Original MedicareCategory:
Why do so many people bash Medicare Advantage? Yet, in every Part of the country, Medicare plans are expanding, and more people are joining. Why are Medicare Advantage plans considered so bad when they attract so many people and keep them as loyal customers?
 What Makes Medicare Advantage Plans Bad?
What Makes Medicare Advantage Plans Bad?
The main reason is location, location, location. Medicare Advantage plans are designed for a particular location, usually a county or collection of counties that make up a region. Medicare Advantage is unlike Original Medicare (only Part A and Part B). Original Medicare is uniform and homogenous throughout the country. Medicare Advantage is not. One plan with the same insurance company may drastically differ from one city to another. In the same state, a plan may be great in an urban area but incredibly poor in a rural area 40 miles away.
When people criticize Medicare Advantage, they create a straw man. They pick the worst locations and the weakest plans. Then they compare those Advantage plans to Original Medicare with the additional insurance product of a supplement. The plans they use as models have high out-of-pocket costs, high copays, limited networks, and low star ratings. Consequently, Medicare Advantage makes a poor showing in those instances.
What Are the Common Pitfalls of Medicare Advantage?
High Out-of-Pocket Costs
Critics claim that Medicare Advantage plans have high out-of-pocket costs. Medicare Advantage’s maximum out-of-pocket (MOOP) for 2023 is $8,300 nationally. That is the highest out-of-pocket an insurance company may charge on a Medicare Advantage plan.
highest out-of-pocket an insurance company may charge on a Medicare Advantage plan.
Insurance companies can set the maximum out-of-pocket (MOOP) lower than the allowed amount. On average, the MOOP was $4,972 in 2022 for in-network and $9,245 out-of-network nationwide.
The MOOP is the highest amount you are responsible for on the plan. Copays add up. If you meet the MOOP total of $8,330–or whatever the amount is–the plan pays 100% on any claims after that.
No Maximum Out-of-Pocket for Original Medicare
Compared to Original Medicare, however, Medicare Advantage has a top limit–a maximum out-of-pocket. Original Medicare has no maximum or cap on the Part A deductible. The Part B coinsurance is an unlimited 20%. Twenty percent of a million dollars is real money!
Those costs that Original Medicare does not pay are only covered if you purchase additional health insurance with a Medigap plan. You need to pay an additional amount to add a Medicare Supplement. A Medicare Supplement in the Omaha, Lincoln, and Council Bluffs areas for a 65-year-old ranges from $1,400–$2,000 per year for a Plan G on top of your Medicare Part B premium, which is currently $164.90.
I work primarily in the Omaha, Lincoln, and Council Bluffs Metro areas. Our maximum out-of-pockets are lower than the national average. Some Medicare Advantage plan MOOPs are as low as $3,800.
Nonetheless, $3,800 or $8,300 is a great deal of money for most people to come up with in a year’s time. It is a legitimate concern, so a person may wish to consider a Medigap Plan N or even High-Deductible Plan G as an alternative to Medicare Advantage. However, many people feel a $4,000 or $5,000 maximum annual out-of-pocket is reasonable for a health insurance plan. It is the same or lower than many employer health plans people had in the course of their working years.
‘Is There A Doctor In the House?’
 Like your employer health plans, Medicare Advantage plans are usually network plans. The most common types of plans are HMO (Health Maintenance Organization) and PPO (Preferred Provider Organization). The HMO plans generally mean you can only see health providers in the plan’s networks. If you go outside of the network–aside from emergencies–the plan will not pay. PPO plans allow you to go outside the networks to providers who take Medicare, but you may pay more for those services, and your MOOP will be higher.
Like your employer health plans, Medicare Advantage plans are usually network plans. The most common types of plans are HMO (Health Maintenance Organization) and PPO (Preferred Provider Organization). The HMO plans generally mean you can only see health providers in the plan’s networks. If you go outside of the network–aside from emergencies–the plan will not pay. PPO plans allow you to go outside the networks to providers who take Medicare, but you may pay more for those services, and your MOOP will be higher.
Network plans can be limited in certain areas. Many rural areas have weak Medicare advantage plans. One of the reasons is that many providers or medical facilities do not work with the plans yet. In those instances, Original Medicare would probably be a better choice with or without a Medicare Supplement.
In other places, I’ve found that the different medical networks compete aggressively against one another. Part of their strategies is to align with specific insurance companies providing Medicare Advantage against their competitors. In this way, a plan might have a limited network of doctors and hospitals. In those situations, an agent must be acutely aware of his client’s needs and weigh all the factors. Depending upon the limitations, Original Medicare may be the better alternative.
Medicare in our Omaha, Lincoln, and Council Bluffs areas are blessed with three robust networks that cooperate with the six insurance companies offering plans in the area. The three networks work with all the plans. Networks and access to providers are non-issues here.
Referral, Or Not Referral
Some Medicare Advantage plans require a referral from your primary care physician (PCP) to see a specialist. The purpose of the referral system is to coordinate care and reduce costs.
costs.
In our area, the HMO plans are “open access.” Open access means no referral is required to go to a specialist when you need one. As a matter of fact, it has been years since Medicare Advantage plans required referrals in our area. However, some plans in some areas still require referrals, which some feel is a drawback.
Medicare Advantage Plans Change Benefits Every Year
Critics of Medicare Advantage site plan changes as a negative for Medicare Advantage. However, Original Medicare also changes. Medigap companies increase premiums almost every year, even several times a year, because of age, higher than normal claims, and inflation. Medicare Part D prescription drug plans DEFINITELY change yearly–premiums, deductibles, copays, and formularies are reworked every year.
 Each year the Medicare Advantage plans mail out the ANOC (Annual Notice Of Changes). An example of changes is: the maximum out-of-pocket may increase. Copays may increase or decrease. Extra benefits, like dental and vision, may be increased or reduced, added or eliminated. You will experience change no matter which direction you go with Medicare.
Each year the Medicare Advantage plans mail out the ANOC (Annual Notice Of Changes). An example of changes is: the maximum out-of-pocket may increase. Copays may increase or decrease. Extra benefits, like dental and vision, may be increased or reduced, added or eliminated. You will experience change no matter which direction you go with Medicare.
