Medicare RegulationsCategory:
If you have paid payroll taxes (FICA) for 40 quarters (or 10 years), you are eligible to apply for Medicare in Nebraska for 2022. You are eligible for Medicare Part A at zero premium and may purchase Part B at the current cost if your income is below the IRMAA (Income Related Monthly Adjustment Amounts) amounts.
The Easy Way To Apply For Medicare in Nebraska For 2022
If you are currently receiving Social Security benefits, you will be automatically enrolled in Medicare Part A for the hospital and Part B for doctor visits and outpatient services. You will then be given the option to cancel Part B if you wish.

You cancel Part B by signing the red, white, and blue Medicare card on the back and mailing it back to Medicare. Otherwise, Medicare Part A and B will start on the effective dates printed on the bottom right corner of the card. The Social Security Administration (SSA) will also start deducting the Medicare Part B premium from your monthly Social Security check.
Applying for Medicare in Nebraska in 2022 is easy that way. It is automatic. The other way is more challenging.
Online Application For Medicare in Nebraska for 2022
Applying for Medicare in Nebraska, Iowa, and throughout the country has become more difficult and complex with each subsequent month. The pandemic pushed the process almost entirely online. Social Security personnel were absent at Social Security Administration Offices throughout Nebraska, Iowa, and the whole country during that time. Offices were closed, and most employees were working remotely.
Identity theft, cyber security, and HIPPA regulations have pushed the Social Security Administration (SSA) to add more and more levels of security to the Medicare application.
I help my prospective clients apply for Medicare all the time. While eligibility for Medicare and Social Security benefits in Nebraska begins at 65, most people are not getting their Social Security benefit checks until much later. Instead, they are waiting until the full benefit age, which is around 66 and 8 months or older. So they need to apply for Medicare online.

I probably average helping five people a week apply for Medicare in Nebraska and Iowa. The level of difficulty each person experiences is amazing. I don’t know how other people do it on their own.
How Do You Apply For Medicare Benefits in Nebraska Online in 2022?
If you are eligible for Medicare in Nebraska, type ssa.gov into your address bar. Do NOT Google ssa.gov. You will end up at all kinds of websites trying to sell you Medicare plans. The Social Security Administration logo will be in the top left corner if you are successful.
Click on Menu in the top right section of the website. Go under Benefits and click Medicare. Then, scroll down the page until you see a bright blue button that says “Apply for Medicare Only.” Click on the button that will take you to a page with a gray button that says, “Start New Application.” Click it.
Follow the prompts. The most crucial part is your My Social Security login. This is the tricky part.
Hundreds of people swear they never set up an online Social Security account. Then, when we start the enrollment process, we discovered they have a My Social Security account, and SSA requires us to use it.
Logging in to your My Social Security account may become an insurmountable obstacle if you need to provide personal verification information, like the answers to the three security questions you had set up previously. At that point, you will be stopped out and need to call or go to the Omaha, Lincoln, or Council Bluffs Social Security Administration office to get access to continue applying for Medicare in Nebraska in 2022.
If you do not have an online My Social Security account, you create one. In creating the account, you will need immediate access to email and text. With that, you will be able to set up an online account.
Follow the prompts to set up the account.
Second Form of Identification When Applying for Medicare in Nebraska for 2022
Giving SSA a second form of identification, such as your driver’s license, is vital. SSA will text a link to your phone. Then you take a photo of your driver’s license to verify who you are. Taking the photo so the system receives it can be problematic. This is the most difficult part of applying for Medicare.
Your phone’s camera software may not work well with SSA’s system, the cellular or internet connection may be weak, or the SSA system may be in a bad mood that day. Many factors can go into making the system unworkable. Be warned.
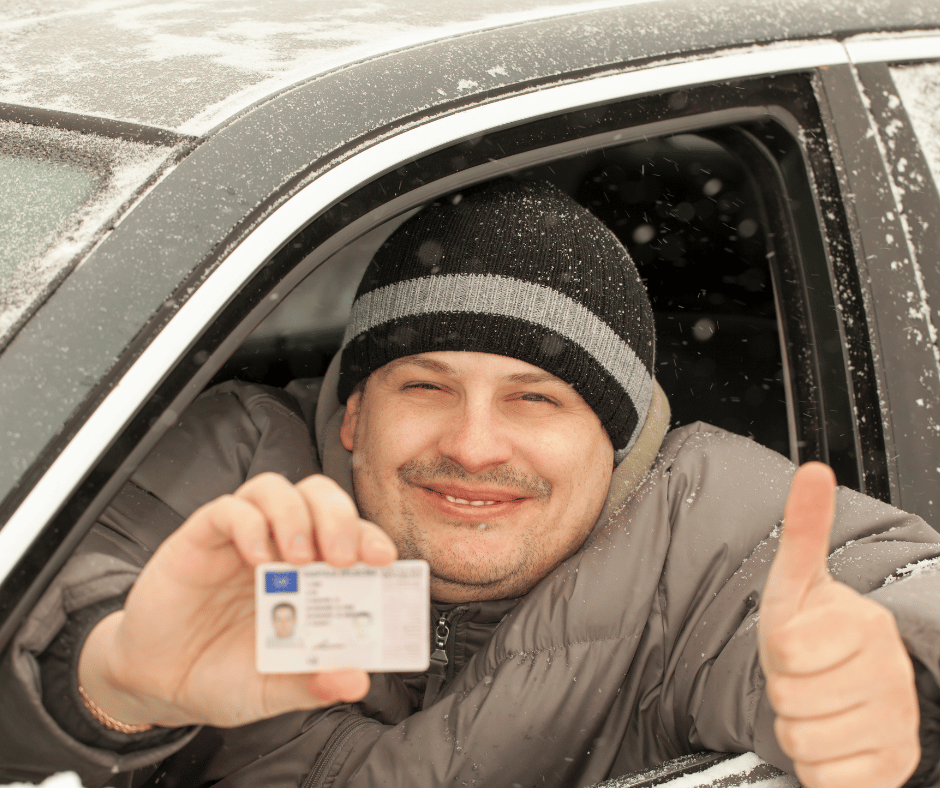
If you cannot set up a second means of verification, you will probably have to wait for a verification code to be mailed to your physical address. Then you go back in to complete the enrollment process.
More than half of the time, the system works. We get the text verification and complete the My Social Security online account setup.
When you enter your My Social Security online account through the Medicare prompts, the system pulls up the application for Medicare. Fill in the details and complete the application. The application process will assume you want Medicare Part A for the hospital since it is free. The system will ask if you want Medicare Part B for doctor visits and outpatient procedures. Medicare Part B costs something. You have the option to say yes or no.
Check On Your Online Medicare Application
When you have completed the application, you can go back in and check on your Medicare application status. A newly created box is in your My Social Security account for Medicare. There will be three grey horizontal bars going across the page. When you complete the application, one bar will be blue. When all three bars are blue, a comment underneath will say you are approved. Congrats!
Above will be a “Verification of Benefits Letter” link. Click on the link. A letter will open up. In the body of the letter will be your Medicare number (MBI), which is made up of eleven digits consisting of a combination of numbers and letters. The letter will also have the dates when your Part A and/or Part B will start.
Sometimes clients tell me they want to wait for the Medicare card to come in the mail. Bad decision. It may take over a month for your Medicare card to show up in the mail, significantly decreasing your time to select, enroll, and get your medical cards from the insurance company before your start date.
Online Medicare Application Problems
Check your account two weeks after you apply for Medicare online, and keep checking it until you have a Medicare number.
