress and stress is because Medicare beneficiaries are sometimes denied coverage. This both confuses and angers Medicare beneficiaries because there doesn’t seem to be any rhyme or reason to the denials. People ask: does Medicare cover Skilled Nursing Facility?
distress and stress is because Medicare beneficiaries are sometimes denied coverage. This both confuses and angers Medicare beneficiaries because there doesn’t seem to be any rhyme or reason to the denials. People ask: does Medicare cover Skilled Nursing Facility?
Medicare Billing Guidelines For Skilled Nursing Facility
From my observation over the years, doctors’ offices sometimes don’t follow the Medicare billing guidelines for Skilled Nursing Facility. I understand everyone is busy and people are certainly well-intentioned, but Medicare is insurance. Insurance has rules, protocols, and forms. A lack of adequate explanation to Medicare is many times the cause of Medicare denials, I’ve seen over the years. Other times the situation does not meet the Medicare criteria for Skilled Nursing Facility stays.
What are the Medicare Skilled Nursing Facility Requirements?
 When skilled nursing is prescribed, five Medicare Skilled Nursing Facility requirements must be met. The first is a qualifying hospital stay.
When skilled nursing is prescribed, five Medicare Skilled Nursing Facility requirements must be met. The first is a qualifying hospital stay.
The Medicare beneficiary must stay as an inpatient for three consecutive days in the hospital. Each of these is an essential ingredient. The beneficiary must be admitted to the hospital. If the patient is only admitted for “observation,” she will not qualify. She must be an “inpatient.” Next, the stay must be consecutive. It can’t be a day or two within a short period of time. It must be at least 3 consecutive days. And finally, it must be at least 3 days, not counting the day of dismissal.
Many times, people assume the day of dismissal counts, but that is definitely not the case. Three days of inpatient care at least with a fourth day for the dismissal. Sometimes people will complain that the patient doesn’t need a third day, but if you want the person to qualify, she must stay at least three consecutive days.
Medicare Skilled Nursing Facility Benefit Period
The second ingredient for Medicare to cover a skilled nursing facility stay is the admittance must occur with 30 days of dismissal from the qualifying hospital stay.
 My mother-in-law had open heart surgery a while back. Her cardiologist prescribed that she stay in a skilled nursing facility for cardiac rehab. She was not a very cooperative patient. She refused. My wife was insistent and explained that if she didn’t go then, she would lose the opportunity for skilled nursing rehab. My mother-in-law’s response was she would do it later if she needed it.
My mother-in-law had open heart surgery a while back. Her cardiologist prescribed that she stay in a skilled nursing facility for cardiac rehab. She was not a very cooperative patient. She refused. My wife was insistent and explained that if she didn’t go then, she would lose the opportunity for skilled nursing rehab. My mother-in-law’s response was she would do it later if she needed it.
Many people mistakenly think they can go to a nursing home for rehab if they simply want to. It must be within the 30-day window after dismissal from an inpatient stay. Otherwise, Medicare will not pay. Now you may think it is not fair, or right, or make sense. I am simply stating the rules and facts.
Medicare Guidelines for Skilled Nursing Facility
 The third requirement for admittance to a skilled nursing facility (SNF) is the treatment can only be provided by a skilled nursing facility.
The third requirement for admittance to a skilled nursing facility (SNF) is the treatment can only be provided by a skilled nursing facility.
What this usually means is “full time” or five day a week care. In other words, the same level of treatment cannot be provided by going to a treatment center by appointment a few times a week. Only an inpatient skilled nursing facility can provide the level of intense treatment needed for adequate recovery. This can be a tricky call and where judgments can and are questioned.
Medicare Denial Skilled Nursing Facility
I had a client who had a knee replacement. Usually a knee replacement, even with  complications, does not require admittance to a skilled nursing facility (SNF) because physical therapy is something that can be completed by going to the physical therapist’s office and/or doing exercises on your own. This situation was different.
complications, does not require admittance to a skilled nursing facility (SNF) because physical therapy is something that can be completed by going to the physical therapist’s office and/or doing exercises on your own. This situation was different.