Over the decade I have offered Medicare Supplements, Medicare Advantage Plans, and Medicare Part D prescription drug plans, all of them changed. Nobody is not changing–sorry for the bad grammar. Some years there are a lot of adjustments. Most of the time, the changes are minor. The changes really hinge on the funding the federal government pumps into Medicare or not and the rate of inflation.
In our area, the Medicare Advantage plans have actually gotten significantly stronger over time. MOOPs have lowered. Additional benefits, like dental, vision, and over-the-counter (OTC) items, were introduced and increased.
Medicare Part A & Part B usually change each year. The Part B premium increases, though it went down slightly this year. Deductibles increase. Part A deductible increased from $1,556 to $1,600 for 2023. Most people don’t notice Original Medicare changes because, if they have a Medigap policy, their supplement takes up the slack. They may not be aware until they get notice of a rate increase from the insurance company. Then, they blame the insurance company for the higher premium, not Medicare. A big part of the higher premium is because Medicare expanded the gap the insurance company needed to fill.
Part D Drug Changes
The biggest problem I have found with the Medicare benefits changing every year is with Part D prescription drug plans. Those on Original Medicare and a Medigap plan have Part D plans. The challenge is insurance companies change the drugs that are covered or not covered. The copays, deductibles, and premiums can change significantly in some years. Companies move drugs from one tier to another. The Gap (or “Donut Hole”) amount fluctuates from year to year. I find Part D plans change significantly compared with the drug element of Medicare Advantage plans.
Clients who ignore the changes in their Part D plan find themselves in a world of hurt come Jan. 1st when they go to the pharmacy counter to pay for their prescriptions.
Whether you are on the Medicare Advantage side or Medigap and Part D side, there is plenty of change to go around.
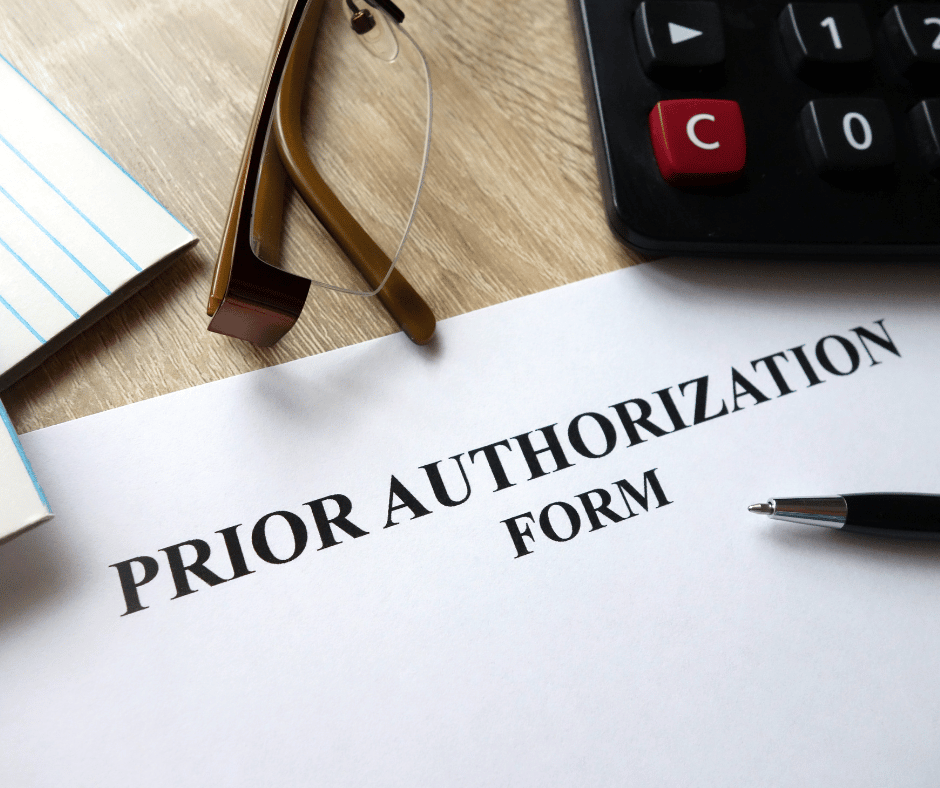
Medicare Advantage Plans Requires Prior Authorization
 Critics of Medicare Advantage point out that Original Medicare does not require prior authorization for most services. Medicare Advantage, however, does require prior authorization for many.
Critics of Medicare Advantage point out that Original Medicare does not require prior authorization for most services. Medicare Advantage, however, does require prior authorization for many.
The criticism is the delay that pre-approval causes. Detractors claim denials are higher for Medicare Advantage than Original Medicare, and the appeal process for denials is arduous.
Preauthorization can be a challenge. You may have faced it with your employer’s health plans. Getting approval from the insurance company is not a new idea. In the past with Medicare Advantage, denials may have been higher. Currently, denials are around 4 percent the first time around. Upon appeal, 75 percent of appeals are overturned. I hear more complaints from clients on Original Medicare and a Supplement. Last week, Medicare refused to pay for my client’s ambulance ride to the emergency room at 3 AM. I helped her with the appeal process.
For urgent cases, you can receive treatment and get approval afterward, or they will rush approval with a response in 72 hours or less.
Changing Your Medicare Advantage Plan
Medicare Advantage critics claim you can’t get out of your Medicare Advantage plan except during a short window of time each year.
Generally, you can only change your Medicare Advantage plan during the Annual Election Period (AEP), which is Oct. 15th- Dec. 7th each year. Ironically, for those on Original Medicare, that is the only time you can change your Medicare Part D prescription drug plan as well. Medicare limits everyone on Medicare in one way or another.
Medicare Advantage also has more times to change than those on Original Medicare. Medicare Advantage has its own unique Open Enrollment Period (OEP) from Jan. 1st–Mar. 31st, when you can make a one-time switch to another Medicare Advantage plan or change back to Original Medicare.
The advantage of Medicare Supplements critics assert is that you can change your supplement year-round. Changing a supplement, however, is subject to underwriting in most states. There is no underwriting for Medicare Advantage. Insurance companies offering Medicare Advantage plans must take you regardless of your health.
Medicare Advantage Does Not Travel
For many years Medicare Advantage plans were criticized because they were only local, especially HMO plans. The health coverage did not travel with you when you left home, except for emergencies.
for emergencies.
Now you are covered for not only emergencies anywhere in the U.S. and, in some cases, abroad, but there may also be in-network coverage. Many of the larger insurance companies also have national networks to which the HMO plans have access, so you could be outside your service area and still get service and pay in-network copays.
You can also select a PPO (Preferred Provider Organization) plan. In a PPO, you can go out of network to a provider who takes Medicare. You may pay a higher copay, and your total out-of-pocket may be larger than in-network, but you will have access to non-network doctors and hospitals with a PPO plan.
Medicare Advantage plans are bad when the networks are small, the MOOP and copays are high, and customer service makes prior authorization a headache. Many rural areas have Medicare Advantage plans that are bad. Some insurance companies design Medicare Advantage plans that are poorly constructed, even bad. Like markets for many products or services, the areas and the companies may not produce the best product or service.
Caveat Emptor – Let the Buyer Beware!
The consumer needs to do his due diligence and use a reputable agent who will give you an honest assessment of the products in your market. Does the plan have good access to medical providers? Are the copays and maximum out-of-pocket reasonable for your budget? Is the company behind the plan strong and well-staffed to provide good to excellent service?
Conclusion
In the decade I have offered Medicare plans and supplements, I have seen the landscape change regarding insurance companies and products. For Medicare in the Omaha, Lincoln, and Council Bluffs areas, Medicare Advantage plans have continually improved with broader access to networks, low copays and MOOPs, and tremendous service to resolve issues as they arise. Some other places are not as good for Medicare Advantage. Many counties in rural Nebraska and Iowa still have no Medicare Advantage plans, or the plans are very weak. Each plan needs to be judged on its own merits, particularly when you are comparing it to Original Medicare and a Medigap policy, and a Part D prescription drug plan.
The question has changed from “Why are Medicare Advantage plans so bad?” to “How are Medicare Advantage plans so good?”
When people compare Medicare with Medicare Advantage, they usually mean Medicare (Original Medicare) with a Medicare Supplement and a Medicare Part D prescription drug plan versus Medicare Advantage (Part C) with prescription drugs included.
The comparison is difficult because they are drastically different, so I believe a fair side-by-side comparison is impossible. That, however, does not stop people from asking the question of which is better, Medicare Advantage or Medicare Supplement.