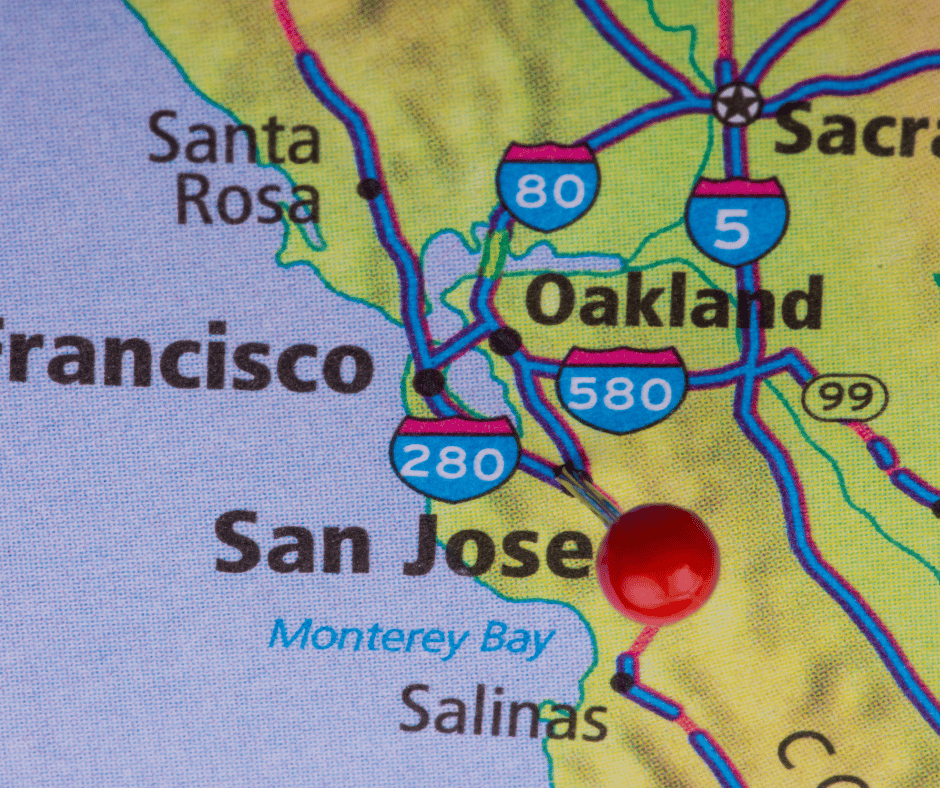
If your account says your case was sent to Salinas, CA, for processing, you need to call your local SSA office to find out why. Salinas, CA, is a black hole.
There is a problem with your application that needs to be solved sooner rather than later, and the folks in Salina, CA, are not very proactive or even active in solving your problem–whatever it may be.
All of this above-said information works if your personal information is in good order with SSA. There may be problems of which you are only aware once you enroll. For example, your name is misspelled with SSA, your birthday is wrong, your address is out-of-date, your maiden name was not changed to your married name or back after a divorce, and your naturalization date or number is incorrect. You could also be flagged as a terrorist, Russian mole, or affiliated with the opposing political party–just kidding.
I’ve experienced all of these with clients–except the terrorist one. Making corrections takes lots of time. I had a gentleman born at a Japanese civilian hospital instead of the U.S. military hospital on the base where his father served, which created a whole set of problems that plagued him throughout his life.
Getting the correct documentation takes time if it can be found. Then SSA takes time to verify the documentation and may ask for more. Then there is the processing time, which could result in you missing your intended start date. That is why you start applying for Medicare in Nebraska as early as possible in 2022.
Calling the SSA Office
You, of course, can call the SSA office or stop in to apply for Medicare in Nebraska for 2022. If you contact them too early, they will not talk with you. Too early is more than 3 months before you turn 65. Then, when they talk with you, SSA generally will set the appointment a month or two later, so you are right up against your birth month and start date. This will work if there are no problems and everything else works smoothly, but this situation usually causes anxiety for most people.

My Experience Helping Clients Apply for Medicare
I’m an insurance agent. I am not an employee of the SSA, but I feel like an unpaid auxiliary staff member. My clients need help, so I’ve learned to navigate the SSA Medicare enrollment system through trial and error. It is a system that is continually evolving.
I’m happy to help my clients. The process creates a tremendous amount of empathy for my clients for what they have to go through. Not only are they confused with all the information and choices that come with going on Medicare, but they have a government bureaucracy that is an unfriendly and confusing obstacle to overcome. I try my best to help and give encouragement when I can’t do specific tasks for them, like finding an original birth certificate with a raised seal.
As the bugs get worked out of the SSA/Medicare system, and Medicare beneficiaries become more tech-savvy, the process for applying for Medicare in Nebraska for 2022 will become more efficient–I hope.
Until then, use this guide to navigate and find your way to the end of the Medicare application maze.
What Does A Medicare Insurance Agent Do?
When you sign up for a Medicare plan or Medicare supplement, you use a licensed insurance agent. An agent is a person who acts on behalf of someone. That someone may be the client or he may be the insurance company. He is licensed which means that the state certifies he has passed some basic testing and has rudimentary knowledge about insurance that allows him to represent a company or person. Medicare insurance agents come in many different types. What type of Medicare insurance broker is near you?
 What Is A Captive Medicare Insurance Agent?
What Is A Captive Medicare Insurance Agent?
A captive Medicare insurance agent is the opposite of an independent Medicare insurance broker. He has a contract to represent one insurance company. He is not an insurance broker. Depending on the level of captivity, he must sell a certain amount of the company’s insurance products to remain an agent and continue to receive renewal commissions. He may or may not be able to sell any other insurance company’s products.
The difficulty with dealing with a captive agent who offers Medicare insurance products is a lack of selection and objective evaluation. He will probably say his products are “the best!” However, you have no way to compare and evaluate based upon the product information he shares. He is a one-trick pony. Physician Mutual agents. Blue Cross Blue Shield of Nebraska Agents.
From what clients have reported to me, many captive agents do not honestly represent themselves as exclusively with one company. They lead prospective to believe they can represent many companies when that is not the case. Some captive agents do not disclose they are in fact captive.
What Is A Medicare Supplement Insurance Agent?
Some agents sell almost exclusively Medicare supplements or Medigap policies. For those who sell over the phone, Medicare Supplements are the only Medicare products they can sell because of very strict regulations around Medicare Advantage and Medicare Part D. Medicare rules and regulations prohibit unsolicited calls to consumers about Medicare Advantage.
and regulations prohibit unsolicited calls to consumers about Medicare Advantage.
 Consequently, these agents sell against Medicare Advantage constantly. They point out weaknesses in the product–whether real, exaggerated or imagined. Medicare Supplements are the best, of course, because they cannot offer an alternative.
Consequently, these agents sell against Medicare Advantage constantly. They point out weaknesses in the product–whether real, exaggerated or imagined. Medicare Supplements are the best, of course, because they cannot offer an alternative.
With auto-dialers, Med Sup agents dial 10 to 15 prospects simultaneously. Call centers in Florida, South Carolina, and California carpet bomb the U.S. with millions of phone calls each day. During Annual Election Period (Oct. 15th–Dec 7th), the Med Sup call centers recruit a bunch of agents for the season. You will probably never talk with the agent again after he signs you up.
Other agents who sell Medicare Supplements exclusively face-to-face are controlled by agencies, managers, or marketing groups. If they sell a lot of one or two companies, their commission is higher. They can win sales trips abroad and bonuses. That is the motive behind their exclusivity. They are not truly Medicare insurance brokers.
What Is A Medicare Advantage Insurance Agent?
Some agents sell just Medicare Advantage plans. They are likewise semi-captive to an insurance company that feeds them leads. The insurance company may have a large market presence. Lots of consumers call in because they are familiar with the brand name and trust it. They enroll in the Medicare Advantage plan over the phone or online with an insurance agent at the company.
Some people, however, want to talk with a live person. The insurance company will send an agent out to the person’s home to explain the product in greater depth and enroll them in person. The agent, however, is obliged to just offer that company’s products in the most favorable light and not the competition. That is why the insurance company supplies the leads to the agents. These are not Medicare insurance brokers.
Independent Medicare Insurance Brokers Near Me
Independent Medicare brokers represent both sides of Medicare–Medigap policies and Medicare Advantage. Independent Medicare insurance brokers represent multiple companies, not just a hand full. He should be showing quotes and brochures from many different insurance companies.
Insurance companies that offer Medicare Advantage pay the agent the same amount, so there should be no preference based upon commission. An independent agent should receive the same percentage on the supplement side as well.
Medicare insurance brokers are only paid when you are a client. To keep you a client, you need to remain a happy client. A conscientious independent insurance agent should keep in touch and make sure his clients are happy with their current Medicare plans and change them when not.
Local Broker Vs. Call Center Agent
When you turn 65, that is when you first become Medicare eligible. You will be inundated with mail, phone calls, and even door knockers trying to sell you some Medicare insurance product. I hear complaints from my clients all the time about the oodles of phone calls and the blizzard of junk mail. They need to go into witness protection to avoid the solicitors.
all the time about the oodles of phone calls and the blizzard of junk mail. They need to go into witness protection to avoid the solicitors.
Most solicitations will come from persons you will never meet. You do not know them. They are strangers calling from far away states. They may have been insurance licensed for only a year, a month, or just a week. The average insurance agent doesn’t last in the business even a year.
Do you want to share your personal information over the phone with a complete stranger? Someone you will never meet in person.
There is something reassuring about dealing with someone who is established in the local community. Proven. They will not disappear in a month. Connected to people and institutions you know. At least a Cornhusker!
How to Find Medicare Brokers In My Area?
You can use Google to find Medicare insurance brokers. Google seems to know everything. It is not a bad start.
An agent’s website gives you a feel for the agent and agency. Blogs and videos demonstrate his knowledge and expertise–or the lack.