She was living in a small apartment with lots of furniture. There was a pet. The husband was feeble. While she was not very old, her knee was not recovering at the usual pace. The doctor recommended skilled nursing care, but Medicare denied the prescription.
The family came to me with questions. I suggested they explain the situation to the doctor in greater detail and with more urgency. She was a serious “fall risk” because of her living situation.
Once the idea was emphasized sufficiently in the doctor’s notes to Medicare, Medicare understood that the work that had been done would be undone if she fell at home because of a pet, furniture, and/or feeble husband, etc. The request was approved.
Skilled nursing is very expensive. Medicare needs to understand the “medical necessity” of a prescription. Once the idea is communicated effectively, things can happen.
List of Medicare Approved Skilled Nursing Facilities
The fourth ingredient is that a doctor, or another appropriate medical professional, certifies that the patient needs the type of daily therapy that can only be performed in a skilled nursing facility. The skilled nursing facility must also be a Medicare-certified skilled nursing facility. You can go to Medicare.gov to find certified sites and Medicare the star ratings for Skilled Nursing Facilities.
The fifth and final requirement can be confusing. The skilled nursing care must be for the reason the patient was in the hospital for the three days.
Imagine John goes to the hospital because of a broken hip. While John was in the hospital, he has a stroke. The doctor certifie s John for treatment at a skilled nursing facility for the stroke, not the hip issue. The skilled nursing recommendation does not have to be based on the reason the person was admitted to the hospital, but it does need to be because of something he was treated for during the 3-day hospital stay.
s John for treatment at a skilled nursing facility for the stroke, not the hip issue. The skilled nursing recommendation does not have to be based on the reason the person was admitted to the hospital, but it does need to be because of something he was treated for during the 3-day hospital stay.
As you can see, Medicare coverage for skilled nursing facilities can be complex. It’s important to have some understanding so that you know what to expect, or not to expect, when it comes to Medicare coverage of skilled nursing facility care, and how to navigate the processes to your benefit and the benefit of loved ones. Medicare Part A covers the Skilled Nursing Facility, but the rule must be followed for Skilled Nursing Facility Medicare reimbursement to happen.
The chances are you or someone in your family will require skilled nursing care because of a serious injury, stroke, or surgery.  Twenty-five percent of skilled nursing stays are less than three months. Many, however, are longer. Nursing home care costs vary from state to state and location to location. The questions my clients ask are: how long does Medicare pay for skilled nursing care?
Twenty-five percent of skilled nursing stays are less than three months. Many, however, are longer. Nursing home care costs vary from state to state and location to location. The questions my clients ask are: how long does Medicare pay for skilled nursing care?
Skilled Nursing Care Costs Are High
 Depending upon the state in which you reside, the daily costs associated with nursing home care vary widely between $140 and $771 per day for a semi-private room in 2017. The average cost was $235 per day for a semi-private room. Multiplying that out the monthly cost associated with skilled nursing care ran anywhere between $4,258 and $23,451 per month for a semi-private room, with the average being closer to $7,148 each month for a semi-private room. For most people, those are prohibitive costs!
Depending upon the state in which you reside, the daily costs associated with nursing home care vary widely between $140 and $771 per day for a semi-private room in 2017. The average cost was $235 per day for a semi-private room. Multiplying that out the monthly cost associated with skilled nursing care ran anywhere between $4,258 and $23,451 per month for a semi-private room, with the average being closer to $7,148 each month for a semi-private room. For most people, those are prohibitive costs!
How Much Skilled Nursing Does Medicare Pay For?
Many of my clients will call when faced with the possibility of going into a skilled nursing facility. Illness is scary enough. You don’t want to worry about overwhelming medical bills. My people want to know they’re covered. They want to know how much skilled nursing does Medicare pay for. Do Medicare Advantage plans cover skilled nursing facilities? Do Medicare Supplements cover skilled nursing facilities? So, the big question is: who pays?
