 Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
Do you or a loved one need hospice care in a skilled nursing facility? Understanding Medicare coverage for this essential service is crucial for maximizing benefits and ensuring quality end-of-life care. This article will explore some of the ins and outs of hospice coverage I didn’t know when my mother was in hospice. We discuss the question of whether Medicare pays for hospice in a skilled nursing facility.
Navigating the complex world of healthcare can be overwhelming, especially when faced with a difficult situation like imminent death like I experienced with my mother. That’s why I’m here to break it down for you. I’ll explain what hospice care entails, how it differs from other types of care, and, most importantly, what Medicare covers. With this information, you can be confident in your ability to advocate for yourself or your loved one and ensure that all available resources are utilized.
At Omaha Insurance Solutions, information is power regarding healthcare decisions. We aim to make complex topics accessible, providing you with the tools you need to confidently navigate the healthcare system. So, let’s dive in and discover how Medicare can support you during a challenging time.
What is Hospice Care & Who is Eligible?
Hospice care focuses on providing comfort and support to individuals in the final stages of a terminal illness. The goal is to improve the quality of life for patients by managing pain and symptoms while offering emotional and spiritual support to both the patient and their loved ones. Hospice care can be provided in various settings, including skilled nursing facilities.
To be eligible for hospice care, a person must have a life expectancy of six months or less, as certified by a physician. This certification is required for Medicare coverage, which we will discuss further in the following sections. It’s important to note that choosing hospice care does not mean giving up on treatment altogether. It means shifting the focus to comfort and quality of life rather than curative measures.
Hospice care is a holistic approach that addresses individuals’ physical, emotional, and spiritual needs nearing the end of life. It provides a compassionate and supportive environment where patients receive specialized care tailored to their unique needs. Now that we have a basic understanding of hospice care, let’s explore how it relates to skilled nursing facilities and the coverage provided by Medicare.
Understanding Skilled Nursing Facility Care and Medicare Coverage
Skilled nursing facilities (SNFs) are residential facilities that provide round-the-clock nursing care for individuals requiring more intensive medical attention than they could receive at home. SNFs are equipped with trained healthcare professionals, including nurses and therapists, who can address the complex needs of patients. SNF care is often required when individuals have conditions that require ongoing medical monitoring, such as chronic illnesses or post-surgical recovery. Medicare covers certain SNF services, including skilled nursing care, rehabilitation therapy, and medications. However, it’s important to note that not all services provided in a SNF are covered by Medicare, and this includes hospice care.
Medicare Coverage for Hospice in a Skilled Nursing Facility
 Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
The criteria are the same as for hospice. Firstly, the individual must be eligible for Medicare Part A, which covers inpatient hospital stays, skilled nursing facility care, and hospice care. Secondly, the hospice care must be certified by a Medicare-approved hospice provider. Thirdly, the individual must have a life expectancy of six months or less, as certified by a physician. Lastly, individuals must agree to forgo curative treatments for their terminal illness and receive only palliative care.
The SNF is not primarily providing hospice care. A hospice team coordinates with the SNF to provide the service in the SNF. The location of the hospice care is secondary. The SNF is a location, like the home.
However, there must be a Medicare-covered reason or treatment to be granted admittance to a skilled nursing facility. The SNF is primarily a medical facility for patients to get better. It is not a hospice facility providing room and board, housekeeping, bathroom transfers, etc.
Medicare Hospice Benefits for My Mom
The doctors diagnosed my mother with ovarian cancer in 2012. I was living in Kansas at the time. I wasn’t able to go on doctor visits with her. My brother, Paul, was taking care of my mom. I would get information about her situation, but it was spotty.
My mother was an ‘I’m in charge’ type of person. Phyllis determined the flow of information, and it was sparse.
Talking with your mother about her health when her mortality is so tightly fixed to it is hard. Looking back now, I was a chicken. Who wants to talk about saying goodbye? I didn’t realize the seriousness of her health situation until much later. I assumed she didn’t speak about her own death, and I didn’t know how to initiate the conversation. We were all in different forms of denial.