Google reviews from clients–hopefully not family and friends–give some proof of professionalism and quality of service. Google is a 3rd party, so the reviews are not cherry-picked.
Referrals are another way. Most of my clients now come from my existing clients. So ask a friend, but check the person out. Go to the Better Business Burea and check the rating. Again, visit the website.
One new client told me she was at a work function. She’s employed in the healthcare field. Three other ladies–fellow nurses–were chatting around a table. She mentioned she was turning 65 and going on Medicare. She complained how the endless phone calls and junk mail made the whole process a headache. Immediately the three nurses volunteered “their Medicare guy” to her to help solve the dilemma. All four were surprised when they realized I was the Medicare agent for each of them.
 How to Choose An Independent Medicare Broker Near Me?
How to Choose An Independent Medicare Broker Near Me?
The most important criterion I believe is experience. Being in the insurance industry, I have seen hundreds of agents come and go since I became an agent back in 2003. Like anything–stock trading, medicine, law–you need practice. While it may be very nice to help out a friend or nephew who is getting started in the business, your health insurance is a serious matter. You want a professional handling your money, your body, and your assets to have time in harness.
Let the market pick your Medicare broker. If the agent makes lots of people happy with his work, he is successful and stays in the business. Time in service with lots of clients is the first key.
While my doctor is younger than me for the first time, she didn’t just get out of medical school. I know she had a lot of practice before I showed up. I think Medicare insurance brokers near you need to have lots of years in the business and lots of clients. That way they are not practicing on you, and they will be there for you for years to come.
Again, visit their website, read their materials, list to their presentation. It is like listening to good or not so good music. After a while, you can tell whether it rings true.
 Needed Changes to the Medicare Enrollment Process 2022
Needed Changes to the Medicare Enrollment Process 2022
I have been a licensed insurance agent since 2003. I’ve seen a lot of changes to Medicare over that time. One of the problems that always baffled me was how difficult it was to enroll in Medicare. Let me put you in the front seat of the upcoming changes to Medicare for 2022 and 2023.
Non-Stop Complaints About Medicare
More than 11,000 persons turn 65 each day and become Medicare eligible. That is a lot of people enrolling in Medicare. The problem that Congress created a number of years ago was moving the full Social Security retirement age from 65 to 66 and so many months.
People are also living longer. Retirement is being pushed off because people don’t have enough saved. Consequently, many continue to work past 66 to just survive, so they remain on their employer’s group health plans. But, when they turn 65, they need to do something about Medicare enrollment.
How to Enroll with Upcoming Changes to Medicare in 2022 & 2023?
When you start your Social Security, Social Security enrolls you automatically into Medicare Part A and Part B when you turn 65. You have the option then to decline Part B. Many do if they are still working and have adequate health insurance from their employer.
Many people are not taking Social Security at 65, so Social Security does not automatically enroll them in Medicare. That number is even smaller than a few years ago.
So, people must actually choose to enroll in Part A at 65. If they are going on Medicare entirely and delaying Social Security, they must actively choose to enroll in Part A and Part B. A lot of people call Medicare complaining because of how hard it is to enroll in Medicare. Upcoming changes to Medicare in 2022 and 2023 will make the enrollment process simpler.
 Enrolling in Medicare at The Social Security Administration Office
Enrolling in Medicare at The Social Security Administration Office
Enrolling in Medicare is a challenge, to put it kindly. I do this for a living. I like to think I have above-average intelligence and some good computer skills. However, I still find the Medicare enrollment process unnecessarily difficult and complicated.
Before the pandemic, you could go to your local Social Security office to enroll in Medicare. Depending on the office’s busyness and the staff’s competency, it was more or less complicated and very time-consuming. The primary issue was the time involved—driving to the office, waiting in line, being at the office during regular business hours when you are still working. Those were the usual challenges. As of the writing of this, the local Social Security offices are closed to visitors because of COVID. The only option now is to enroll online.
Apply For Medicare Online Only
The other option for enrollment, which has become pretty much the only option now, is enrolling online. Enrolling online is not easy, even if everything goes smoothly.
In the past two years, the online process has evolved. A few months ago you took a photo of your state driver’s license. Social Security scanned your license into their system through your smartphone. The purpose was to identify you if you did not already have an active MySocialSecurity account. It was not a bad improvement over the old way, which was answering credit questions. That was an amazing bureaucratic mess in itself. I’m glad the credit questions are gone, but the technology for taking the photo of the driver’s license was faulty.
The latest method is a combination of email and text confirmation codes. This method works if there are no issues with your personal information.
 The major challenge with this newest method is some of my clients do not have email or do not get emails and texts on their phones.
The major challenge with this newest method is some of my clients do not have email or do not get emails and texts on their phones.
Challenges, however, go beyond just the mechanics of getting enrolled with Medicare. The problems are with when you can enroll, penalties when you don’t follow the rules, confusion about the rules, and penalties that are imposed as a result. Frustration has built over time as more and more baby boomers run into the wall called Medicare enrollment.
Someone must have heard that consumers were not happy because Congress made some significant changes to the Medicare enrollment process for 2022 and 2023.
What Are the Upcoming Changes to Medicare for 2022?
In December 2020, Congress passed the Beneficiary Enrollment Notification and Eligibility Simplification (BENES) Act of 2020. Parts of this legislation will be effective beginning in January 2023.
The changes are in five areas:
- GEP (General Election Period)
- Part B Enrollment Exceptions
- IEP (Initial Enrollment Period)
- Advanced education for Medicare enrollment
- Expanded Kidney transplant patient coverage
What Are Medicare General Enrollment Period Changes For 2022 & 2023?
Sometimes people miss their Initial Enrollment Period (IEP), which occurs when they turn 65. If you do not have health insurance from 65 onward, you cannot enroll in Medicare until the General Election Period (GEP), January 1st—March 31st. The delay is part of the punishment for missing your IEP. You may also incur the 10% permanent late enrollment penalty.
The problem with the rules around GEP is that Medicare Part A and/or Part B does not start until July 1st after you enrolled sometime from January 1st–March 31st. Consequently, a person cannot get a Medicare Supplement or Part D plan until then. Medicare Part C/Medicare Advantage plans are delayed even further until Annual Election Period (AEP) in October. You are without comprehensive health coverage for many months after an already delayed enrollment.
The BENES Act changes GEP (General Election Period). Congress moved GEP from the first three months of the year to the last three months of the year—October 15th—December 31st—to coincide with the Medicare Annual Election Period (AEP), which is October 15th–December 7th. The hope was to reduce confusion and enable a newly enrolled beneficiary to get maximum coverage right away. For example, if you enrolled in November during the GEP, your Medicare would start on Dec 1st.
 Medicare Changes in 2022 Allow For More Exceptions
Medicare Changes in 2022 Allow For More Exceptions
Medicare enrollment periods are very restrictive and precise. The handbook that agents must learn runs to many pages for Medicare election periods when someone can enroll in Medicare or make changes to a Medicare plan. Often I cannot enroll someone in a plan or change their plan, even when the situation is terrible, because of the restrictive enrollment election criteria.
The new law allows the Secretary of Health and Human Service to initiate a particular enrollment period for Part B when exceptional circumstances arise. Of course, we all can think of the pandemic as the perfect example.
The Last 3 Months of The Initial Enrollment Period
Many people know that your Initial Enrollment Period (IEP) is three months before the month of your birthday, the month of your birthday, and the three months afterward. What people do not realize about this rule is there are additional rules for the last three months. This provision has been the bane of my existence—as well as a few clients—for years.
Staggered Medicare Start Dates Change in 2023
Sometimes people will delay enrolling in Medicare when they turn 65 to coincide with a spouse turning 65, a retirement date, the end of a school year, etc. The problem with enrolling after you turn 65 is the start dates are staggered.
For example, you are turning 65 in July, but your spouse is turning 65 in October and needs you to remain on the employer health plan so she can have health insurance. You want to enroll in Medicare for an October 1st start date so it coincides with your spouse, but you can’t.
If you enroll in August, your Medicare will start in September. If you enroll in September, your Medicare will start two months in November under the current rules. You will need to enroll in Medicare in August, so your Medicare starts in September. Your spouse will enroll during the three months before, so it starts on October 1st. You will need to double pay for insurance for one month because of the unusual Medicare rules.
The upcoming changes to Medicare in 2022 and 2023 do away with the silliness. Joe can enroll in September for October and not have to pay double for health insurance. I can’t tell you how many times this has been an unnecessary burden for my clients going on Medicare.
This change will allow people retiring at the end of their IEP (Initial Enrollment Period) to have a smoother transition from employer coverage to Medicare without a lapse in coverage or double paying.
Medicare Part B after 65
I find that Medicare does not explain very well how Medicare works when you work past 65 or beyond and have an employer health plan. I hear the standard response from Medicare and Social Security bureaucrats. They encourage people to enroll only in Part A and stay on their employer’s health plan as long as they are working.