Medicare Skill Nursing Benefit Period Is 100-Days
So, how many days does Medicare cover skilled nursing facility care? The Medicare Skilled Nursing Facility (SNF) benefit period, or “Spell of care,” is 100 days. The benefit period ends when the patient leaves the SNF for 3o days, and a new 100 day benefit period is available after 60 days.
Skilled Nursing Facility’s Legal Obligations
When a patient leaves a hospital and moves to a nursing home that provides Medicare coverage, the nursing home must give the patient written notice of whether the  nursing home believes that the patient requires a skilled level of care and thus merits Medicare coverage. Even in cases where the SNF initially treats the patient as a Medicare recipient, after two or more weeks, often, the SNF will determine that the patient no longer needs a skilled level of care and will issue a “Notice of Non-Coverage” terminating the Medicare coverage.
nursing home believes that the patient requires a skilled level of care and thus merits Medicare coverage. Even in cases where the SNF initially treats the patient as a Medicare recipient, after two or more weeks, often, the SNF will determine that the patient no longer needs a skilled level of care and will issue a “Notice of Non-Coverage” terminating the Medicare coverage.
Whether the non-coverage determination is made on entering the SNF or after a period of treatment, the patient can submit or not to Medicare. The patient (or his or her representative) should always ask for the bill to be submitted. This requires the nursing home to submit the patient’s medical records for review to the fiscal intermediary, an insurance company hired by Medicare, which reviews the facility’s determination. The review costs the patient nothing and may result in more Medicare coverage. While the review is being conducted, the patient is not obligated to pay the nursing home. However, if the appeal is denied, the patient will owe the facility retroactively for the period under review.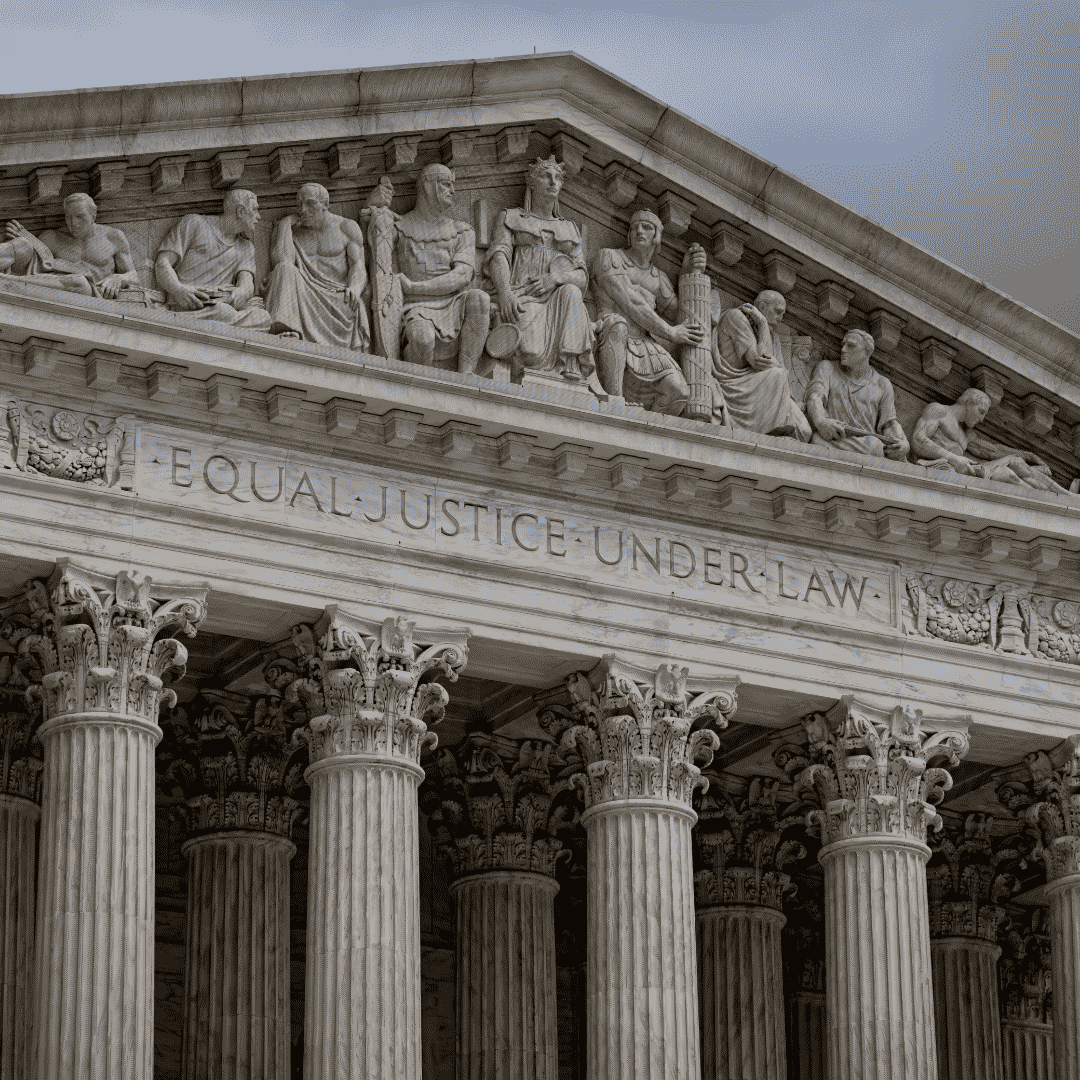
If the fiscal intermediary agrees with the nursing home that the patient no longer requires a skilled level of care, the next level of appeal is to an Administrative Law Judge. This appeal can take a year and involves hiring a lawyer. It should be pursued only if, after reviewing the patient’s medical records, the lawyer believes that the patient was receiving a skilled level of care that should have been covered by Medicare. If you are turned down at this appeal level, there are subsequent appeals to the Appeals Council in Washington, and then to federal court.