At the end of 2012, the doctors said there was nothing more to be done. I don’t think I fully grasped what that meant at the time. I also did not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
My mother was admitted to hospice care (Medicare Hospice Benefits Booklet).
Mom’s Terminal Illness
Nature, in its less than glorious side, took its course rapidly. My mother’s health deteriorated in a few short weeks.
Cancer is a painful disease. The healthcare personnel gave her various painkillers, but even as they did so, we all insanely talked about not wishing to cause addiction. The pain had its own mind.
At various times, my mother’s suffering would be such that she needed to go to the hospital. There, the doctors administered intravenous medications that were faster acting and stabilized her pain level.
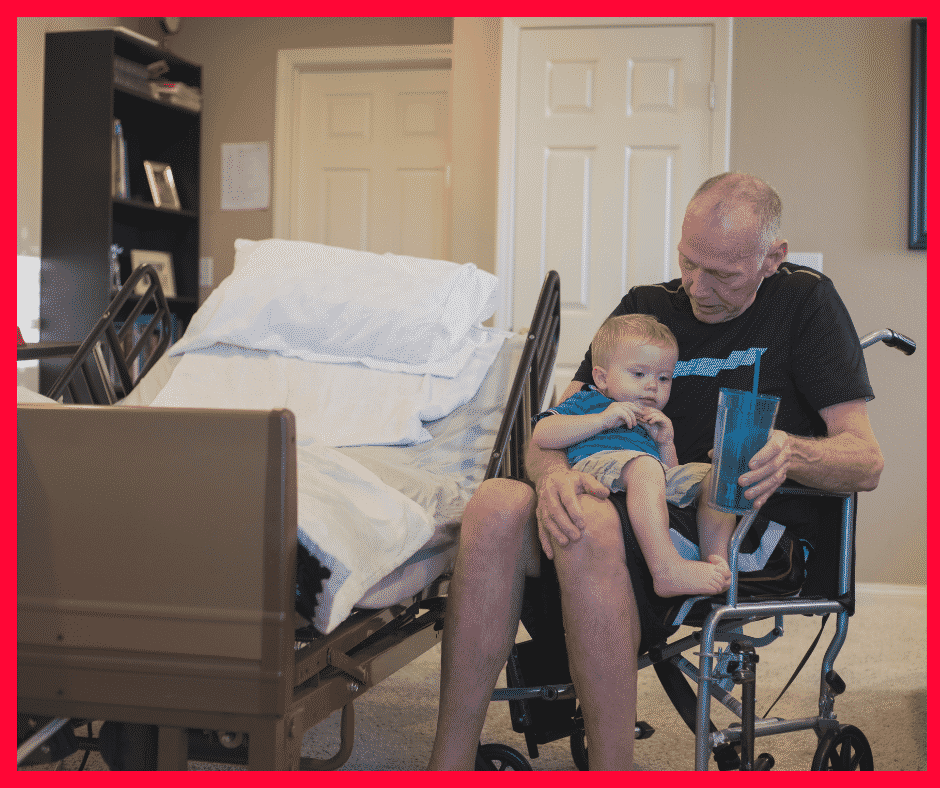
During the last visit, it became clear that we could not care for her at home. My father, John Grimmond–who would pass away six months later–was not physically able to care for our mother. I was in Kansas, my other brother, Tom, was in Sioux Falls, and Paul was in Omaha but busy with his career and family.
My mother needed around-the-clock care. We asked, ‘Does Medicare pay for hospice in a skilled nursing facility?’ The real question was whether Medicare would pay for a skilled nursing facility while my mother died. Strictly speaking, Medicare does not pay for custodial care. Custodial care is bathing, feeding, toileting, etc. Medicare doesn’t cover room and board if you get hospice care while in a nursing home or a hospice inpatient facility. That is out of your pocket.