In the past, that standard answer may have worked, but when more and more people are working past 65 and full Social Security retirement is 66+, reality changed.
Also, employer plans have steadily declined in quality during the past fifteen years. Health plan costs have increased and coverage has decreased significantly. I find the vast majority of employer health plans are inferior to Medicare Advantage or Original Medicare and a supplement.
Medicare Enrollment Deadline & Penalty
The most common issue around Medicare is initial enrollment, which is when people turn 65. Some people claim they didn’t know about their Medicare enrollment. I’m not sure how that is possible because most people’s mailbox is jammed full of mail announcing they are turning 65 and need to get signed up for Medicare.
The real issue around 65 is should I enroll in Medicare, and how do I quickly do that? I find a lot of legitimacy around that question.
The upcoming changes to Medicare in 2022 & 2023 through the BENES Act will include notifying people of Medicare eligibility. The notifications will start at ages 60 to 64. Medicare will send information to explain rules such as Medicare eligibility, timeframes for enrollment, Medicare penalties, delaying Medicare without penalty, Part B coordination of benefits, and other online resources will be included on the notice. The purpose is to alert beneficiaries, so no one misses their opportunity.
If your mailbox was not full enough when you turned 65, it will be stuffed to overflowing now.
Medicare For Kidney Transplant Patients
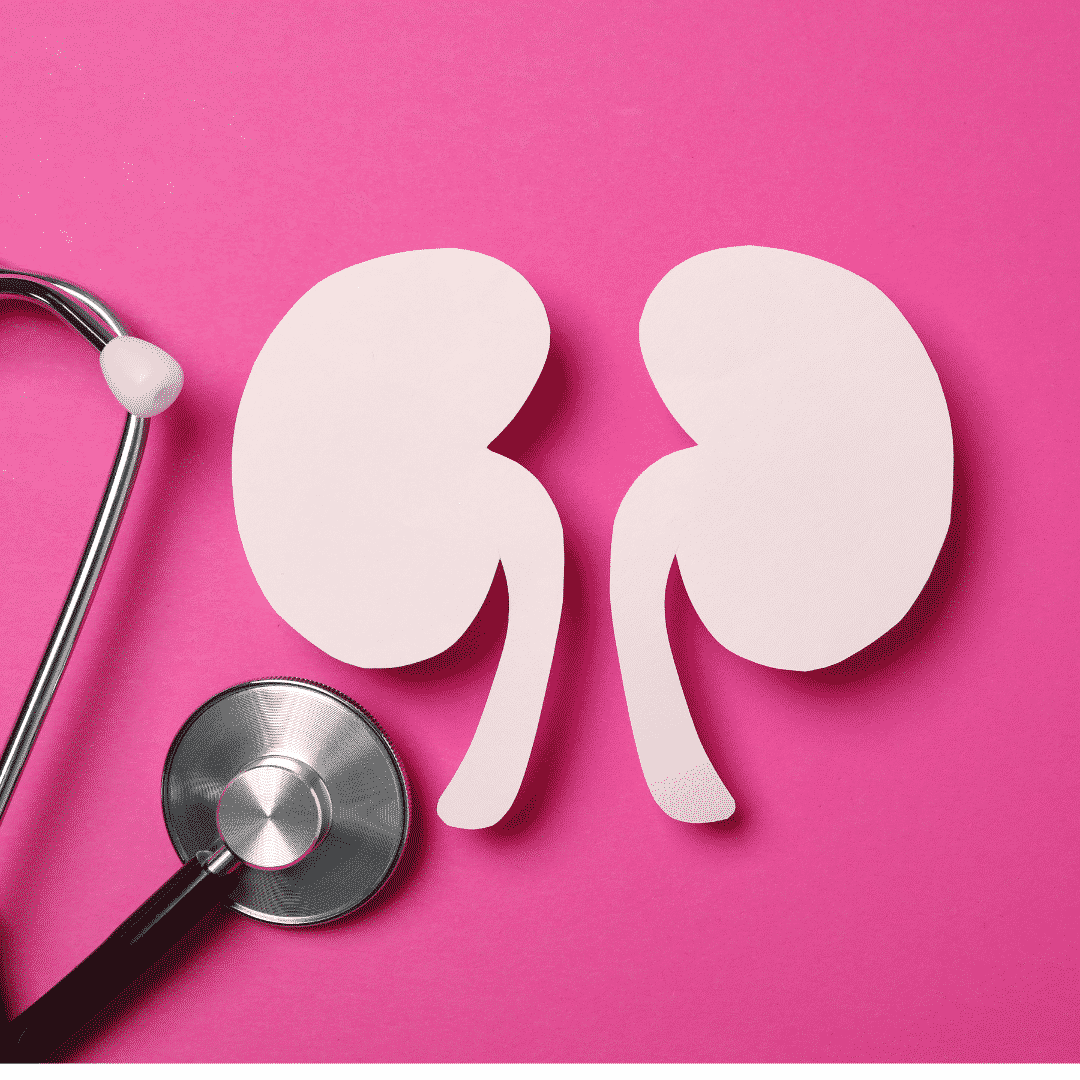 End-Stage Renal Disease (ESRD) is one of the ways you qualify for Medicare before age 65.
End-Stage Renal Disease (ESRD) is one of the ways you qualify for Medicare before age 65.
If you are under 65 and diagnosed with ESRD, you can enroll in Medicare for a specific number of months. For example, now if you qualify for Medicare based on ESRD and have a kidney transplant, your Medicare coverage will end 36 months after the month of your transplant.
The BENES Act of 2020 change will allow kidney transplant beneficiaries to continue their Medicare Part B coverage past 36 months if they have no other health insurance source. The purpose of this is so these beneficiaries will continue to have coverage for immunosuppressive drugs.
According to the Social Security Administration (SSA), Part B’s premium under these circumstances would be less than the base premium and not subject to late penalties.
When Does the BENES Act Take Effect?
The BENES Act will take effect on January 1, 2023, but like many laws, different aspects will be implemented over time to give all the institutions and organizations time to comply.
The two changes I think most important are General Election Period (GEP) and Initial Enrollment Period (IEP). Those will be implemented on the start date–January 1, 2023. The outreach program and kidney transplant patients will take about two years to enact the changes fully.
The number of people enrolling in Medicare is monster. I think all the Baby Boomers enrolling in Medicare have forced politicians and bureaucrats to streamline the Medicare system. Upcoming changes to Medicare enrollment in 2022 and 2023 are going to make life easier. Late enrollment penalties and complaints should decline significantly with the more efficient and user-friendly rules. The most vulnerable, like kidney transplant patients, will have better options.

Christopher Grimmond
Medicare and Medicare insurance, however, is still complicated. When you need help understanding the new BENES rules and all the others, give us a call at 402-614-3389 and speak with a licensed and experienced insurance professional.
55648_051622_MK
 As much information as there is about Medicare, I’m surprised people still do not remember important Medicare dates. The surplus of commercials, mailers, emails, and advertisements probably do more to obscure and confuse people about Medicare enrollment dates. The first Medicare enrollment date to remember is the most important one.
As much information as there is about Medicare, I’m surprised people still do not remember important Medicare dates. The surplus of commercials, mailers, emails, and advertisements probably do more to obscure and confuse people about Medicare enrollment dates. The first Medicare enrollment date to remember is the most important one.
Medicare Initial Enrollment Period
You are first eligible for Medicare at age 65. You can enroll in Medicare three months before your 65th birthday, the month of your birthday, and three months after your birthday. If you do not enroll, a penalty is permanently added to your Medicare Part B premium if you do not enroll.
The penalty is 10% of your current Part B premium added to your Part B premium for the rest of your life. Yes, it never stops. The 10% penalty is for not being enrolled in Medicare each full year when you were eligible. I have client who cannot verify he had employer health coverage for 4 year. Yes, he has a permanent 40% penalty tacked on to his Medicare Part B premium.
There is also a separate permanent penalty for not having a Medicare Part D plan as well.
The exception is if you have an employer health plan that is as good as Medicare. If you do, then you may defer going on Medicare indefinitely without penalty as long as you remain on a qualifying employer health plan. This is the part that many salespeople leave off in the rush to sell you a supplement or Medicare plan.
The Big Medicare Enrollment Date Is Annual Election Period (AEP)
Once you are on Medicare, you have an opportunity to change your Medicare Part D or Medicare Part C/Medicare Advantage plan during Annual Election Period (AEP). AEP that is from October 15th–December 7th each year.
You need this period because Medicare plans change, and your health needs change. You can switch to a plan that better serves your needs during this time. AEP is particularly important for a person on expensive medications.