Medicare Is Original Medicare: Part A & B
Original Medicare is Part A for hospitals, and Part B for doctor visits and outpatient procedures. Part A has a $1,600 per event deductible in 60 days without a cap. Part B is an 80/20 split. You pay the 20% coinsurance, and there is no limit on the 20%.
Original Medicare + Medicare Supplement
To fill in the gaps in Medicare, you may purchase a Medicare Supplement / Medigap policy. Depending on where you live and the company you choose, the monthly premium can range from $100 to $200 per month. You can fill in the gap entirely except for the first $226 with a Plan G. As you age past 65, the price of your Medicare Supplement will increase.
Sometimes, your supplement may increase by hundreds of dollars. I recently had someone referred to me who was paying over $300 for her Medigap Plan G policy. She was in her mid-70s. She passed through underwriting, so we switched her to another Medigap plan at half the cost. Some people, however, cannot pass underwriting and need to remain on their high and increased Medigap policy.
Medicare Supplement + Medicare Part D PDP
Part D prescriptions drug plan (PDP) is separate from your Medicare Supplement and a separate charge. Again, the premium can range from $10 to $100 per month, with different prices for your medication copays. The key to comparing Part D plans is the year’s total cost — monthly premium plus individual prescription copays.
Medicare Advantage Or Medicare Part C