Qualifying for Skilled Nursing Facility Care while on Hospice
The staff at the hospital initially told us that our mother needed to go to a skilled nursing facility (SNF) because they recognized she required more care than we could provide. They informed us that Medicare would provide and pay for hospice care in the Skilled Nursing Facility, but the cost of room and board and custodial nursing care would not be covered, and they were correct. Medicare coverage for skilled nursing when you are in hospice is tricky.
skilled nursing when you are in hospice is tricky.
The fortunate occurrence, however, was the intravenous nature of my mother’s painkillers. Other than a hospital, you can only receive intravenous medication treatment in a skilled nursing facility. The nature of my mom’s treatment triggered a reason Medicare would accept her being admitted to a skilled nursing facility and pay for it.
Medicare does cover skilled nursing care after a qualifying hospital stay of 3-days or more. Intravenous medication administration also requires a skilled nursing facility. A home health care nurse showing up several times at home would not be adequate. Also, my mother needed physical therapy to improve her strength after the reaction to the pain. From Medicare Part A and Part B, there were sufficient reasons for Medicare to pay for her stay in the skilled nursing facility (SNF) while she was in hospice.
Does Medicare Pay For Skilled Nursing Care During Hospice?
Strictly speaking, Medicare does not pay for skilled nursing care because someone is in hospice, but other triggering events often cause Medicare to cover skilled nursing care.
For example, someone who is in hospice falls and breaks a hip. That situation would justify skilled nursing care. A person develops an infection or pneumonia that results in hospitalization. Then, they qualify for a skilled nursing stay.
How to Navigate the Medicare Coverage Process for Hospice in a Skilled Nursing Facility
 Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
1. The first step is to consult with the individual’s physician to determine if they meet the eligibility criteria for hospice care in a SNF. The physician can provide the necessary certification and guidance through the process. He knows the triggering circumstances that justify a skilled nursing facility stay.
2. It’s important to choose a Medicare-approved hospice provider with experience providing SNF care. They will be able to guide you through the necessary paperwork and ensure that all requirements are met. The health professionals are very familiar with Medicare’s billing codes and protocols for admittance to a SNF.
3. If the individual is already receiving care in a SNF, it’s important to coordinate with the facility to ensure a smooth transition to hospice care. The SNF staff can provide valuable information and support during this process.
4. Familiarize yourself with Medicare’s costs and coverage for hospice care in a SNF. This will help you plan and make informed decisions regarding the individual’s care.
The professionals you deal with know the Medicare rules and the subtleties of maximizing coverage in different circumstances. Listen attentively to their guidance.
Common Misconceptions about Medicare Coverage of SNF During Hospice
Several common misconceptions exist about Medicare coverage for hospice care in a SNF. Let’s address some of these misconceptions and provide clarity:
provide clarity:
1. Medicare only covers hospice care in certain settings: Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, and skilled nursing facilities. As long as the eligibility criteria are met, Medicare will cover hospice care in a SNF.
2. Medicare covers room and board in a SNF. As a rule, Medicare does not cover room and board in a SNF because the individual is receiving hospice care, though room and board may be covered because the patient is in the SNF for reasons other than hospice.
3. Medicare coverage for hospice care is limited to specific conditions: Medicare coverage for hospice care is not limited to specific conditions or illnesses. As long as the eligibility criteria are met, Medicare will provide coverage for hospice care in a SNF for any terminal illness.
4. Medicare coverage for hospice care is limited to a certain time frame: Medicare does not limit the duration of hospice care coverage in a SNF. As long as the individual meets the eligibility criteria, Medicare will continue to cover the necessary services.
Bottomline: Ensuring Quality Care and Coverage for Hospice in a SNF through Medicare
Maximizing Medicare coverage for hospice care in a skilled nursing facility is essential for ensuring quality end-of-life care. By understanding the eligibility criteria, coverage details, and navigating the Medicare system, you can advocate for yourself or your loved one and ensure all available resources are utilized.
Remember, hospice care is a compassionate and holistic approach that focuses on providing comfort and support during the final stages of a terminal illness. Medicare provides coverage for hospice care in a SNF, including room and board, medications, and necessary medical equipment. By staying informed and proactive, you can maximize Medicare coverage and ensure that the individual receives the care they need.
 Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Phyllis Grimmond 1935-2013 R.I.P.
The Bottomline: Benefit Knowledge Makes for Maximum Benefits
At Omaha Insurance Solutions, we understand the importance of access to accurate and reliable information regarding healthcare

Christopher J. Grimmond
decisions. We aim to empower you with the knowledge and resources to navigate the complex world of Medicare coverage. It is important to know that Medicare pays for hospice care in a skilled nursing facility.
By maximizing benefits and ensuring quality care, we can make a difference in the lives of individuals and their loved ones during this challenging time. Call us at 402-614-3389 to ensure you have a Medicare plan protecting you and your loved ones. Speak with an experienced licensed insurance agent profession.
What Are Skilled Nursing Facilities?

All of us have strong memories of visiting the “old folks’ home.” Whether grandparents, relatives, or friends, we recall the smells, linoleum, long hallways, and institutional dormitory rooms. “Old folks’ homes” or nursing homes fall under the category of Skilled Nursing Facilities (SNF). Medicare covers skilled nursing facilities within limits.
Patients go to the SNF after surgeries to recover, from illnesses to heal, and from injuries to recover and strengthen. Skilled Nursing Facilities are for temporary treatment, not long term residential care or custodial care, like memory care. Other facilities, like senior living communities, assisted living, or senior care centers describe other types of facilities that assist seniors.
A skilled nursing facility provides highly skilled professionals, such as occupational therapists, physical therapists, registered nurses, speech therapists. The advantage of an SNF is these professions are available 24 hours a day for the patients. The level of care is very high but short term.
Post-Acute & Skill Rehab Services
 Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Medicare covers skilled nursing facilities within specific parameters. Nursing home care is for individuals who have reached a point in life when they can no longer perform activities of daily living. This is referred to as custodial care. In other words, they cannot bath, feed, and dress themselves. Medicare will not pay for those services to be provided exclusively.
Skilled Nursing is for after surgery or acute illness, for example, hip surgery for a fractured hip or a stroke. A skilled nursing facility admits patients for a short period of time after being in the hospital to aid in their healing and/or rehabilitation. Hospitals are incredibly expensive, and a skilled nursing facility can provide the necessary treatment at a lower cost.
Medicare Criteria For Skilled Nursing Facilities
The tricky part about skilled nursing facilities is admittance. A skilled nursing facility requires patients to meet certain essential criteria for admittance and for Medicare to pay. This is the complex checklist:
- The patient must be admitted to a hospital as an “inpatient” for at least three consecutive days, not including the day of dismissal. She can’t be in the
 hospital for “observation” for it to count for Medicare to pay.
hospital for “observation” for it to count for Medicare to pay. - Medicare mandates patient admittance to the skilled nursing facility within 30 days of discharge from the hospital. If problems arise later—past 30 days—the patient cannot go to the skilled nursing facility and have Medicare pay for it.
- Only a skilled nursing facility can provide the type of care necessary for the patient’s recovery. A skilled nursing facility would provide intense physical therapy for a hip injury or occupational therapy after a stroke. Going to the physical therapist’s office a couple of times a week would not be sufficient in those cases.
- A doctor, or appropriate medical professional, must certify that skilled nursing care is required for recovery.
- The patient must be treated for the same condition for which she was in the hospital.
There are nuances and exceptions to some of these rules. The list gives you a good idea about how skilled nursing fits into your Medicare health insurance. The Omaha, NE area has many quality Medicare certified facilities, and You can find them on the Medicare.gov website.
Sheep get sheared. They follow the other sheep into the pen, down the shoot, then in to the hands of the shearer and are fleeced. The ram is a alert. He doesn’t go with the flow he leads the way and butts heads when he is force to go where he doesn’t want to go.
How do people pick their Medicare supplement plan and company? They talk with their buddy on the left and their buddy on the right. ‘They both can’t be wrong.’ Everyone says Plan F is “the best.” “I never have to pay anything”—no co-pays. That’s great! Sign me up. That is the thought process of the sheep. Insurance companies love it. Insurance agents love it. Plan F is the most expensive plan in all kinds of way.