Part D and Part C plans can drop prescription drugs, move them to higher tiers, or increase their copays significantly. The Annual Election Period allows people to switch to a plan that covers their medications at a lower cost.
Those on Part C/Medicare Advantage plans may be interested in other Medicare Advantage plans that have lower copays and better benefits. The Annual Election Period (AEP) is an opportunity to shift to a better plan.
For those who want to move to a Medicare Supplement from an Advantage plan or go from an Advantage plan to a Medicare Supplement, this is the time for that switch.
Medicare Advantage Open Enrollment Period (OEP)
A couple of years ago, CMS (Center for Medicare & Medicaid Services) decided to create Medicare Advantage Open Enrollment Period (OEP). OEP is from January 1 — March 31 each year; if you’re enrolled in a Medicare Advantage Plan, you can switch to a different Medicare Advantage Plan or switch to Original Medicare (and join a Medicare Part D prescription drug plan) once during this time.
CMS observed that Medicare beneficiaries change Medicare Advantage plans during Annual Election Period AEP (Oct 15th–Dec 7th), but mistakes happen. The biggest mistake is the plan they switched to did not have their doctors in the network.
Other mistakes happened as well. OEP was an opportunity to rectify the situation. It was a free get-out-of-jail pass. You can make one change to another Part C/Medicare Advantage plan.
Or you could ultimately get out of your Medicare Advantage plan and go back to Original Medicare (Part A & Part B) and purchase a Part D plan.
 The Lesser-Known Medicare Enrollment Date Is General Election Period
The Lesser-Known Medicare Enrollment Date Is General Election Period
Another Medicare enrollment date to remember is January 1-March 31 each year for those who missed their initial enrollment period. This is called the General Enrollment Period. Your coverage, however, does not start until the following July 1. You might pay a monthly late enrollment penalty if you don’t qualify for a Special Enrollment Period.
At this time, you may have an open enrollment period for a Medicare Supplement starting in July. You may also enroll in a Part D plan, but you will need to wait until Annual Election Period in October to enroll in a Medicare Advantage plan.
 Special Enrollment Periods
Special Enrollment Periods
There is a myriad of Special Enrollment Periods. One of the most common is when someone is past 65 and 4 months and losses their employer’s health plan. At this time, CMS will allow you to enroll in Medicare Part A and Part B without delay or penalty if you can verify employer health coverage.
Some additional forms need to be completed and submitted to the Social Security Administration. Still, you will be enrolled on the date of your choosing and not need to wait for General Election Period.
Rules & Penalties
Medicare has lots of rules, regulations, norms, and penalties. Some of them are pretty obscure, but there is little to no forgiveness for mistakes or ignorance of the law. If you have questions about Medicare, please call us at 402-614-3389 or check out our blogs and videos on OmahaInsuranceSolutions.com. You can also call Medicare at 800-633-4227 or look on Medicare.gov for information about Medicare enrollment dates to remember.
 Medicare Open Enrollment Is Also Known As Medicare Annual Election Period
Medicare Open Enrollment Is Also Known As Medicare Annual Election Period
Medicare Open Enrollment is when people may make changes to their Medicare plan. Medicare Open Enrollment is also called Annual Election Period or AEP. That is the new official name Medicare Open Enrollment. Annual Election Period (AEP) is when you can change your Medicare Part D prescription drug plan or your Medicare Part C Medicare Advantage plan. AEP is from October 15th–December 7th. A lot of people blow this opportunity. They don’t check to see if they have the best plan for their needs and situation for the coming year. BIG MISTAKE. For some people with serious health issues and medication needs, HUGE MISTAKE!
There are a thousand complaints the day after Medicare Open Enrollment (Annual Election Period), December 8th. People offer a myriad of excuses–It’s the agent’s fault,’ ‘I was too busy to deal with it,’ ‘The dog ate my Medicare card.’ The number of phone calls I get on December 8th is amazing–mostly non-clients. They are hoping to find a Medicare-fairy-godmother to save them from their negligence. Sorry, there is no Medicare-fairy-godmother!
When January 1st arrives and the new plan year begins, people may find out their plan does not cover one or more medications, or the price of one of their drugs went through the roof. Now they have a deductible on their plan they didn’t have before, a medication moved to a higher tier, or their doctor is no longer in-network. Their Medicare situation is a disaster because they didn’t double-check during the Medicare Open Enrollment / Annual Election Period (AEP).
What are the most significant problems created by not reviewing your Medicare plan during Medicare Open Enrollment / Annual Election Period (AEP)?
 Formulary Check During Medicare Open Enrollment
Formulary Check During Medicare Open Enrollment
During Medicare Open Enrollment /Annual Election Period (AEP), insurance companies determine the medications on their approved list of drugs in the formularies that service their Medicare Part D prescription drug plans and the Part C Medicare Advantage plans.
Some years, they drop certain medications altogether. In other years, they might shift the medications from a lower to a higher tier.
The result is you may end up paying more for your prescription drugs. In some cases, a lot more. Checking the formulary and comparing it to the other plans in the area is a straightforward but essential process.
During Medicare Open Enrollment / Annual Election Period (AEP), reviewing medications is a big part of what we do. I sometimes have to arm-twist clients to send me their current list of medications. Some will tell me that they don’t need to do anything because their medications have not changed, but I try to remind them it doesn’t matter. The insurance companies change their formularies.
medications. Some will tell me that they don’t need to do anything because their medications have not changed, but I try to remind them it doesn’t matter. The insurance companies change their formularies.
Over the years, I have had clients neglect their reviews and end up with substantial prescription drug bills as a consequence. Your agent should thoroughly check your medications with dosages each AEP.
 Double Check Physician Directories
Double Check Physician Directories
The Medicare Advantage plan manages your care. That means that an insurance company under the supervision of Medicare is making determinations about your care. As part of that program, they have doctors contracted with the plan. Some doctors and hospitals are not contracted. Doctors may change their credentialing.
may change their credentialing.
It is important to double-check to ensure your doctor is still in-network during Medicare Annual Election Period (AEP) / Medicare Open Enrollment.
We have three medical networks in the Omaha, Lincoln, and Council Bluffs area. The vast majority of medical professionals are part of one or more of these networks. The networks work with the local Medicare Advantage plans. Doctor access is not an issue.
I have clients, however, throughout the U.S., and the other plans are not as generous in the number of in-network medical professionals. Checking the directory to make sure your physicians are still in-network every year is critical during Annual Election Period (AEP) / Medicare Open Enrolment.
 Review CoPays
Review CoPays
With Medicare Advantage plans, copays may change from year to year. This AEP saw very little change among the plans around here. I suspect that was because the plans determined prices in the Spring of the preceding year.
The inflation we are experiencing right now was not a factor in the 2022 planning. I think 2023 will be a different ball game.
Copays can change each year, so you need to review those changes. For example, the cost of MRIs may jump on your plan to the extent you want to change to another plan. Sometimes plans will drop benefits that Medicare does not require, like dental.
I’ve seen plans in the past drop benefits like dental. Beneficiaries don’t imagine their plan could ever change. The lack of coverage and the price tag associated with that shocks clients.
Re-Explain The Donut Hole
 The dreaded Donut Hole or Gap! The Donut Hole is still there. I’ve seen the burden of drug costs lighten for some of my clients, but it is still expensive when people fall into the Donut Hole.
The dreaded Donut Hole or Gap! The Donut Hole is still there. I’ve seen the burden of drug costs lighten for some of my clients, but it is still expensive when people fall into the Donut Hole.
If you are on expensive medications that drive you into the Gap, checking your medications for the level of Gap coverage is essential. While no plan eliminates the cost, some plans are structured, so you pay less than other plans. Some plans delay going into the Gap longer, or other plans even out the cost because of a zero deductible.
If drug costs are an issue for you, look at the various Part D, and Part C plans side-by-side to determine which payment schedule would benefit your wallet during Medicare Open Enrollment.
Have A Conversation About Your Travel Plans
 Many clients on Medicare like to travel. Their grandkids are scattered throughout the country. Friends moved to warmer clients, or getting out of town is just great. Other clients have semi-permanent homes in Arizona, Florida, and Texas. Medicare is a federal program. It exists from sea to shining sea in the U.S. The Medigap policies that company them work anywhere in the U.S. too. (Medicare. however, does not leave the borders of the U.S.)
Many clients on Medicare like to travel. Their grandkids are scattered throughout the country. Friends moved to warmer clients, or getting out of town is just great. Other clients have semi-permanent homes in Arizona, Florida, and Texas. Medicare is a federal program. It exists from sea to shining sea in the U.S. The Medigap policies that company them work anywhere in the U.S. too. (Medicare. however, does not leave the borders of the U.S.)