Medicare Advantage (or Part C) is different. Private insurance companies take what Original Medicare does and has a maximum out-of-pocket cost cap. Original Medicare, remember, is unlimited.
Medicare Advantage breaks out each of the different services. For example, x-rays, outpatient surgeries, labs, emergency services, etc. The service is given small copays versus Original Medicare’s unlimited 20%. These minimal copays add up toward the maximum out-of-pocket (MOOP). Most years, you will not reach your maximum out-of-pocket. In most years, your out-of-pocket will be $500 or less.
Medicare Advantage Has a Maximum Out of Pocket
The maximum out-of-pocket (MOOP) nationally is currently $8,300. The Omaha, Lincoln, and Council Bluffs area average around $4,500 or less for the MOOP. Some of the plans’ MOOP is $3,900. Original Medicare does not cover your coinsurance or deductibles unless you make the additional purchase of a Medigap policy.
Most Medicare Advantage plans also include Part D prescription drug coverage. There is no separate charge. Most of the Medicare Advantage plans in our area are zero premium or are very low premium with prescriptions included. The prescription drug part of Medicare Advantage excludes the Part D deductible on most plans. The current Part D deductible on stand-alone prescription drug plans is $505.
The cost for Medicare Advantage with drug coverage is usually zero. Your only monthly cost is your Medicare Part B premium and possibly copays for the medications.
Over the years, Medicare Advantage copays have increased to reflect rising medical costs and inflation. The increase has been minimal, but that will change, I’m sure, in our current high-inflation atmosphere. The same will be valid for Original Medicare and Medicare Supplements.
Medicare Advantage Has Networks
Another difference that concerns people choosing between Medicare Supplement and Medicare Advantage is medical networks. This is a genuine concern in certain areas. In our Omaha, Lincoln, Council Bluffs metro area, there are principally three networks: CHI Health, Nebraska Medicine, & Methodists Health Systems. The Medicare Advantage plans in our area work with all three networks. It is a non-issue. In other places, the network system may be something to be aware of.
All the Medicare Advantage companies offer PPO (Preferred Provider Organization) options. You can go out of network to someone who accepts Medicare. You may pay more and have a larger MOOP, but there is that option. You are not confined exclusively to the plan network.
Also, many of the larger insurance companies offer national networks, so even within their HMO (Health Maintenance Organization) system, you may still be able to see doctors and hospitals outside your local service area and pay in-network copays.
Medicare Advantage Prior Authorization vs Original Medicare & Supplement
The other difference between Original Medicare / Medicare Supplement and Medicare Advantage is preapproval. Original Medicare does not require prior authorization for most procedures and services. Medicare Advantage is the reverse. This is an unusual concern because, during all your working years, your insurance companies required prior authorization for any services of any cost or significance.
With Medicare Advantage, there is really no change. Those who do not favor Medicare Advantage put this out as a deficiency in the program. In my experience and statistically speaking, most denials in the big picture are overturned. The national average for Medicare Advantage denials is 4 percent. Those denials are usually attributed to a lack of explanation and documentation on the provider’s part. The fix is usually an easy and quick remedy when the effort is put in to correct the error.
How Much Risk Do You Want to Carry?
Original Medicare with a Medigap policy and Part D prescription drug plan is the most comprehensive Medicare insurance. You have reduced risk to the lowest level. The trade-off is you pay an ever-increasing premium for the convenience of not paying copays or an expensive year when you require many medical services.
Medicare Advantage saves you a monthly premium upfront, but you will pay copays as services are required. You may even reach your maximum out-of-pocket during a challenging year. That is the trade-off.
Networks are something to consider with Medicare Advantage. That consideration should be based on a case-by-case basis, depending on your location. But with national networks and PPO plans, the network issue is not the issue it was a few years ago.
How much risk do you wish to assume, and how much do you want to budget toward healthcare? The answer to those questions is the solution to which is better Medicare Advantage vs. Medicare Supplements.

Medicare has had an exciting history with prior authorization. Medicare prior authorization has become controversial over the years because of Medicare Advantage.
Have You Always Been Subject to Prior Authorization?
Health plans started using prior authorization in the 1960s. Hospital admittance grew after the creation of Medicare and Medicaid. At the same time, more employers began offering employees health insurance as part of their compensation package. Medical costs grew significantly, particularly hospital stays.
Insurance companies began implementing utilization reviews in the 1960s. Utilization reviews were a process to reduce the overutilization of resources and identify waste. Registered nurses initially performed utilization reviews in hospital settings. The skillset gained popularity within the health insurance industry as research grew around medical necessity, misuse, and overutilization of services.

Health plans reviewed claims for medical necessity and hospital length of stay. Health plans began to require physicians to certify the admission and subsequent days after admission to help contain costs. Prior authorization originated from the use of utilization reviews.
Fast-forward to the present day. You were subject to prior authorization when you entered the workforce and received employer-provided group health insurance as a benefit. The insurance company determines if it is “medically necessary” and covered by the policy your company purchased when you have any medical procedure. Then there is further discussion about the appropriate charges. Whether or not you were aware of it, prior authorization has always been part of your health insurance coverage.
Why Do Insurance Companies Use Prior Authorization?
Prior authorization is a medical management tool. Doctors and insurance companies work together to ensure that a specific treatment or service is the best option for the patient’s needs.
The purpose of prior authorization is to identify and discourage unnecessary and costly low-value services to reduce wasteful spending without impeding quality healthcare services.
Prior authorization, supervision, audits, and other compliance tools help identify and root out fraud, waste, and abuse in the healthcare system. The ultimate purpose is to reduce costs for the consumer and prevent unnecessary treatments.
The Department of Justice announced today (Feb 17, 2021) criminal charges against 138 defendants, including 42 doctors, nurses, and other licensed medical professionals, in 31 federal districts across the United States for their alleged participation in various healthcare fraud schemes that resulted in approximately $1.4 billion in alleged losses.
The charges target approximately $1.1 billion in fraud committed using telemedicine, $29 million in COVID-19 healthcare fraud, $133 million connected to substance abuse treatment facilities or “sober homes,” and $160 million connected to other healthcare fraud and illegal opioid distribution schemes across the country.

While most doctors, medical professionals, and medical facilities are honest and act with integrity, an element will always and continually seek illicit gain costing consumers and taxpayers untold amounts. This results in higher insurance premiums and medical costs. It is naive to believe all are good actors and that every recommended treatment and service is the best fit.
Why Does Original Medicare Not Use Prior Authorization?
In part, the Medicare prior authorization controversy is that “Original Medicare” does not require prior authorization for most procedures, and Medicare Advantage does. (Original Medicare is just Medicare Part A and Part B. The payment structure is called fee-for-service. Medicare Advantage (or Part C) is Medicare administered by a private insurance company contracted and approved by Medicare.)
At first glance, you probably ask, ‘Why does Original Medicare not require prior authorization’ because prior authorization is common practice in the health insurance world? No company will leave the decision to spend potentially tens of thousands of dollars, even millions, to one person without some oversight.
When Medicare was established, Congress included certain arrangements and excluded others. In Section 1862(a)(1)(A) of the Social Security Act:
“No payment may be made under Part A or Part B for any expenses incurred for items or service which . . .. are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed member . . ..”
The key phrase is “reasonable and necessary.” “Reasonable and necessary” has been interpreted over the years very broadly. If a submitted claim is in an allowed category and not excluded, the submission is “reasonable and necessary.”
The doctor authorizes an MRI of the shoulder because the patient complains of problems. MRIs are covered. This procedure is “reasonable and necessary” because it is not an uncommon practice, even if there may be less expensive diagnostic procedures or treatments.
As you can probably guess, this broad interpretation with no oversight or accountability will result in large amounts of fraud, waste, and abuse.
Why Is Medicare Advantage Prior Authorization So Controversial?

The short answer to why is that Original Medicare doesn’t require prior authorization. The controversy is some believe beneficiaries are being denied essential medical services and treatments. Beneficiaries and medical professionals do not even attempt to overturn denials because they believe the appeal process is so burdensome.
The facts, however, do not paint such a sad picture. The Office of the Inspector General reviewed a large number of Medicare Advantage Organizations (MAO), reviewing 448 million preauthorization requests in 2016. Of those, MAOs denied about 1 million preauthorization requests for a denial rate of 4 percent—4 percent is tiny.
The September 2018 Office of Inspector General report found that Medicare Advantage Organizations (MAO) overturned 75 percent of their own denials from 2014-2016, overturning approximately 216,000 yearly. During that same period, independent reviews discovered additional requests that had been inappropriately denied.
The most surprising finding, however, is that only one percent of beneficiaries and providers appealed their denial, which raised the question: how many were denied necessary treatment because the process is so arduous?
Unfortunately, the study does not give a coherent explanation of the denials. From my experience of doing Medicare planning for a decade with thousands of beneficiaries, doctors’ offices do not always submit requests with detailed documentation in support. When the request is denied, they blame the insurance company, and the effort stops unless the patient pushes the issue.
The other reason I find for denial is the doctor’s office uses the wrong billing code. Quite often, the insurance company does not give any explanation in those cases. The response is “denied.” The solution requires the doctor’s office to call and talk with the claims department about billing codes, documentation, and supporting tests. In the absence of these items, nothing happens.
Unfair Statistics and Sensational Journalism
The Department of Health and Human Services Office of Inspect General (OIG) conducted a study of Medicare Advantage Organizations’ (MAO) denial of prior authorizations during one week (June 1-7, 2019). In that week, there were 250 denials. The OIG discovered that 13 percent of these prior authorizations were incorrect. This amounted to 33 cases.
Later in the same report, they admitted the usual national average is 5 percent. No reason was given why the study was not expanded when the conclusions from their study did not coincide with other long-standing evidence, particularly when the study was so microscopic–one week and 250 cases.

In the same study, they did not review the cases where the prior authorization was approved when it should have actually been denied. There was also no control group to compare against. The OIG did not study fee-for-service Medicare billing for fraudulent or wasteful claims or denials on their part.
The New York Times piled on in an April 2022 article. They presented a very slanted view of the study, beginning the article with “Medicare Advantage plans often deny needed care, federal report finds.” Only toward the very end of the article did the author get into any of the facts of the report. The general impression during the first half of the article is Medicare Advantage denies its clients the necessary medical care they need.
Why Are Medicare Prior Authorization Denials Overturned?
Denials may be overturned for many reasons. First, there were errors on the part of the insurance company. The decision was incorrect.