There are ten possible Medicare supplement plan types that an insurance may offer–A–N. In reality, they usually only offer 4 or 5. Plan F is the most popular as well as the most expensive. Insurance companies and agents like that because it brings in the most money and pays the highest commission. But is it the best for a client?
Plan F does cover all the deductibles and co-insurance that Medicare doesn’t cover. That is nice, but you pay a price for that convenience. It raises the question whether Plan F is the best.
Is there an alternative? How about Plan G? Plan G is very close to Plan F. The difference is that you pay the Part B deductible of $147. It is a one-time annual deductible. Once you pay your Part B deductible of $147, for let’s say a doctor’s visit, you are done for the year. Everything else will be covered 100% which is similar to a Plan F. So why plan G? Because the premium is lower—quite a bit.
Let’s do some simple math. Let’s say that a plan F is $150 per month for a 65 year old male and a plan G is $110 for the same person. The difference is $40 per month and $480 per year less for the Plan G. Subtract the $147 Part B deductible, and you are still ahead $333. Putting it another way, you are paying $333 for the convenience of having the insurance company pay your Part B deductible so that you don’t have to write a check IF you go to the doctor or have some other procedure. Multiply that times 10 years and you are at $3,330.
The second and more important consideration about Plan G is that the rate increases are smaller and less frequent. Yes premiums go up because medical costs go up, but the unusual reality about Plan G policy holders is that they generally do not go to the doctor or emergency room as frequently as Plan F policy holders. There is something about the $147 deductible that causes people to pause and think. ‘Is this really medically necessary?’ The result is that, because Plan G policy holders do not over use medical benefits to the extent Plan F policy holders do, the claims and cost are not has high. Consequently the rate increases for Plan G’s are fewer and smaller than Plan F. Plan F is the best?
Don’t be a sheep. Don’t follow the herd. Stop and look at the different plans. Ask yourself the hard question in light of the facts whether Plan F is the best. Do some analysis, and you will save money in the short, long, and longer run.
 402-614-3389; [email protected]
402-614-3389; [email protected]
 Most people show up at the steps of Medicare without any idea about how to buy Medigap insurance. If they have health insurance company A at their work, they call up health insurance company A and buy their Medigap insurance from company A. They don’t shop, and most pay more without getting more.
Most people show up at the steps of Medicare without any idea about how to buy Medigap insurance. If they have health insurance company A at their work, they call up health insurance company A and buy their Medigap insurance from company A. They don’t shop, and most pay more without getting more.
Amateur Or Professional?
A few years ago, a friend of mine told me that he was going to finish off his basement himself. His wife wanted it done because she was going to host her large family for Thanksgiving that year. Tom thought he could save some money by doing it himself.
himself.
He figured out a design, went to the hardware store, and bought some lumber. It sat there for several months because he got busy with coaching the kids, work, and other projects. His wife got on him because there was a deadline. He started the project, but because he wasn’t an experienced carpenter, he made a few mistakes. The mistakes started adding up.
Mistakes are expensive. The deadline was looming. Finally, he called in a professional. The basement was done in six weeks, just in time for Thanksgiving. He also realized that the basement was much nicer than what he could have done.
What does this have to do with how to buy Medigap Insurance?
How Do You Find The Lowest Price?
A true insurance professional will show you how to buy Medigap insurance at the lowest cost for the coverage you want. He will have the knowledge and experience to better serve you than doing Medigap insurance yourself, visiting with a friend of a friend who does Medigap insurance part-time, or talking to someone in a call center thousands of miles away.
The benefits of working with an experienced and independent local Medigap insurance professional are that he or she understands the laws and regulations around Medicare in that state and county. The Medicare Handbook is over 150 pages. It takes a while to absorb all the regulations, and that is just from Medicare. Each insurance company has its underwriting guidelines, policies, and procedures. In other words, buying Medigap insurance is complicated.