Day 101 You Pay
 If you need more than 100 days of SNF care in a benefit period, how many days will Medicare pay for skilled nursing care? Nothing. SNF is meant to be short term. You will need to pay out of pocket if your care ends because you are run out of days. The SNF is not required to provide written notice. It is important that you or a caregiver keep track of how many days you spend in a SNF to avoid unexpected costs after Medicare coverage ends.
If you need more than 100 days of SNF care in a benefit period, how many days will Medicare pay for skilled nursing care? Nothing. SNF is meant to be short term. You will need to pay out of pocket if your care ends because you are run out of days. The SNF is not required to provide written notice. It is important that you or a caregiver keep track of how many days you spend in a SNF to avoid unexpected costs after Medicare coverage ends.
How Else to Pay For Skilled Nursing Care
If you are receiving medically necessary physical, occupational, or speech therapy, Medicare may continue to cover those skilled therapy services even when you have used up your SNF days in a benefit period, but Medicare will not pay for your room and board, meaning you may face high costs.
used up your SNF days in a benefit period, but Medicare will not pay for your room and board, meaning you may face high costs.
Medicare does not cover long term care or custodial care. You may wish to move to a home health care situation at that point. Medicare pays for home health care, and the costs are much less. If you have long-term care insurance, it may cover your SNF stay after your Medicare coverage ends. If your income is low enough, you may be eligible for Medicaid to cover the cost of your stay.
Unlimited Skilled Nursing Benefit Periods
Once you are out of skilled nursing for 60 days, your SNF benefit period ends, but you may become eligible again for another SNF benefit period after a qualifying hospital stay of 3-days. There is no limit on the number of benefit periods available to a Medicare beneficiary as long as the Medicare requirements are met.
In other words, a person could potentially keep going into Medicare covered skilled nursing care every 100 days after a 60-day break as long as it is preceded by a qualifying hospital stay of 3-days. While repeat 100 day stays in a skilled nursing facility are not likely, that does give an idea of the level of incredible care available to a Medicare beneficiary.