Medicare Advantage plans, however, are set up for a particular area or region. The HMO (Health Maintenance Organization) plans only include doctors and hospitals in that area. Emergencies are a different matter. Emergency visits are covered anywhere in the country. Some insurance companies with HMO plans also have national networks, so you can still get in-network services and prices outside of your geographic region for ordinary services.
include doctors and hospitals in that area. Emergencies are a different matter. Emergency visits are covered anywhere in the country. Some insurance companies with HMO plans also have national networks, so you can still get in-network services and prices outside of your geographic region for ordinary services.
For those who travel a lot and especially those who stay for long periods away from home, I highly recommend the PPO (Preferred Provider Organization) plans. You may go to doctors and hospitals outside the network as long as they take Medicare. Out-of-network copays may be more, but you have the convenience and security of going anywhere that accepts Medicare.
You can change your Medicare Advantage plan during Medicare Open Enrollment even if you are out of the area. There is email, U.S. mail, text, and even voice signatures.
Changing Circumstances Makes Medicare Open Enrollment Critical
Over the years, I have had client reevaluate their situation during Medicare Open Enrollment or AEP. Those paying enormous amounts in monthly Medigap premium look to switch to a Medicare Advantage plan.
The amount of money they pay in premium very quickly covers any copays. Others anticipate more medical costs as they age, switching to Medigap plans. Medicare Open Enrollment or AEP is the time to review your ever-changing circumstances and adjust accordingly.
Save Money On Medigap Quote Anytime, Not Just During Medicare Open Enrollment
While Medicare supplements are not geared toward Medicare Open Enrollment or AEP exclusively, it is still an excellent time to look at your pricing. Running Medigap quotes only takes a few moments. I can tell you in a minute if you have the lowest price for Plan G or Plan N in your area. We can then make adjustments accordingly.

Christopher Grimmond
Medicare planning is not a one-and-done deal. As you change, Medicare changes and the Medicare plans change. You need to make the adjustments that best fit your needs and circumstances at that time.
Ignore Medicare Annual Election Period (AEP) October 5th–December 7th at your peril or not.
 IRMAA Tax Definition
IRMAA Tax Definition
Many of you may see the letters IRMAA when learning about Medicare. The government loves acronyms. IRMAA stands for Income-Related Monthly Adjustment Amounts. It is based on a person’s modified adjusted gross income (MAGI). The IRS uses a tiered scale. Your Medicare Part B and Part D premium will cost more based upon the income thresholds you cross for that year. How you file your taxes also determines where you fall in the IRMAA brackets and thus the amount you pay. Be conscious of your tax filing status. Married filing separately can have a devastating effect.
I was helping a new client prepare for Medicare a few years ago. His income alone was over $120,000 not counting his wife’s income. She was five years younger and had health insurance through her employer. Her income was quite a bit smaller. The IRMAA brackets were much lower than the IRMAA 2022 brackets now. My client had only crossed the first rung of the IRMAA threshold. His Part B premium was going to be just a little over the Part B premium most people were paying at the time.
He called me a month before his Medicare started. He was almost hysterical because his IRMAA premium was over $400 per month. I said it was a mistake and had him call Social Security.
It turned out not to be a mistake. As the story unfolded, I discovered that he was estranged from his wife. They were still legally married. As a matter of fact, they had been divorced, and he remarried her again.  They lived in the same residence–he lived upstairs and she lived downstairs–but they filed separate tax returns. She absolutely refused to file jointly, and he would not divorce her because of the financial consequences.
They lived in the same residence–he lived upstairs and she lived downstairs–but they filed separate tax returns. She absolutely refused to file jointly, and he would not divorce her because of the financial consequences.
My client fell into the bizarre category of “Married Filing Separately.” You can see on the IRMAA Chart for 2022 what that does to the premium. Even the lowest income earner on the IRMAA chart pays the same premium as the highest earners!
After decades in the insurance industry and thousands of clients, you eventually see everything!
He canceled his Medicare and stayed on his employer’s health plan that was terrible coverage rather than pay the IRMAA Medicare tax.
IRMAA rules are the same if you are on Original Medicare with a supplement and Part D plan or a Medicare Advantage plan. The Medicare tax is imposed on all Medicare benefits whose income is above the tiered IRMAA limits. IRMAA affects 5% of Medicare beneficiaries. IRMAA 2022 rates went up significantly from IRMAA 2021.
IRMAA Brackets for 2022
| your yearly income in 2020 (for what you pay in 2022) was | You pay each month (in 2022) | ||
|---|---|---|---|
| File individual tax return | File joint tax return | File married & separate tax return | |
| $91,000 or less | $182,000 or less | $91,000 or less | $170.10 |
| above $91,000 up to $114,000 | above $182,000 up to $228,000 | Not applicable | $238.10 |
| above $114,000 up to $142,000 | above $228,000 up to $284,000 | Not applicable | $340.20 |
| above $142,000 up to $170,000 | above $284,000 up to $340,000 | Not applicable | $442.30 |
| above $170,000 and less than $500,000 | above $340,000 and less than $750,000 | above $91,000 and less than $409,000 | $544.30 |
| $500,000 or above | $750,000 and above | $409,000 and above | $578.30 |
What Is IRMAA Part D?
The IRMAA Part D prescription drug element of Medicare has a separate charge for the higher income brackets from the Medicare Part B health insurance. The IRMAA for Part D affects 8 percent of people on Medicare prescription drug plans. Medicare IRMAA Part D is on top of the cost of the prescription drug plan itself. Each Part D plan has its own monthly premium the insurance companies collect.
The IRMAA Medicare Part D can be deducted from your Social Security or bank account. Below are the new rates for Medicare Part D IRMAA 2022.
| File individual tax return | File joint tax return | You pay each month (in 2022) |
| $91,000 or less | $182,000 or less | $0.00 |
| above $91,000 up to $114,000 | above $182,000 up to $228,000 | $12.40 |
| above $114,000 up to $142,000 | above $228,000 up to $284,000 | $32.10 |
| above $142,000 up to $170,000 | above $284,000 up to $340,000 | $51.70 |
| above $170,000 and less than $500,000 | above $340,000 and less than $750,000 |
$71.30 |
| $500,000 or above | $750,000 and above |
$77.90 |
How Does IRMAA Work?
The Social Security Administration (SSA) will notify you within which IRMAA 2022 brackets you fall. The notification is an initial determination. In the notice, your rights will be spelled out and an appeal form included.
I suggest you verify that your tax information is correct and your income falls within the IRMAA limits Social Security specifies. Double-check you are looking at the IRMAA 2022 brackets. The official numbers come out each year by the first of the year and are found on the Medicare.gov website.
 The IRS provides SSA with your tax information. In the initial determination and before the tax is applied, check the accuracy of the IRS’s information. Make sure SSA has your correct income, filing status, and year. If your income decreased significantly because of a life-changing event (LCE) consider a Medicare IRMAA appeal to SSA.
The IRS provides SSA with your tax information. In the initial determination and before the tax is applied, check the accuracy of the IRS’s information. Make sure SSA has your correct income, filing status, and year. If your income decreased significantly because of a life-changing event (LCE) consider a Medicare IRMAA appeal to SSA.
SSA’s determination can change from year to year based upon the rise or fall of your income. Income is not only earned income but also qualified money from retirement accounts, sales of property and stock, and other investment income. Consult with your tax advisor for the relevant and current information for your situation. The IRMAA tax is based upon your income going back two years. The IRMAA limits can change each tax year.
I warn clients about the IRMAA tax, but inevitably I get the hesitant phone call. ‘What is this bill from Social security about?’ I remind them of the past conversations, and for those prospective high-income earning clients, the discussion around IRMAA might determine whether they stay on their employer health plan or go on Medicare.
Sometimes, it makes financial sense–if you plan on working anyway–to stay on the employer health plan, and not enroll in Medicare Part B. The cost of Medicare and the IRMAA tax may be substantially more than what you pay in premiums for your health plan at work. As much as I prefer to acquire clients than not, I have recommended several individuals over the years to stay on their employer health plan.
I spoke  with a surgeon the other day. He is now 70. We have talked each year for the past five. He works as a research consultant at a much-reduced salary. He is effectively part-time. His employer provides health coverage for him and his wife that is as good as Medicare for a much lower price than what he would pay because of IRMAA. He and his wife only have Medicare Part A. As his income decreases, they may eventually transition to full Medicare, but with the IRMAA brackets where they are, staying off Part B and not paying IRMAA tax is better.
with a surgeon the other day. He is now 70. We have talked each year for the past five. He works as a research consultant at a much-reduced salary. He is effectively part-time. His employer provides health coverage for him and his wife that is as good as Medicare for a much lower price than what he would pay because of IRMAA. He and his wife only have Medicare Part A. As his income decreases, they may eventually transition to full Medicare, but with the IRMAA brackets where they are, staying off Part B and not paying IRMAA tax is better.