And all of these organizations are run by humans, and humans make mistakes—lots of mistakes. Have you ever had an insurance company make a mistake that affected you? I’ve seen a few, and an experienced Medigap insurance agent can quickly and easily help you resolve snags that inevitably will arise when you’re trying to figure out how to buy Medigap insurance.
How Do You Buy Medigap Insurance With So Many Choices?
Showing you how to buy Medigap insurance means shopping for Medicare supplements and plans for you. In Nebraska or Iowa, there are over 30+ insurance companies offering hundreds of supplements, 20 Medicare Part C Advantage plans, and 28 Medicare Part D prescription drug plans, which all interact with Medigap insurance.
That is a tremendous amount of information, and prices and information are not easily available to persons not licensed and appointed with Medigap insurance companies. A truly independent agent will be able to show you all the plans and pricing, not just one company with a few plans or a handful of cherry-picked companies. Using sophisticated software, he or she can line up the Medigap insurance plans in your area down to the zip code, showing you how to buy Medigap insurance.
A Plan G is a Plan G
A dirty little secret that most people do not know is all the Medigap insurance plans are the same. By law and regulation, the plans are exactly the same. 
“It’s important to compare Medigap policies since the costs can vary between insurance companies for exactly the same coverage . . . .” The Official U.S. Medicare Handbook: Medicare & You
A Plan G is a Plan G is a Plan G. The only difference is the price. An independent Medicare insurance broker should be able to line up all the Plan G’s and Plan N’s in a row from the least expensive to the most for you to see. How to buy Medigap insurance should be straightforward.
Lowest Price vs. Biggest Brand
While brands are not unimportant, saving money is more important. Some companies trade on their name. You pay more, but the Medigap insurance you buy does not cover anymore, pay any faster, or do anything extra.
There are other things to consider when you think about how to buy Medigap insurance. You will hopefully be using Medicare for twenty or thirty years. Picking a Medicare plan is not like getting a tattoo. It is not a one-and-done thing. Each year Medicare makes changes in rules. Medigap insurance policies go up in price because of age or rate increases. The insurance companies are constantly adjusting plans based upon Medicare, markets, inflation, pharmaceutical companies, etc.
Medigap Age & Rate Increases
How to buy Medigap insurance should also consider the history of age increases to the policy and rate increases. For an insurance company to stay alive, not to mention be profitable, it must be able to adjust its prices. The two ways an insurance company adjusts are through age and rate increases. An independent Medicare insurance broker should be able to show you the age increases. In other words, what will your Medigap insurance policy be at 66, 67, 68, etc.
An independent Medicare insurance agent should also have access to the history of rate increases. Some companies will increase their rates each year a little bit. Other companies will wait a couple of years. Those increases can be quite large. Either way, the price will go up. While past performance does not guarantee the future, you still get an idea of how any insurance company handles prices and inflation. With inflation over 4% this quarter, prices will definitely be going up.
How To Buy Medigap Insurance?
An experienced and independent agent lives in this world and can guide you through the changes to supplements and plans that are most beneficial to you. She can shop Medicare supplements each year and show you how to buy Medigap insurance at the lowest price.
New people are constantly recruited to sell Medigap insurance. Some last a few days, a few months, or a few years. Most do not last at all. The Medicare rules are confusing and unforgiving. Insurance companies follow strict underwriting guidelines and are constantly changing prices. Do you really want to do it yourself or entrust yourself to an amateur?
A Professional Will Show You How to Buy Medigap Insurance
The insurance companies will not give you a discount for going direct. When you do that—and the insurance companies love that—your agent is now whoever answers the 800-number you call. You will speak to a different person each time. That person may be in the insurance industry for two days, two months, or two years. You’ll never know. Or would you rather have an experienced and independent local insurance professional who will be your advocate for the next twenty or thirty years, to help you learn how to buy Medigap insurance? He can show you how to buy Medigap insurance at the best price for you.
for two days, two months, or two years. You’ll never know. Or would you rather have an experienced and independent local insurance professional who will be your advocate for the next twenty or thirty years, to help you learn how to buy Medigap insurance? He can show you how to buy Medigap insurance at the best price for you.