NO Insurance: $176 Per Day
Medicare Supplements and Medicare Advantage plans pick up large portions of the 100-benefit period. The amount covered depends on the type of Medicare Supplement plan and Advantage plan. If the patients has neither, just Original Medicare, she is responsible for 21-100 days. The per day cost is currently $176 (2020).
30 Or 60 Days
 An important note on the number of days out of a Skilled Nursing Facility approved stay. If a patient has left the SNF for 30-days or less, she may return without a 3-day inpatient hospital stay to initial the stay, but the 100-day count continues from where it left off. If the patient has been out of the SNF for 60-days for less, but more than 30-days, she will need another 3-day hospital stay for Medicare to pay for the time in the Skilled Nursing Facility. And the 100-day count continues from where it left off. After 60 consecutive days without SNF care, a new benefit may begin. There is no limit to the number of benefit periods.
An important note on the number of days out of a Skilled Nursing Facility approved stay. If a patient has left the SNF for 30-days or less, she may return without a 3-day inpatient hospital stay to initial the stay, but the 100-day count continues from where it left off. If the patient has been out of the SNF for 60-days for less, but more than 30-days, she will need another 3-day hospital stay for Medicare to pay for the time in the Skilled Nursing Facility. And the 100-day count continues from where it left off. After 60 consecutive days without SNF care, a new benefit may begin. There is no limit to the number of benefit periods.
Dave’s Scenario
Let’s layout some common scenarios. You might need your calculator or at least your fingers and toes to keep track.
Imagine David is in the hospital for 4 days because of a stroke. He is then admitted to a skilled nursing facility for 20 days. Dave leaves the skilled nursing facility for 28 days, but he has a complication. Dave falls going to the bathroom. The doctor readmitted him into the nursing home. He is within the 30-day window. No problem. Medicare will pay for that.
If, however, David was out of the nursing home 31 days, and he fell, he would need another 3-day stay in the hospital to be readmitted to the skilled nursing facility so Medicare would pay. Dave’s doctor may or may not be able to get him re-admitted to the hospital based upon his medical condition.
Summary
Skilled Nursing Facilities (SNF) are incredibly expensive. How long does Medicare pay for Skilled Nursing Care? Medicare does cover a 100-day benefit period. Medicare Supplements and Medicare Advantage plans cover large portions of the stay, depending on the plan. The cost, however, starting day 21 is $176 per day to patients without any additional coverage. The 100-day benefit period has very strict rules when it begins and ends. There are rules to which you need to be attentive to avoid unexpected and large bills, and it is worth talking with your insurance agent to make sure you have the maximum amount of coverage you can afford.
 Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
Do you or a loved one need hospice care in a skilled nursing facility? Understanding Medicare coverage for this essential service is crucial for maximizing benefits and ensuring quality end-of-life care. This article will explore some of the ins and outs of hospice coverage I didn’t know when my mother was in hospice. We discuss the question of whether Medicare pays for hospice in a skilled nursing facility.
Navigating the complex world of healthcare can be overwhelming, especially when faced with a difficult situation like imminent death like I experienced with my mother. That’s why I’m here to break it down for you. I’ll explain what hospice care entails, how it differs from other types of care, and, most importantly, what Medicare covers. With this information, you can be confident in your ability to advocate for yourself or your loved one and ensure that all available resources are utilized.
At Omaha Insurance Solutions, information is power regarding healthcare decisions. We aim to make complex topics accessible, providing you with the tools you need to confidently navigate the healthcare system. So, let’s dive in and discover how Medicare can support you during a challenging time.
What is Hospice Care & Who is Eligible?
Hospice care focuses on providing comfort and support to individuals in the final stages of a terminal illness. The goal is to improve the quality of life for patients by managing pain and symptoms while offering emotional and spiritual support to both the patient and their loved ones. Hospice care can be provided in various settings, including skilled nursing facilities.