IRMAA Appeal
Here are the IRMAA chart 2022 exceptions broadly considered. There are more reasons for an IRMAA appeal than can be easily listed. This list is not exhaustive.
|
Situation |
Description |
|
Tax return inaccurate or out of date |
|
|
A Life-Changing Event (LCE) that affects the beneficiary’s modified adjusted gross income |
There are 7 qualifying life-changing events:
|
The most common exception that has occurred among my clients over the years is a large IRA withdrawal. When people go to retire, some make a one-time large withdrawal from their IRA. The purposes vary. The most common one is to pay off a home mortgage upon retirement.
Of course, you pay the deferred taxes on the qualified money withdrawn from the IRA, but in terms of Medicare, the money is considered income even though it is retirement assets. You did not take the IRA contributions as income when you deferred them into your retirement account, so the government wants the taxes when you realize it as income. But, it is then counted as income for purposes of Medicare IRMAA.
More importantly, the result of an IRA withdrawal is to raise your income that year a considerable amount over your normal income. The IRMAA tax may apply, even though it is not your normal income. I have found those who go through the appeal process frequently receive a favorable decision in this kind of instance. I can help you with the form. The IRMAA appeal form is on the Social Security website.
 The Mechanics of IRMAA
The Mechanics of IRMAA
CMS (Center for Medicare & Medicaid Services) calculates IRMAA and publishes it yearly in the Federal Register. Once the IRMAA is calculated, CMS informs Social Security. Social Security has access to your income and tax information through the Internal Revenue Service (IRS). They communicate IRMAA determination. Social Security, which administers Medicare, notifies you of whether you need to pay more than the standard premium. The standard premium for Part B in 2021 was $148.50. Part B 2022 premium increased to $170.10 at the first of the year. Part D premium varies upon the prescription drug coverage.
IRMAA Medicare is based upon your modified adjusted gross income (MAGI) that the Internal Revenue Service (IRS) will report. Social Security considers years prior. They go back two years to determine the IRMAA surcharge. The IRMAA will adjust each year based upon that year’s MAGI. The surcharge is applied to the Part B premium and the Part D premium.
How to Appeal Social Security IRMAA?

The Office of Medicare Hearing and Appeals handles all appeals for IRMAA tax. There are two categories of Medicare IRMAA appeals.
- The calculation is incorrect.
- A life-changing event.
The specific life-changing events are marriage, divorce, death of a spouse, reduction in work hours and/or termination, loss of income-producing property, or loss of pension. You submit the Medicare IRMAA appeal form to the Office Medicare Hearing and Appeals where Social Security determines if the tax will be reduced.
As I am writing this article, I can no longer find the appeal form on the Medicare.gov or CMS.gov websites where is generally where you could find this form without much difficulty. After an hour’s search, I gave up. Hopefully, they will put the form back upon the website soon.
If you fall in the IRMAA tax category, it is something to seriously consider as you go on to Medicare. The tax may be temporary as your income declines in retirement, but for those whose income remains in the higher tiers, you may wish to consider other alternatives.
 As always, if you need help navigating the archine world of Medicare and Medicare insurance, please give us a call at 402-614-3389.
As always, if you need help navigating the archine world of Medicare and Medicare insurance, please give us a call at 402-614-3389.
 Every year there are changes to Medicare. The changes are usually not as drastic as the television commercials would lead you to believe. The purpose of the advertisements is to stimulate fear, uncertainty, and greed. They hit it hard to motivate you to call the 800-number. They will claim to offer a free objective evaluation. I find their objective evaluation inevitably ends with you changing to their plan. Know about Medicare 2021 changes before they flip you.
Every year there are changes to Medicare. The changes are usually not as drastic as the television commercials would lead you to believe. The purpose of the advertisements is to stimulate fear, uncertainty, and greed. They hit it hard to motivate you to call the 800-number. They will claim to offer a free objective evaluation. I find their objective evaluation inevitably ends with you changing to their plan. Know about Medicare 2021 changes before they flip you.
Unique One-Time Medicare 2021 Changes
My grandmother used to say, ‘live long enough, and you will see everything.’ The changes this year are unique because of the pandemic. COVID tests will have no co-pays. The vaccine is free. The federal government wants to overcome the virus, so Medicare is reflecting that public health policy.
Many Medicare plans had already offering telehealth options. With the pandemic, insurance companies now hardwire their plans with these options–most with zero co-pays.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) changes began in 2015. CMS implemented the changes slowly over the years so Medicare, the insurance companies, and beneficiaries could more easily adjust. Starting in 2020, those turning 65 did not have the opportunity to purchase the Medigap F or C plan. Medicare fazed out those plans with plan G being the principal plan with the most comprehensive coverage. They grandfathered in those 65 and over before 2020. They can still own and purchase plan Fs and C’s.
Medicare Part B Premium in 2021
The most significant Medicare change to know about in 2021 for most people is the Part B premium. This year it will increase from $145.60 to $148.50 per month per person, which is a $2.90 increase. Each year the premium amount is a hard-fought debate in Congress. Usually, Congress threatens to raise it much more. Constituents call in, and advocacy groups lobby, so the price usually goes down.
Part B Deductible in 2021
Medicare Part B consists of many different services. It has its own deductible, which is separate and distinct from the Part A deductible. The deductible increased from $198 in 2020 to $203 in 2021, only $5. The deductible is a flat amount. The consumer pays the deductible before the 20% coinsurance starts. For plan G, the Part B deductible is the only payment, aside from the monthly premium. The Medigap policy fills the remaining gaps in Part A and Part B coverage.
COLA 2021
Social Security and Supplemental Security Income (SSI) benefits for approximately 70 million Americans will increase 1.3 percent in 2021. The 1.3 percent cost-of-living adjustment (COLA) will begin with benefits payable to more than 64 million Social Security beneficiaries in January 2021. The Social Security COLA increase should not be less than the Medicare Part B premium increase. There are exceptions around this. If you are receiving Social Security benefits, you will be held harmless on the increase, but those who do not take Social Security benefits will pay the increase.
Medicare 2021 Changes for Part A
Medicare Part A covers inpatient hospitals, skilled nursing facilities, and some home health care services. About 99 percent of Medicare beneficiaries do not pay a Part A premium since they have at least 40 quarters of Medicare-covered employment. The Medicare Part A inpatient deductible that beneficiaries will pay when admitted to the hospital is $1,484 in 2021, increasing $76 from $1,408 in 2020.
Part D Changes in 2021 (Senior Savings Model)
The Senior Savings Model is an experiment in modeling that tests the impact of offering beneficiaries an increased choice of enhanced alternative Part D plan options that offer lower out-of-pocket costs for insulin. One in every three Medicare beneficiaries has diabetes, and over 3.3 million Medicare beneficiaries use one or more of the common forms of insulin. For some of these beneficiaries, access to insulin can be a critical component of their medical management, with gaps in access increasing the risk of serious complications, ranging from vision loss to kidney failure to foot ulcers (potentially requiring amputation) to heart attacks.
Unfortunately, sometimes the cost of insulin can be a barrier to appropriate medical management of diabetes. CMS’s designed Senior Savings Model for Part D plans to address President Trump’s promise to lower prescription drug costs. The model provides Medicare patients with new choices of Part D plans that offer insulin at an affordable and predictable cost. A one-month supply of a broad set of plan-formulary insulins costs will be no more than $35 each.
Medicare changes to know in 2021 are your drugs listed in the formulary. Part D premiums for 2021 will probably rise an average of 9%. The average stand-alone Part D premium is $41 in 2021. The premiums range from $7 a month for the SilverScript SmartRx plan to a high of $89 for the AARP MedicareRx Preferred plan.

Part D Deductible 2021
The Part D drug deductible went up from $435 to $445 on most plans. That is the max deductible CMS allows insurance companies to set the deductible. They can set it lower, though few plans did this year, and for those plans with zero deductible or a lower deductible, the cost is offset by either higher monthly premiums or co-pays or both.
Most of the time, that deductible is only applicable to tiers 3, 4 & 5 medications.
The first of the year is the time when I get the distressed phone calls because people must meet their deductibles. Many forget the deductible starts over again in January, and they are shocked when they show up at the pharmacy counter. I have to remind clients they need to meet the deductible first to get to the lower copay.
Medicare Advantage Changes in 2021
In the nine years, I have offered Medicare Advantage plans, I have seen the number and especially the quality of the plans increase significantly. Nationally more Medicare Advantage plans are offered now than ever before. In Nebraska and Iowa, I have seen the number of counties offering quality plans explode.