Errors on the part of the doctor’s office or medical facility. They did not include sufficient documentation or incorrect information. The denial is reversed, then. The provider may add new information from additional tests in the appeal process that contributes to an overturn.
The overturn does not necessarily mean the MAO acted inappropriately, but the process and extra steps critics claim create friction in the system. Patients may wish to avoid going through the trouble of appeal. Doctors may not make recommendations because of a history of denials.
Did Medicare Ever Use Prior Authorization?
The Medicare practice of accepting bills from providers at face value without question as “reasonable and necessary” was an established and haloed practice from the beginning of Medicare. All parties who benefited the most—except U.S. taxpayers—were unmotivated to change until the wheelchair scandal.
In 1999 it was discovered that Medicare spent $8.2 billion to procure power wheelchairs and “scooters” for 2.7 million people. A large portion was paid to scammers because they discovered that Medicare not only did not require prior authorization for wheelchairs, but Medicare did not even review the authenticity of the claims.
A Washington Post article published in August 2014 highlighted the massive fraud of Medicare’s resources. The article chronicled the sensational scams and trials of many Medicare swindlers. The outrageous theft of public funds and the massive fraud shamed CMS to amend its regulations to finally require preauthorization for some “durable medical equipment,” i.e., electric wheelchairs.
Bureaucrats inside CMS admitted they knew how the wheelchair scheme worked as early as 1998. But it was not until 15 years later that officials finally did enough to curb the practice significantly. Durable medical equipment—electric wheelchairs—is the only exception to the “reasonable and necessary” practice. They must be preapproved.
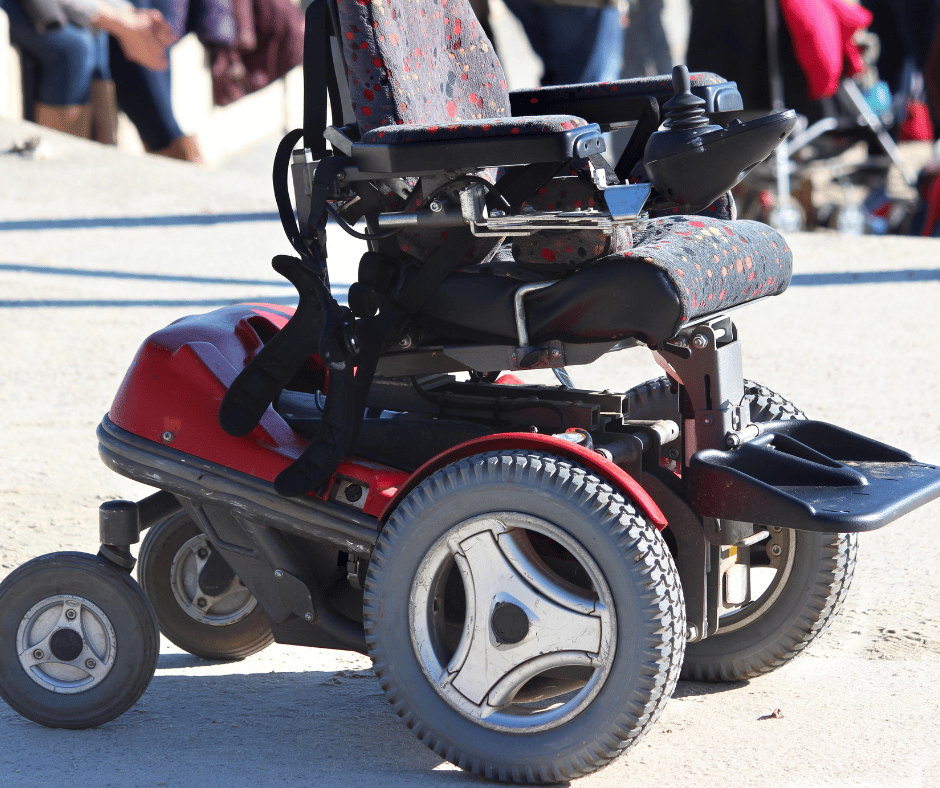
Consequently, hundreds of millions of false and unnecessary claims were paid over many years in a massive Medicare fraud. Once the bureaucratic problem was fixed, and claims were more thoroughly reviewed, an enormous shift occurred. Medicare reimbursements for motorized wheelchairs fell from $32 million every month to $7 million—a 78 percent decrease.
The Medicare Claims System Is Designed for Fraud, Waste, & Abuse
By law, Medicare must pay most of its claims within 30 days. In that short window, it is supposed to filter out the fraud and uncover claims where the diagnosis or the prescription is bogus.

The system attempts to ameliorate the damage through a “pay and chase” policy. The bill is paid, then it is reviewed. Only a tiny fraction of claims — 3 percent or less — are reviewed by a live person before they are paid. The rest are reviewed only after the money is spent. If at all.
The whole Medicare claims process is set up as an honor system for the richest program managed by the U.S. government. It is a thief’s dream.
Medicare Prior Authorization Test Program
In March 2017, CMS (Center for Medicare & Medicaid Services) designed a test program for preauthorization for fee-for-service Original Medicare. In the month of March, the GAO (U.S. Government Accountability Office), in a Senate report, estimated a savings of $1.1 to $1.9 billion when preauthorization was used that month. The report estimated the federal government made an estimated $36.2 billion in improper payments for the Medicare fee-for-service program from July 2015 to June 2016.
The committee’s recommendation became the report’s title— “CMS Should Take Actions to Continue Prior Authorization Efforts to Reduce Spending.” The prior authorization programs created to monitor and measure improper payments were discontinued and never recommissioned.
Original Medicare Fee-For-Service vs. Medicare Advantage
The government created Medicare in 1965. It had been a long-time project of the Democratic Party. CMS (Center for Medicare & Medicaid Services), Department of Health & Human Services, and Social Security Administration are government agencies. Politicians of all political parties exercise control and funding over these agencies and programs. The agencies are staffed by thousands of bureaucrats and government union workers. A tremendous amount of various and conflicting self-interests, power, and money are all mixed together.

To save Medicare from ballooning budgets and to offer an alternative to citizens, the same politicians, programs, and agencies partnered with private insurance companies to control spending and improve patient care. What is now known as Medicare Advantage began back in the 90s.
The two ways of doing government healthcare for seniors are in competition. Politicians view the world through different ideologies and support policies and programs based upon their political views. Those who support the various political ideologies will support or attack these two platforms accordingly.
It is vital to find all the relevant facts, make your own comparisons and analysis, and determine where lies the truth and the better path.

The amount of the Medicare Part A Hospital deductible for 2023 is vital because other numbers are based upon it. The Part Hospital A deductible in 2023 is more than just a dollar amount. The Part A deductible for Medicare drives the other copays, coinsurance, and deductibles.
Part A not only covers inpatient hospital stays. Medicare Part A and the deductible for 2023 include Skill Nursing Facilities, Home Healthcare, and even Hospice. These services have their own particular copays.
Payroll Taxes Pay For Medicare Part A
Payroll taxes support Medicare Part A. Each pay period, the taxes deducted from your check go into a special trust fund to cover Part A expenses. The payroll tax (or FICA) is currently 1.45% of your gross wages. There is no limit to the 1.45% tax. In other words, your entire income, even if it is $400,000, is subject to the 1.45% tax.
While the revenue from payroll taxes to the federal government is enormous as an absolute number, it is finite and limited in relation to the costs that Medicare Part A must support. Consequently, deductibles, coinsurance, and copays for the hospital, skilled nursing, home health care, and hospice are designed to offset any shortfall in rising expenses and insufficient tax revenue.
Medicare Part A Increases In 2023 Increase Supplements
Part A claims generally are more considerable than Part B claims. When the Center for Medicare & Medicaid Services (CMS) increases the deductibles and copays for Part A, the insurance companies need to cover more with the Medigap and Medicare Advantage policies. Their costs and risk go up in relation to Medicare’s higher deductibles and copays. They pass those costs on to the consumer through increased premiums and larger copays.
How Much Is Medicare Part A Deductible?
The Medicare Part A deductible for 2022 was $1,556 per benefit period. The new Medicare Part A deductible for 2023 is $1,600 per benefit period, which is a 3% increase.