To be eligible for hospice care, a person must have a life expectancy of six months or less, as certified by a physician. This certification is required for Medicare coverage, which we will discuss further in the following sections. It’s important to note that choosing hospice care does not mean giving up on treatment altogether. It means shifting the focus to comfort and quality of life rather than curative measures.
Hospice care is a holistic approach that addresses individuals’ physical, emotional, and spiritual needs nearing the end of life. It provides a compassionate and supportive environment where patients receive specialized care tailored to their unique needs. Now that we have a basic understanding of hospice care, let’s explore how it relates to skilled nursing facilities and the coverage provided by Medicare.
Understanding Skilled Nursing Facility Care and Medicare Coverage
Skilled nursing facilities (SNFs) are residential facilities that provide round-the-clock nursing care for individuals requiring more intensive medical attention than they could receive at home. SNFs are equipped with trained healthcare professionals, including nurses and therapists, who can address the complex needs of patients. SNF care is often required when individuals have conditions that require ongoing medical monitoring, such as chronic illnesses or post-surgical recovery. Medicare covers certain SNF services, including skilled nursing care, rehabilitation therapy, and medications. However, it’s important to note that not all services provided in a SNF are covered by Medicare, and this includes hospice care.
Medicare Coverage for Hospice in a Skilled Nursing Facility
 Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
The criteria are the same as for hospice. Firstly, the individual must be eligible for Medicare Part A, which covers inpatient hospital stays, skilled nursing facility care, and hospice care. Secondly, the hospice care must be certified by a Medicare-approved hospice provider. Thirdly, the individual must have a life expectancy of six months or less, as certified by a physician. Lastly, individuals must agree to forgo curative treatments for their terminal illness and receive only palliative care.
The SNF is not primarily providing hospice care. A hospice team coordinates with the SNF to provide the service in the SNF. The location of the hospice care is secondary. The SNF is a location, like the home.
However, there must be a Medicare-covered reason or treatment to be granted admittance to a skilled nursing facility. The SNF is primarily a medical facility for patients to get better. It is not a hospice facility providing room and board, housekeeping, bathroom transfers, etc.
Medicare Hospice Benefits for My Mom
The doctors diagnosed my mother with ovarian cancer in 2012. I was living in Kansas at the time. I wasn’t able to go on doctor visits with her. My brother, Paul, was taking care of my mom. I would get information about her situation, but it was spotty.
My mother was an ‘I’m in charge’ type of person. Phyllis determined the flow of information, and it was sparse.
Talking with your mother about her health when her mortality is so tightly fixed to it is hard. Looking back now, I was a chicken. Who wants to talk about saying goodbye? I didn’t realize the seriousness of her health situation until much later. I assumed she didn’t speak about her own death, and I didn’t know how to initiate the conversation. We were all in different forms of denial.
At the end of 2012, the doctors said there was nothing more to be done. I don’t think I fully grasped what that meant at the time. I also did not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
My mother was admitted to hospice care (Medicare Hospice Benefits Booklet).
Mom’s Terminal Illness
Nature, in its less than glorious side, took its course rapidly. My mother’s health deteriorated in a few short weeks.
Cancer is a painful disease. The healthcare personnel gave her various painkillers, but even as they did so, we all insanely talked about not wishing to cause addiction. The pain had its own mind.
At various times, my mother’s suffering would be such that she needed to go to the hospital. There, the doctors administered intravenous medications that were faster acting and stabilized her pain level.
During the last visit, it became clear that we could not care for her at home. My father, John Grimmond–who would pass away six months later–was not physically able to care for our mother. I was in Kansas, my other brother, Tom, was in Sioux Falls, and Paul was in Omaha but busy with his career and family.
My mother needed around-the-clock care. We asked, ‘Does Medicare pay for hospice in a skilled nursing facility?’ The real question was whether Medicare would pay for a skilled nursing facility while my mother died. Strictly speaking, Medicare does not pay for custodial care. Custodial care is bathing, feeding, toileting, etc. Medicare doesn’t cover room and board if you get hospice care while in a nursing home or a hospice inpatient facility. That is out of your pocket.