There are now over 4,800 Medicare Advantage plans, an increase of 76% over 2017. The average person will choose from 33 plans offered by eight different insurance companies, with some areas having as many as 60 different plans.
Besides, the number of Special Needs Plans (SNP) also increased to nearly 1,000 in 2021, a sizable jump. The increase in SNP means more people have access to low-cost plans with extra benefits to manage chronic conditions and diseases.
Medicare Advantage Premiums in 2021
Average Medicare Advantage premiums dropped for the fourth consecutive year to $21 in 2021, down from $25 in 2020. Nearly 90% of all Medicare Advantage plans include Part D prescription drug coverage.
Of note, the Medicare Advantage out-of-pocket maximum will increase to $7,550 in 2021, up significantly from $6,700 in 2020. However, the vast majority of insurance companies set their out-of-pocket max well below the government limit. In 2020, the average Medicare Advantage out-of-pocket maximum was $4,900.
 Medicare Advantage and ESRD
Medicare Advantage and ESRD
The most heartening plan change for Medicare Advantage is ESRD (End-Stage Renal Disease). When I first started, the only pre-existing condition that excluded me from enrolling someone in a Medicare Advantage plan was ESRD. While I didn’t have that situation very often, it was sad when I couldn’t offer Part C to clients.
ESRD is one of the health issues that almost always automatically makes you Medicare eligible. Still, if you are younger than 65 in Nebraska and Iowa, you are not eligible for a Medicare supplement. The dialysis falls under the unlimited 20% coinsurance of Part B. The cost can be incredible. Even for those on Medicare Advantage, beneficiaries can easily hit the maximum out of pocket.
At least now those with ESRD can get on a Medicare Advantage plan and limit their out-of-pocket costs.
There’s good news for people with ESRD in 2021. In the past, those with ESRD could not join Medicare Advantage unless there was an ESRD Special Needs Plan available. However, new rules grant guaranteed issue rights to people with ESRD for any Medicare Advantage plan offered in their service area.
Access to Medicare Advantage when you have ESRD is massive. Long-standing rules allowed Medigap companies to deny coverage to people with ESRD outside their Medigap Open Enrollment Period. Even many states that enacted laws forcing insurers to offer Medigap to people under age 65 failed to extend that protection to people with ESRD.
What this means is that, for the first time, people with ESRD have low-cost options to control their health care expenses with a Medicare Advantage plan. If that applies to you, you could have used the 2020 Annual Election Period to shop for a new Medicare Advantage plan.
Provider Compensation
Congress made significant changes to the billing process behind Medicare in the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA changes how Medicare rewards providers for qualify over volume inpatient care. It streamlines provider reimbursements through the Merit-Based Incentive Payments System (MIPS) and even grants bonuses for participation in alternative payment models (APMs). Still, the change that gets the most attention is the eliminating of Plan F and C in the Medigap lineup. The plans completely covered the Part A deductibles and Part B co-insurance, so beneficiaries did not have to pay anything aside from their monthly premiums. Congress found the lack of co-pays and deductibles was an incentive for waste and abuse of the Medicare system. Starting in 2021, you could no longer purchase Plan F or C when you turned 65. Those who turned 65 before that period were grandfathered into Plan F and C.
through the Merit-Based Incentive Payments System (MIPS) and even grants bonuses for participation in alternative payment models (APMs). Still, the change that gets the most attention is the eliminating of Plan F and C in the Medigap lineup. The plans completely covered the Part A deductibles and Part B co-insurance, so beneficiaries did not have to pay anything aside from their monthly premiums. Congress found the lack of co-pays and deductibles was an incentive for waste and abuse of the Medicare system. Starting in 2021, you could no longer purchase Plan F or C when you turned 65. Those who turned 65 before that period were grandfathered into Plan F and C.
The other most obvious change was the Medicare number is no longer your Social Security number, but a unique eleven-digit number combining letters and numbers. Everyone’s card should have been replaced by the end of 2019, though I still have some clients who have their old numbers and card. It is a simple matter of calling Medicare for a replacement card.
Medicare makes slight changes over time. Many times the Medicare changes to know about in 2021 do not apply to you, but you, or your agent, still need to be aware of what is going on to always maximize your benefits and avoid disadvantaging yourself temporarily or permanently.
What is Medicare? A basic question. Or rather, why should anyone care about Medicare? The reason people should care is that most bankruptcies are medical bankruptcies. In other words, if you wish to protect your retirement nest egg from bill collectors, Medicare is important to know about. There are few things that are more disturbing than a pile of medical bills sitting on the kitchen table. The golden years could be tarnished with worrying about actual or potential medical expenses. Medicare–if implemented proper–will protect you from a potential catastrophe. It is critical for people entering into retirement to understand what is Medicare.
What is Medicare?
 Medicare is a Federal health insurance program for people who are 65 and older (or on Social Security disability). It began in 1965 when President Johnson signed it into law. It was designed to provide medical covered to the elderly at a reasonable price. In 1965, few people had health coverage once they stopped working. As a result, many seniors fell into poverty because of burdensome medical expenses. Medicare was a solution to a national problem.
Medicare is a Federal health insurance program for people who are 65 and older (or on Social Security disability). It began in 1965 when President Johnson signed it into law. It was designed to provide medical covered to the elderly at a reasonable price. In 1965, few people had health coverage once they stopped working. As a result, many seniors fell into poverty because of burdensome medical expenses. Medicare was a solution to a national problem.
Medicare Part A
Medicare is divided into two parts: Medicare Part A and Medicare Part B. Medicare Part A has everything to do with the hospital. It doesn’t cost anything because you paid for it during your working years. It was one of the deductions in your payroll taxes. Medicare Part A covers a 100% of the medical expenses incurred in the hospital, but there is deductible that many people are not aware of. The Medicare Part A deductible is currently $1,288. This is NOT an annual deductible. It is a deductible per benefit period, and a benefit period is 60 days. So each event has a deductible, and the time for the event is 60 days. In other words, you could have multiple events and pay multiple deductibles because the event is not limited to just a 60 day period. Each new event, even if it overlaps with another event, has its own 60 day timeline. While rare, it could happen, and probably more importantly, you could pay the Part A $1,288 deductible more than once in any given year.
Medicare Part B
Medicare Part B, however, does cost something. For most people going on Medicare and Social Security in 2016, the Medicare Part B premium is $121.80 per month. It is generally taken out of your Social Security check. Medicare Part B covers doctors’ visits and outpatient procedures, such as X-rays, blood work, emergency room visits, etc. Medicare Part B covers 80% of the cost. Your portion is 20%. The 20% coinsurance, however, is unusual. There is no cap. There is no maximum out-of-pocket. Most group plans you were ever on probably had a maximum out-of-pocket. It may have been $1,000, $2,000, even $10,000, but at some point, you stopped paying and the insurance company covered everything. Medicare Part B does not have that, so 20% of a big number will be a big number. You keep paying your 20% coinsurance as long as the bills come in.
These are the basic building blocks to what is Medicare. You must understand Medicare, Medicare Part A, and Medicare Part B to understand the rest that follows. In the next blogs and videos, we will cover how to get Medicare, how to cover the Part A deductible, and how to fill the unlimited 20% gap in Part B coverage.
Delay Medicare Enrollment
Many people work past 65. They continue on with them employer group coverage. They delay Medicare enrollment. At 66+, they wonder what to do about Medicare.
How to Enroll after 65
Here is what to do. Go to Medicare.gov. Click on “Forms, Help, Resources” on the top right. Then click on “Medicare Forms” on the left middle. You will see the enrollment forms in the middle of the page in PDF form. There are two forms: one to enroll in Medicare Part B and a second for your employer to sign off on your coverage. You fill out the enrollment in Part B. Give the second form to your employer. Your employer will verify that you have had health coverage as good as Medicare since you turned 65. They will sign the form. It is important for you to write in the date that you wish your Medicare Part B to start. Give yourself enough time to find a Medicare plan and prescription drug plan. (There are much shorter and restrictive time limits when you have delayed Medicare Part B enrollment.) Drop the forms in the mail or hand deliver them to the local Social Security office.
Medicare Employer Enrollment Forms
Why do you want to involve your employer with your enrollment in Medicare Part B? If you do not have your employer verify that you had health coverage from the time you could have enrolled in Medicare until the time you did take Part B, Medicare will assume you did not have creditable coverage and will asset a penalty. The penalty is a 10% increase in Part B premium for every year you did not have coverage. That can be significant over time and completely unnecessary. Delay Medicare enrollment at your own risk. Get the form. Your employer is required to verify. The human resource department will know exactly what to do. It is a very simple matter.
At Omaha Insurance Solutions, we help clients who delay Medicare enrollment all the time. We can get this done quickly and easily. Give us a call 402-614-3389. We can email you the forms, walk you through filling them out, and explain what to do.