The key to Medicare Part A deductible is the benefit period. The benefit period restarts after 60 days without inpatient care. There is no limit to the number of benefit periods a patient may experience in a year. Consequently, the insurance company that covers this risk has almost unlimited liability.
After the Part A deductible is met during the benefit period, the patient has 60 days at no cost in the hospital. If the patient remains as an inpatient on day 61, his copay is $400 daily from day 61 to 90 for 2023. As you can imagine, the 60-day stay is more than sufficient for most people.
Lifetime Reserve Days
However, for those who need even more inpatient hospital care, there is a one-time amount of 60 lifetime reserve days. The patient may draw upon this pool of days when he has exceeded the initial 90 days. The accompanying copay for these 60 lifetime reserve days is $800 per day. Once these days are exhausted, then you are responsible for all costs on day 150 and beyond that year.
These numbers are strictly Medicare Part A deductible, and copays for 2023 without a Medicare Supplement or Medicare Advantage plan included.

Medicare Part A Include Skilled Nursing Facilities
Medicare Part A for 2023 includes skilled nursing facilities. Skilled nursing is required when the level of care is more than can be provided by home health care visits or a patient going to a facility several times a week. Skilled nursing is for intense rehabilitation requiring several hours of care per day.
The Medicare Part A deductible for 2023 is zero for the first twenty days in the skilled nursing facility, but from day 21 to day 100, the copay increased from $194.50 to $200 daily in 2023.
Medicare Supplements fill in the gap for skilled nursing facility care. Medicare Advantage plans provide smaller daily copays, but the cost of a supplement or advantage plan increases when more of the burden is passed on to the plan.
Home Healthcare & Hospice Go With Part A
Home health care is also part of Medicare Part A. It remains the same with zero copays, and durable medical equipment remains at 20% coinsurance.
While these numbers remain the same, inflation affects the amount the insurance company must make up to cover the 20% of durable medical equipment like walkers, wheelchairs, hospital beds, CPAP machines, oxygen tanks, and other medical equipment. More liability means higher premiums in the long run for Medicare Supplements.
Medicare Part A includes hospice. The Medicare Part A for hospice in 2023 is the same as well. Medicare almost completely covers hospice. There are some minimal copays for medications.

At the end of each year, the Center for Medicare & Medicaid Services (CMS) releases the new numbers for Medicare Part A and Part B. The insurance companies follow suit with their adjustments over the course of the year. Understanding the changes and how all the numbers work together gives you a better appreciation for how Medicare works and enables you to anticipate increases and plan your healthcare budget. You can adjust your strategy for your Medicare Supplement, Medicare Advantage plan, or Medicare Part D prescription drug plan when you know how it works. The first number to learn is the Medicare Part A deductible for 2023.
 Medicare Denial
Medicare Denial
One of the biggest fears people have when they come to my office, for example, is backbreaking medical bills. A major concern is: ‘Will Medicare cover . . . . ? You can then imagine how clients react when Medicare does not cover a bill.
Fortunately, I do not get many frantic phone calls from clients who are upset because Medicare denied a claim. Medicare denials, however, do happen. Most of the time, a Medicare denial is simple to handle. At other times, there needs to be a formal Medicare appeal process.
First of all, what is a Medicare denial of coverage? A denial is when Medicare, the Medicare Advantage plan, or the Medicare Part D prescription drug plan refuses to cover and pay for a particular procedure or medication.
This denial may come in many forms. The Medicare denial letter may come before the procedure. The doctor’s office calls to get prior authorization, and the procedure is denied. The denial may come after the procedure is performed, and Medicare denies payment. The patient may be in the midst of the procedure, such as staying in a hospital, skilled nursing facility, or receiving home health care. Medicare refuses to cover additional time in the institution.
Understanding How Medicare Coverage Works
One time I had a client who had a serious shoulder problem. The doctor recommended an MRI. The Medicare Advantage plan denied the treatment. They suggested a less expensive treatment to repair the situation–physical therapy.
The client called me to complain. After a few phone calls with the insurance company, they explained physical therapy was far less expensive, and it may achieve the same result without being so intrusive as surgery.
The purpose of the MRI was a preliminary to surgery. The client later said he had no intention of having surgery at his age. He simply wanted to know what was wrong with his shoulder.
Most situations can be easily resolved without going through the Medicare appeal process.
Medicare and the insurance companies will almost always take the least expensive and intrusive route when prescribing treatments. A denial is not always a denial.
Medicare Summary Notice
Medicare sends a quarterly statement, the Medicare Summary Notice (MSN). It lists all the procedures you have had in the past quarter, the cost, and the payment. The MSN is not a bill. It is a notice that people with Original Medicare get in the mail every three months for their Medicare Part A and Part B-covered services. The MSN shows all services and supplies billed to Medicare during a 3-month period, what Medicare paid, and the amount you owe. It will also show denials.
Another client of mine was denied access to a Skilled Nursing Facility (SNF). She had had a knee replacement. Usually, patients go directly home after a knee replacement. In her case, the rehabilitation was not going well. Her home was a small apartment with pets. She lived alone. When Medicare denied the request, we had the doctor put she was a “fall risk” in the letter to Medicare, and he laid out the reasons. The appeal was quickly granted.
Many times it is not an issue of denial of coverage; it is poor communication. In this instance, we did not even use the formal Medicare appeal process. It was just a letter of clarification from the doctor.
Medicare Appeal Process
If you disagree with the Medicare coverage determination, you can appeal the decision. An appeal is a formal way of asking Original Medicare (Part A & Part B), the Medicare Advantage Plan, or the Part D plan to review and change the coverage decision.
A Medicare appeal is different than filing a grievance or complaint with Medicare. Grievances deal with the quality of coverage, the listing of medications on formularies, or access to medical personnel and institutions.
An appeal asks Medicare to pay for a procedure it denied. For example, an appeal may ask Medicare to extend a patient’s stay in a skilled nursing facility beyond her situation’s customary period. An appeal may ask Medicare to approve a more expensive procedure than is ordinary for the situation.
As a Medicare beneficiary, you have a right to file an appeal. There are five levels to an appeal. Medicare Advantage and Part D plans mirror the same process. If you are dissatisfied with the decision at the last level, you may proceed to the next level. The denial letter includes instructions on how to apply.
 Medicare Redetermination Form For Appeal Process
Medicare Redetermination Form For Appeal Process
Once you are aware of a Medicare denial of coverage with which you disagree, you need to act. You have 120 days to respond.
Download and complete the Redetermination Request Form. The form goes to the Medicare contractor, or you can write your own letter. Remember to include all the essential information. You will receive a Medicare Redetermination Notice within 60 days after Medicare, or the contractor receives the letter. If you disagree with that decision, you have 180 days to appeal to Level 2.
Medicare Reconsideration Request Form
A Qualified Independent Contractor (QIC) administers the 2nd Level of appeal, not Medicare or the insurance company contracted with Medicare. It is a third party that reviews the case. The appeal process is the same as the previous. There is a designated form—the Medicare Reconsideration Request Form. The decision is rendered in 60 days or less.
Administrative Law Judge
If you disagree with the decision from the 2nd Level, you may proceed to the 3rd Level, which is the Administrative Law Judge Hearing. You have 60 days to make this appeal.
Of course, there is a specific form for this appeal, and it is sent to the Office of Medicare Hearings and Appeals (OMHA) Central Operations. The address is on the form. If you are not satisfied with this decision, you may appeal to the 4th Level within the 60 days allotted.
 Medicare Appeals Council
Medicare Appeals Council
The 4th Level in the Medicare appeal process is like the others. The council has 90 days to respond. If you still are not satisfied, you may take your appeal to a district court within 60 days.
Federal District Court Judicial Review
The 5th and final Level is the Federal District Court Judicial Review. Cases that make it this far usually significantly impact Medicare when won. This is the “supreme court” of the Medicare world.
Medicare Appeal Process Help
Please, call when you have questions about appeals. We can help steer you in the correct direction. You can also call Medicare directly. They are open 24/7. They will mail or email you the required forms as can we.
If your appeal is to an Advantage or Part D plan, you call them directly. Their appeal process mirrors the Medicare appeal process and is usually less formal. You can also call the local SHIP (State Health Insurance Assistance Program) office to assist you.
Expedited Review
Many times speed is essential in a decision. The Medicare beneficiary may request an expedited review.
For example, you are in a hospital. The doctor thinks you need an additional three days because your body is not recovering from the treatment at the average speed. It is three days beyond what Medicare allows. Medicare will deny payment. The hospital files the Medicare Redetermination Form requesting three extra days. They also request an expedited review, which means Medicare will make a decision within 72 hours. An expedited review for medications on a Part D plan is 24 hours.
The Beneficiary and Family-Centered Care-Quality Improvement Organization (BFCC-QIO) is the department that will help with appeals.
Handling NO!
No one likes no. My five-year-old granddaughter does not like no. My wife certainly does not like no. Most of my clients don’t like no, but we hear it, even from Medicare at times.
No, however, does not necessarily mean we are done. There is a process. I am happy to help clients navigate the hurdles and obstacles of the Medicare appeal process. Sometimes there is no need for the process. It is just a matter of talking to the right person or better communication.
Getting Medicare and your Medicare insurance to work for you is what training and years of experience enable us to do. We will walk you right through the Medicare appeal process.