Qualifying for Skilled Nursing Facility Care while on Hospice
The staff at the hospital initially told us that our mother needed to go to a skilled nursing facility (SNF) because they recognized she required more care than we could provide. They informed us that Medicare would provide and pay for hospice care in the Skilled Nursing Facility, but the cost of room and board and custodial nursing care would not be covered, and they were correct. Medicare coverage for skilled nursing when you are in hospice is tricky.
skilled nursing when you are in hospice is tricky.
The fortunate occurrence, however, was the intravenous nature of my mother’s painkillers. Other than a hospital, you can only receive intravenous medication treatment in a skilled nursing facility. The nature of my mom’s treatment triggered a reason Medicare would accept her being admitted to a skilled nursing facility and pay for it.
Medicare does cover skilled nursing care after a qualifying hospital stay of 3-days or more. Intravenous medication administration also requires a skilled nursing facility. A home health care nurse showing up several times at home would not be adequate. Also, my mother needed physical therapy to improve her strength after the reaction to the pain. From Medicare Part A and Part B, there were sufficient reasons for Medicare to pay for her stay in the skilled nursing facility (SNF) while she was in hospice.
Does Medicare Pay For Skilled Nursing Care During Hospice?
Strictly speaking, Medicare does not pay for skilled nursing care because someone is in hospice, but other triggering events often cause Medicare to cover skilled nursing care.
For example, someone who is in hospice falls and breaks a hip. That situation would justify skilled nursing care. A person develops an infection or pneumonia that results in hospitalization. Then, they qualify for a skilled nursing stay.
How to Navigate the Medicare Coverage Process for Hospice in a Skilled Nursing Facility
 Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
1. The first step is to consult with the individual’s physician to determine if they meet the eligibility criteria for hospice care in a SNF. The physician can provide the necessary certification and guidance through the process. He knows the triggering circumstances that justify a skilled nursing facility stay.
2. It’s important to choose a Medicare-approved hospice provider with experience providing SNF care. They will be able to guide you through the necessary paperwork and ensure that all requirements are met. The health professionals are very familiar with Medicare’s billing codes and protocols for admittance to a SNF.
3. If the individual is already receiving care in a SNF, it’s important to coordinate with the facility to ensure a smooth transition to hospice care. The SNF staff can provide valuable information and support during this process.
4. Familiarize yourself with Medicare’s costs and coverage for hospice care in a SNF. This will help you plan and make informed decisions regarding the individual’s care.
The professionals you deal with know the Medicare rules and the subtleties of maximizing coverage in different circumstances. Listen attentively to their guidance.
Common Misconceptions about Medicare Coverage of SNF During Hospice
Several common misconceptions exist about Medicare coverage for hospice care in a SNF. Let’s address some of these misconceptions and provide clarity:
provide clarity:
1. Medicare only covers hospice care in certain settings: Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, and skilled nursing facilities. As long as the eligibility criteria are met, Medicare will cover hospice care in a SNF.
2. Medicare covers room and board in a SNF. As a rule, Medicare does not cover room and board in a SNF because the individual is receiving hospice care, though room and board may be covered because the patient is in the SNF for reasons other than hospice.
3. Medicare coverage for hospice care is limited to specific conditions: Medicare coverage for hospice care is not limited to specific conditions or illnesses. As long as the eligibility criteria are met, Medicare will provide coverage for hospice care in a SNF for any terminal illness.
4. Medicare coverage for hospice care is limited to a certain time frame: Medicare does not limit the duration of hospice care coverage in a SNF. As long as the individual meets the eligibility criteria, Medicare will continue to cover the necessary services.
Bottomline: Ensuring Quality Care and Coverage for Hospice in a SNF through Medicare
Maximizing Medicare coverage for hospice care in a skilled nursing facility is essential for ensuring quality end-of-life care. By understanding the eligibility criteria, coverage details, and navigating the Medicare system, you can advocate for yourself or your loved one and ensure all available resources are utilized.