I remember when the hospital staff explained my mother’s Medicare coverage to me. I kept asking, “What does Part A cover? How is Part B different?” I couldn’t remember anything. I’m sure the stress of my mother dying had a lot to do with it, but it seemed like I was a child going back to school trying to learn my A, B, C’s. I should have called the Medicare coverage helpline at 800-633-4227, but I didn’t know.
 The Alphabet of Medicare Coverage
The Alphabet of Medicare Coverage
Understanding the building blocks of how Medicare works begins with understanding the Medicare alphabet. We start with A. A is not for Apple but for Medicare Hospital coverage. When Medicare first started in 1965, there was only hospital coverage. Hospital costs are generally the largest. Seniors in the 1960s were being devastated by hospital medical costs and the availability of insurance at the time. Congress created Medicare.
Medicare Part A costs nothing if you have worked and paid the Medicare tax for at least 40 quarters (or 10 years). The quarters do not need to be consecutive, only total up to 40 quarters.
Medicare Part A Hospital Coverage
Part A covers the hospital 100% for 60 days after the deductible is met. Currently, the Part A deductible for 2022 is $1,556. This deductible is per event in a 60 day period. It is possible to have more than one deductible in 60 days if the medical issues for hospitalization are unrelated. For example, you had a heart attack one month and fell off a ladder the next month. Two unrelated events sent you to the hospital within 60 days, and so you paid two $1,556 deductibles. Not likely, but certainly possible.
 Part A Coinsurance
Part A Coinsurance
If you continue to remain after the first 60 days in the hospital, you have a $389 copayment per day from day 61-90. Again, hospital stays of that length are infrequent. Nonetheless, you are still responsible for that cost if it occurs and you have no other insurance, like a Medigap plan.
Part A Lifetime Reserve Days
If you go beyond 90 days, there is a bank of “lifetime reserve days” from which you can draw. You have a total of 60 lifetime reserve days. These lifetime reserve days are exactly what it means. Once the 60 days are used up, you have no more. You pay 100% of the inpatient hospital costs after the 90 days going forward.
Medicare Hospital Coverage
Part A covers everything that happens in the hospital during your stay, except some doctor visits. As for the copays, coinsurance, etc., a Medicare Supplement (Medigap) policy may cover those costs. Medicare Advantage/Part C configures the copays in various ways depending upon the policy. Medigap and Medicare Advantage are covered in detail in other blogs.
 Medicare Part B Coverage
Medicare Part B Coverage
Part B covers everything other than inpatient stays at the hospital, even if a procedure takes place at a hospital. Medicare Part B coverage excludes medications usually unless the medications are the type administered in a doctor’s office or through durable medical equipment, such as insulin through an insulin pump.
Medicare Part B coverage is for doctor visits and outpatient procedures. The doctor visits can also be the doctor visits while in the hospital.
Part B Costs
Medicare Part B coverage does cost something. Currently, the Part B premium is $170.10 for 2022 for most people. The Part B premium had the most significant increase in Medicare’s history from last year, $148.50.
For approximately 4% of the Medicare demographic, the Part B premium is more because of your income. Please, confer our blog on the IRMAA Tax.
Part B covers 80% of the doctor and outpatient costs without limit. There is no upper dollar limit on Medicare benefits as long as the procedures are “medically necessary” and occur at a Medicare-approved facility or with a doctor who accepts Medicare assignment. On the flip side, however, you also have a 20% coinsurance you must pay, which has no cap or limit. That is drastically different from what you probably experienced with your employer’s health plan. Most plans have a maximum out-of-pocket (MOOP). Those MOOPs may be as high as $10,000 or $15,000, but you have a cap at some point. Medicare Part B coverage is an unlimited 20% coinsurance. There is no cap or limit. Another reason to get some sort of additional insurance coverage.
Medicare Part C Coverage
 Keeping with the alphabet theme, Medicare Part C coverage is next. The Balanced Budget Act of 1997 (BBA) established a new Part C for the Medicare program. Part C was known then as Medicare+Choice (M+C) program, which started in 1999. Many times clients will ask if Medicare Part C or Advantage are new. There have been many iterations of Medicare Advantage with variable names. Part C was only in limited markets when it first began. Omaha, Lincoln, Council Bluffs, eastern Nebraska, and Western Iowa were not the hotbeds where the Part C programs were initiated or grew. Of course, that is changed.
Keeping with the alphabet theme, Medicare Part C coverage is next. The Balanced Budget Act of 1997 (BBA) established a new Part C for the Medicare program. Part C was known then as Medicare+Choice (M+C) program, which started in 1999. Many times clients will ask if Medicare Part C or Advantage are new. There have been many iterations of Medicare Advantage with variable names. Part C was only in limited markets when it first began. Omaha, Lincoln, Council Bluffs, eastern Nebraska, and Western Iowa were not the hotbeds where the Part C programs were initiated or grew. Of course, that is changed.
The Medicare+Choice was renamed Medicare Advantage (MA) under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA). The MMA updated and improved the choice of plans for beneficiaries under Part C and changed the way benefits are established, and payments are made. The MMA broadened Medicare Part C coverage. MMA enabled Medicare Advantage to also include Medicare Part D prescription drug coverage for the first time.
Medicare Advantage Design
Medicare partnered with health insurance companies to create Medicare Advantage plans. The Part C plans need to offer at least as much as Original Medicare Part A & B in the overall actuarial cost sense, but they could also offer more, such as dental, vision, hearing, etc. Medicare regulates and monitors the plans. Medicare Part C coverage must be as good as Original Medicare.
The Part C plans are Medicare. That is why it is called “Medicare Part C.” Medicare Advantage is Medicare administered by a private insurance company approved by Medicare.
Medicare Part C/Medicare Advantage is usually offered at little or no premium over the Medicare Part B premium payment. The plans, however, have copays and coinsurance with a maximum out-of-pocket for the total copays.
Medicare Part D Coverage
The final letter in this Medicare alphabet is Part D for Medicare prescription drug coverage. Until 2003 Medicare did not sponsor prescription drug coverage, though some supplements had their own private programs. After the MMA legislation, Medicare worked with insurance and pharmaceutical companies to establish drug plans that provided medications at reasonable rates and distributed the costs fairly among participants. The premium for each plan varies.
The Dreaded Donut Hole
 The Medicare coverage for Part D plans has four phases. To start, there is the deductible. The current deductible on most plans in 2022 is $480. During the second or initial phase, the beneficiary covers about a fourth of the actual cost of the medications once the annual deductible is met. The plan pays the other three-fourths.
The Medicare coverage for Part D plans has four phases. To start, there is the deductible. The current deductible on most plans in 2022 is $480. During the second or initial phase, the beneficiary covers about a fourth of the actual cost of the medications once the annual deductible is met. The plan pays the other three-fourths.
If the client and the plan payout $4,430 in copays and cost from the plan, then the Medicare beneficiary moves into the 3rd phase, which is the Gap (or Donut Hole). At this point, the pharmaceutical companies discount the medications to 25% of their actual cost. The beneficiary then pays the total cost of the drugs until he reaches $7,050 of combined payments out of his pocket.
Then he has crossed over to the 4th and final stage–Catastrophic. In the catastrophic phase, you will pay the greater of 5% of drug costs or $3.98 for generic and $9.98 for non-generic medications. You will pay these amounts until the end of the year. On the first of the year, the whole cycle starts over.
What Medicare Covers and What Medicare Does Not Cover
Medicare coverage is easier to define by saying what it does not cover.
No Long-Term Care
Original Medicare–just Part A and Part B–does not cover long-term care or is sometimes referred to as custodial care. Medicare covers skilled nursing facilities, and skilled nursing facilities are mostly long-term care facilities. But the purpose of the skilling nursing facility with Medicare is in the service of curing an illness and is only temporary. Skilled nursing facility care is limited to 100 days. It is not custodial care.
Custodial care is needed when you can no longer perform activities of daily living, such as bathing, toileting, transferring, dressing, eating, etc. Medicare does not cover long-term care for custodial purposes.
No Dental
Medicare does not cover routine dental care, such as teeth cleaning, fillings, extraction, crowns, root canals, etc. Yes, many Medicare Advantage / Part C plans cover dental but not Original Medicare Parts A & B. This is a common confusion.
Medicare Parts A & B. This is a common confusion.
In keeping with the dental theme, Original Medicare does not cover dentures. Some Medicare Advantage plans do. Medicaid in many states covers dentures, but Medicare does not, though you may purchase a separate and private dental plan for that purpose.
No Cosmetic Surgery
Original Medicare does not cover cosmetic surgery. Breast augmentation, hair implants, botox injections are not on the list of Medicare authorized treatments. That being said, there are exceptions depending upon circumstances. In other words, how “medically necessary” the treatment is.
One of my clients called me ecstatic because she was approved for breast reduction. I must admit breast reduction was not one of the things I gave a great deal of thought to. I remember my grandmother explaining to me once in an unusual turn of events the challenges well-endowed women have, but it was never something I thoroughly appreciated. However, my client explained to me why it was “medically necessary,” and Medicare concurred. The breast reduction was approved, but generally speaking, there is no Medicare coverage for cosmetic surgery.
No Acupuncture
Original Medicare does not cover acupuncture. I never would have imagined how popular acupuncture is, but I have gotten that question many times over the year. Medicare Part A or B do not cover acupuncture, though more and more Advantage plans offer some acupuncture, usually in conjunction with chiropractic care.
No Hearing Aids
Original Medicare does not cover hearing aids or their fitting. Anyone who has even a remote experience with hearing aides knows how incredibly expensive hearing aides are. Neither Part A nor B covers hearing aides. Again many Advantage plans do cover various aspects of audiology and hearing aids. Thus the mass appeal of Medicare Advantage over Original Medicare.
No Routine Foot Care
 Original Medicare does not cover “routine foot care.” Yes, Medicare covers feet and the rest of your body, but “routine foot care” is a particular thing. Primarily routine foot care involves cutting or removing corns and calluses, trimming, cutting, or clipping nails, and hygienic and preventive maintenance, like cleaning and soaking your feet. This type of care is vital for some people with specific health issues to prevent infection or damage to their feet. Routine foot care is absolutely critical for those with diabetes and neuropathy to avoid infection and other problems that could result in amputation. Neither Part A nor Part B covers routine foot care. Many Medicare Advantage / Part C plans do cover routine foot care.
Original Medicare does not cover “routine foot care.” Yes, Medicare covers feet and the rest of your body, but “routine foot care” is a particular thing. Primarily routine foot care involves cutting or removing corns and calluses, trimming, cutting, or clipping nails, and hygienic and preventive maintenance, like cleaning and soaking your feet. This type of care is vital for some people with specific health issues to prevent infection or damage to their feet. Routine foot care is absolutely critical for those with diabetes and neuropathy to avoid infection and other problems that could result in amputation. Neither Part A nor Part B covers routine foot care. Many Medicare Advantage / Part C plans do cover routine foot care.
One of my clients was quite a large man. He was also diabetic with many other complications. He could not trim his own toenails. He very much needed podiatric care. As a matter of fact, he was embarrassed by the whole situation and neglected the trimming for a while. As you can guess, his toes became infected, which resulted in losing some toes.
While these are not small or unimportant areas of health, Medicare does not cover them. Medicare, however, covers virtually everything else that is “medically necessary.”
Medicare Coverage For Experimental Treatments
Experimental treatments or clinical trials, however, are in their own category. Medicare may cover experimental treatments. Though that being said, most “experimental” treatments are voluntary programs supported by funding from pharmaceutical companies or other institutions. Those can only be spoken to on a case-by-case basis. Medicare may cover some or all of the treatment depending upon the type of treatment. Indeed, those aspects Medicare typically would be covered.
Many years ago, a man was referred to me because he had had some difficulty around this issue of clinical trials. He had been on a Medicare Advantage plan with a previous agent. He could only get into the clinical trial without paying for a large part of it was to return to Original Medicare. After much difficulty with Medicare, Medicare granted him an exception to return to Original Medicare without waiting for the Annual Election Period in October.
The next problem was finding a Part D prescription drug plan that would cover his medications. That’s where I came in. That matter was straightforward, but the difficulty he had getting some Medicare coverage for the experimental treatment was interesting and scary, which ultimately prolonged his life by many years.
More Information in Other Blogs
There is much more to say about Medicare. There is, even more, to say about Parts A, B, C, & D; however, over 2,000 words in just this article is more than enough for anyone to read about the wonders of Medicare in a brief sitting. I recommend searching in the search tool at the top of the blog section for more information on each Part of Medicare and the sundry-related topics, but before going on, you must understand the foundational building blocks of Medicare.

Christopher Grimmond
When you need help understanding Medicare, give us a call at 402-614-3389, or the Medicare coverage helpline is 800-633-4227. Medicare is open 24/7.
Medicare Advantage or Medicare Part C is another way to receive Medicare. “Original Medicare” is a combination of Medicare Part A and Part B. It is called “Original Medicare” because that was its first plan in the late 60’s. Medicare Part A was hospital insurance and Medicare Part B was added later. It included doctor visits and outpatient procedures. Some people call it traditional Medicare. It became “Original Medicare” when a new form of Medicare was created–Medicare Advantage, also called Medicare Part C. What is the advantage of Medicare Advantage over Original Medicare?
The Advantage of Medicare Advantage vs Original Medicare
Let’s explain “Original Medicare” first. Medicare Part A covers hospital stays. The Part A has a deductible. It is currently $1,340 for every hospital stay for the same event in a 60 day period. If a completely unrelated event lands you in the hospital, e.g., car accident, heart attack, stroke, etc., even within the first events 60-day period, you will still pay the $1,340 deductible for those unrelated events. That kind of deductible schedule could add up to a significant cash outlay in a year. Likewise, Medicare Part B exposes you to a great deal of risk. While Medicare Part B pays 80% of doctor and outpatient costs, your 20% co-insurance has no cap on it. There is no maximum out-of-pocket. Sky is the limit. If you have a million dollars worth of bills under Part B, 20% is $200,000.
 Maximum Out-Of-Pocket
Maximum Out-Of-Pocket
The Advantage of Medicare Advantage is a maximum out-of-pocket. The highest maximum out-of-pocket for Medicare Advantage plans in 2018 is $6,700. Some plans maximum out-of-pocket are much less, depending on the area, the company, and the type of plan. However, the easiest and clearest difference between Original Medicare and Medicare Advantage is a definite limit on what you pay out of your pocket. Medicare Advantage has a maximum out-of-pocket. Original Medicare does not.
Minimum Co-Payments
Each Medicare Advantage Plan has its own schedule of co-pays, deductibles, and co-insurance. One co-pay that is standardized in all plans is the emergency room visit. In 2018, the emergency room visit co-pay is $80. I would rather pay $80 with a Medicare Advantage plan rather than 20% of any amount on Original Medicare. I broke my arm a number of years ago biking. My emergency room visit was $3,000. The advantage of Medicare Advantage I think is an $80 co-pay rather than 20% bill–$3,000 x 20% = $600.
 Part D Prescription Drug Included
Part D Prescription Drug Included
With Original Medicare, you still need to get a Medicare Part D prescription drug plan, even if you don’t take any medications. Otherwise, you will be penalized when you eventually do enroll in a Medicare Part D plan. The Part D plan is generally included in a Medicare Advantage plan at zero or little cost. If you purchase a Part D plan, you may pay between $21–$100 per month. The advantage of Medicare Advantage is paying zero or very little for your drug plan.
Vision and Dental
Mo st Medicare Advantage plans have additional benefits, such as vision, dental, and over the counter items. How would you like to get your teeth cleaned twice a year at zero cost? That is all most people are interested in when it comes to dental usually. They don’t want to spend $50 a month on a dental plan when cleanings are all they really want or need.
st Medicare Advantage plans have additional benefits, such as vision, dental, and over the counter items. How would you like to get your teeth cleaned twice a year at zero cost? That is all most people are interested in when it comes to dental usually. They don’t want to spend $50 a month on a dental plan when cleanings are all they really want or need.
Compared to Original Medicare, the advantage of Medicare Advantage makes complete sense. It limits your maximum out-of-pocket, combines Part D at little or no cost most times, includes extra benefits, like dental and vision. There are usually many plans in your area. Here is Omaha there are eleven Medicare Advantage plans among five insurance companies. You should be able to find something that fits your needs among that variety. Call us to find out 402-614-3389.
When people arrive at the doorstep of Medicare at age 65, they are confronted with the daunting task of picking a Medicare plan. Most people find picking Medicare plan overwhelming and confusing.
100’s of Supplements to Pick From
Insurance companies offer hundreds of different Medicare supplements, Medicare Advantage plans, and Medicare Part D prescription drug plans. Picking Medicare plan means choosing between Medicare supplements and a Part D prescription drug plan OR Medicare Advantage/Part C. Next picking Medicare plan means choosing the plan type. Medigap plans range from plan A through the alphabet to plan N, which doesn’t include a Part D drug plan. The drug plans can be a little simpler because you can use the Medicare tool to narrow down the selection. The Medicare calculator bases the plan selection upon the prescriptions you enter into the system. The calculator picks the Medicare Part D plan that will cost the least in total costs for you. On the other side, Medicare Advantage plans consist of a wide variety of co-pays, co-insurance, deductibles, and maximum out-of-pocket costs and amounts that may or may not include a Part D plan.
Foreign Language of Medicare
Medicare itself is like a foreign language of Part A, Part B, and Part D with rules around enrollment that includes penalties when you do not comply. The Medicare.gov website is meant to be helpful, but the shear amount of information, jargon, legalese makes it a barrier to entry rather than a door. Even the Medicare handbook is hundreds of pages. Its size makes the evaluation of information almost impossible.
 The Pain of Picking Medicare Plan
The Pain of Picking Medicare Plan
As a consequence, picking a Medicare plan is a frustrating and painful process for people. That is why I take people through a 3-step process. 1.) There is a brief, foundational explanation of Medicare and how it works. 2.) Look at ALL of the plans, but in an organized and ordered fashion. The first step helps you evaluate the plans. I share the story behind each company from my fifteen years of insurance experience because each company has a history in the market. 3.) I find out about you. Everyone is unique. Some people are risk takers. Others are not. Some have health concerns that are foremost of mind. Others do not have any.
Logical Process
The logic of the process enables people to narrow down choices and make the best one for them. I ask questions as we go along. Test and probe. Explain aspects of the plans as we go through each. Constantly test for understanding. So the process of picking a Medicare plan becomes clearer as we move through it. I generally meet with people twice. The first time is usually months before they can do anything. There is no pressure to make a decision or ‘buy right now.’ Clients have time to think, collect more information, verify what they’ve learned, talk with confidants. The next time we get together is to review with updated information. That is the time for picking a Medicare plan. By then you are comfortable and confident with your decision because your decision is well informed. It is logical. The decision is made over time without pressure. You know what you are doing when you pick your Medicare plan.
If you would like to go through this process, there is not cost or obligation. Call 402-614-3389 to find out more.
We’ve all experienced that less than happy holiday vacation spent ill. What’s worse is getting sick abroad and worrying about Medicare insurance coverage. If you’re planning a winter getaway, check out and share our healthy Medicare travel tips to ensure your vacation goes off without a hitch.
Prevention
Whether you’re going foreign or domestic, Medicare travel tip #1. Always research your destination. Even learning about a stomach bug going around could help save your trip. Also be sure to take a look into potential health facilities by contacting the U.S. embassy in the country you’re going to visit or by getting help from your hotel. Know and have the contact information for the hospitals and urgent care centers that could be available to you during your trip.
Common Traveling Illnesses
 Important Medicare travel tips is to know what to avoid on your trip. Here are some common illnesses you can bring back from your vacation:
Important Medicare travel tips is to know what to avoid on your trip. Here are some common illnesses you can bring back from your vacation:
- Malaria – Often found in tropical climates, Malaria is contracted though an infected mosquito bite. Although the disease has flu-like symptoms, it may become deadly. The CDC (Centers for Disease Control and Prevention) has the need-to-know information on Malaria for travelers.
- Traveler’s Tummy – One of the most common maladies foreigners experience when traveling abroad. Traveler’s tummy is common throughout Asia, Africa, Latin America and the Middle East. You can learn more about the gastro-intestinal sickness and how to avoid it from the CDC.
- Zika Virus – Zika is something we’ve all heard about on the news in the past year. Symptoms can range from flu-like to joint pain and rashes. It’s been linked to Asia, Brazil, Central America, Mexico, The Caribbean and The Pacific Islands. This CDC Infographic has tips on preventing Zika while traveling abroad.
You can read up on what to specifically watch out for depending on where you’re going on the travel section of the CDC website.
Check Your Coverage
Compare Plans and Explore Your Options
 Your health coverage will vary depending on your Medicare plan. Original Medicare will usually only provide coverage within the U.S. Some Medigap plans have travel coverage. Some Medicare Advantage Plans may as well, but you’ll have to check your specific plan.
Your health coverage will vary depending on your Medicare plan. Original Medicare will usually only provide coverage within the U.S. Some Medigap plans have travel coverage. Some Medicare Advantage Plans may as well, but you’ll have to check your specific plan.
If you need some help navigating your Medicare coverage options, our agents can help and are available all year-round.
Doctor Knows Best
Before traveling, meet with your doctor to have a check-up, talk about any health concerns you may have, if you’ll need any vaccinations, etc. Your physician should be able to inform you on any must-know health concerns in regards to wherever you’re going.
Pack Smart Most Important of Medicare Travel Tips
 Pack weather-friendly, and don’t forget your necessary prescriptions and medications in your carry-on luggage. That is the most important of Medicare travel tips. If you’re traveling by car, keep your meds in an easy-to-access designated location. If you have any special medical supplies that you need to use, get a note from your doctor that explains why you need them. It’s better to be safe than sorry! If you need help thinking through these Medicare travel tips or you want to invest in travel insurance, give us a call at OmahaInsuranceSolutions.com 402-614-3389
Pack weather-friendly, and don’t forget your necessary prescriptions and medications in your carry-on luggage. That is the most important of Medicare travel tips. If you’re traveling by car, keep your meds in an easy-to-access designated location. If you have any special medical supplies that you need to use, get a note from your doctor that explains why you need them. It’s better to be safe than sorry! If you need help thinking through these Medicare travel tips or you want to invest in travel insurance, give us a call at OmahaInsuranceSolutions.com 402-614-3389
With these tips, you should be enjoying your vacation in no time. Happy travels!
One of the most common questions we receive is: “Am I eligible for Medicare?” Well, there’s no black and white answer to Medicare eligibility. Your Medicare eligibility may depend on several different situations. Luckily, we make Medicare easy—this post will show you how and when to apply for Medicare based on your unique situation.
Medicare Eligibility
You become eligible for Medicare when you turn 65 (or younger if you have certain disabilities or diseases). If you or your spouse ha worked in the U.S for more than 10 years, you qualify for Medicare benefits.
Make Comparing Medicare Plans a Breeze
Medicare has four parts: Medicare Part A , Part B, Part C and Part D. Parts A and B include doctor and hospital insurance. Together, Parts A and B are referred to as Original Medicare.
You can apply for Original Medicare the year you turn 65, but only if you meet one of the below requirements:
- You’re eligible to receive Social Security benefits or Railroad Retirement benefits.
- You’re already receiving your retirement benefits from Social Security or Railroad Retirement.
- You or your spouse are covered for Medicare through government employment.
Medicare eligibility doesn’t mean you have to start using it. People are different—some may be ready and waiting to get their Medicare benefits and some may not need coverage yet. If you’re getting ready to turn 65, read on to see your Medicare options.
I’m Turning 65 This Year…
If you’re turning 65 soon, you may want to do one of many things depending on your situation:
- You’re retired
- You want to retire
- You have other health coverage
- You are still working and don’t want to retire yet
See the options for your situation below.
…and Want to Apply for Medicare
If you’re planning to receive retirement benefits before or at the age of 65, apply for Medicare at the same time or at least 3 months before your birthday. That way you’ll become automatically enrolled in Medicare when you turn 65.
…and Am Still Working
If you’re still working when you turn 65, you might want to keep your current health coverage provided by your employer. You can keep your current coverage and still apply for Medicare Part A (most people don’t have to pay a premium for Medicare Part A, so you won’t have to incur a cost).
However, you may consider deferring Medicare Part B to avoid the monthly premiums. We recommend checking with your employer to see how your current coverage may work with Medicare Part B before you make any decisions.
…and Am Covered by My Spouse
If you’re still getting health coverage from your spouse that’s working, refer to the paragraph above.
…and Did Not Pay Medicare Taxes While Working
There are some cases where individuals are 65 and older and a permanent resident of the United States, but they (or their spouse) did not pay Medicare taxes while working. If this is your situation, you still have options.
- Medicare Part A with premiums
- You can purchase Medicare Part A.
- Medicare Part A without premiums
- You’re receiving Railroad Retirement
- Kidney transplant patients/dialysis patients may still be able to receive benefits per special circumstance.
 I’m Over 65 and Haven’t Enrolled in Medicare
I’m Over 65 and Haven’t Enrolled in Medicare
If your 65th birthday has come and gone, you still have several options and opportunities to receive your healthcare.
- If you’re within 3 months of your 65th birthday, you still qualify for enrollment under your initial enrollment period.
- Otherwise, you can wait until general enrollment (January 1 – March 3).