Remember, hospice care is a compassionate and holistic approach that focuses on providing comfort and support during the final stages of a terminal illness. Medicare provides coverage for hospice care in a SNF, including room and board, medications, and necessary medical equipment. By staying informed and proactive, you can maximize Medicare coverage and ensure that the individual receives the care they need.
 Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Phyllis Grimmond 1935-2013 R.I.P.
The Bottomline: Benefit Knowledge Makes for Maximum Benefits
At Omaha Insurance Solutions, we understand the importance of access to accurate and reliable information regarding healthcare

Christopher J. Grimmond
decisions. We aim to empower you with the knowledge and resources to navigate the complex world of Medicare coverage. It is important to know that Medicare pays for hospice care in a skilled nursing facility.
By maximizing benefits and ensuring quality care, we can make a difference in the lives of individuals and their loved ones during this challenging time. Call us at 402-614-3389 to ensure you have a Medicare plan protecting you and your loved ones. Speak with an experienced licensed insurance agent profession.
What Are Skilled Nursing Facilities?

All of us have strong memories of visiting the “old folks’ home.” Whether grandparents, relatives, or friends, we recall the smells, linoleum, long hallways, and institutional dormitory rooms. “Old folks’ homes” or nursing homes fall under the category of Skilled Nursing Facilities (SNF). Medicare covers skilled nursing facilities within limits.
Patients go to the SNF after surgeries to recover, from illnesses to heal, and from injuries to recover and strengthen. Skilled Nursing Facilities are for temporary treatment, not long term residential care or custodial care, like memory care. Other facilities, like senior living communities, assisted living, or senior care centers describe other types of facilities that assist seniors.
A skilled nursing facility provides highly skilled professionals, such as occupational therapists, physical therapists, registered nurses, speech therapists. The advantage of an SNF is these professions are available 24 hours a day for the patients. The level of care is very high but short term.
Post-Acute & Skill Rehab Services
 Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Medicare covers skilled nursing facilities within specific parameters. Nursing home care is for individuals who have reached a point in life when they can no longer perform activities of daily living. This is referred to as custodial care. In other words, they cannot bath, feed, and dress themselves. Medicare will not pay for those services to be provided exclusively.
Skilled Nursing is for after surgery or acute illness, for example, hip surgery for a fractured hip or a stroke. A skilled nursing facility admits patients for a short period of time after being in the hospital to aid in their healing and/or rehabilitation. Hospitals are incredibly expensive, and a skilled nursing facility can provide the necessary treatment at a lower cost.
Medicare Criteria For Skilled Nursing Facilities
The tricky part about skilled nursing facilities is admittance. A skilled nursing facility requires patients to meet certain essential criteria for admittance and for Medicare to pay. This is the complex checklist:
- The patient must be admitted to a hospital as an “inpatient” for at least three consecutive days, not including the day of dismissal. She can’t be in the
 hospital for “observation” for it to count for Medicare to pay.
hospital for “observation” for it to count for Medicare to pay. - Medicare mandates patient admittance to the skilled nursing facility within 30 days of discharge from the hospital. If problems arise later—past 30 days—the patient cannot go to the skilled nursing facility and have Medicare pay for it.
- Only a skilled nursing facility can provide the type of care necessary for the patient’s recovery. A skilled nursing facility would provide intense physical therapy for a hip injury or occupational therapy after a stroke. Going to the physical therapist’s office a couple of times a week would not be sufficient in those cases.
- A doctor, or appropriate medical professional, must certify that skilled nursing care is required for recovery.
- The patient must be treated for the same condition for which she was in the hospital.
There are nuances and exceptions to some of these rules. The list gives you a good idea about how skilled nursing fits into your Medicare health insurance. The Omaha, NE area has many quality Medicare certified facilities, and You can find them on the Medicare.gov website.