 Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
Maximizing Medicare: Understanding Coverage for Hospice in Skilled Nursing Facilities
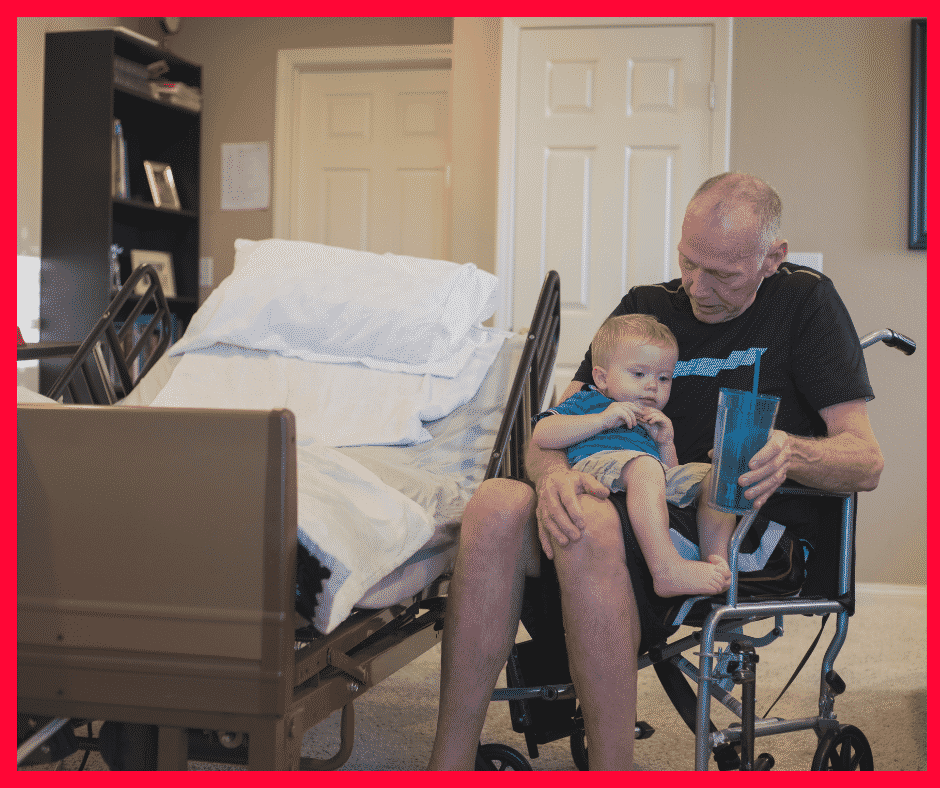
Do you or a loved one need hospice care in a skilled nursing facility? Understanding Medicare coverage for this essential service is crucial for maximizing benefits and ensuring quality end-of-life care. This article will explore some of the ins and outs of hospice coverage I didn’t know when my mother was in hospice. We discuss the question of whether Medicare pays for hospice in a skilled nursing facility.
Navigating the complex world of healthcare can be overwhelming, especially when faced with a difficult situation like imminent death like I experienced with my mother. That’s why I’m here to break it down for you. I’ll explain what hospice care entails, how it differs from other types of care, and, most importantly, what Medicare covers. With this information, you can be confident in your ability to advocate for yourself or your loved one and ensure that all available resources are utilized.
At Omaha Insurance Solutions, information is power regarding healthcare decisions. We aim to make complex topics accessible, providing you with the tools you need to confidently navigate the healthcare system. So, let’s dive in and discover how Medicare can support you during a challenging time.
What is Hospice Care & Who is Eligible?
Hospice care focuses on providing comfort and support to individuals in the final stages of a terminal illness. The goal is to improve the quality of life for patients by managing pain and symptoms while offering emotional and spiritual support to both the patient and their loved ones. Hospice care can be provided in various settings, including skilled nursing facilities.
To be eligible for hospice care, a person must have a life expectancy of six months or less, as certified by a physician. This certification is required for Medicare coverage, which we will discuss further in the following sections. It’s important to note that choosing hospice care does not mean giving up on treatment altogether. It means shifting the focus to comfort and quality of life rather than curative measures.
Hospice care is a holistic approach that addresses individuals’ physical, emotional, and spiritual needs nearing the end of life. It provides a compassionate and supportive environment where patients receive specialized care tailored to their unique needs. Now that we have a basic understanding of hospice care, let’s explore how it relates to skilled nursing facilities and the coverage provided by Medicare.
Understanding Skilled Nursing Facility Care and Medicare Coverage
Skilled nursing facilities (SNFs) are residential facilities that provide round-the-clock nursing care for individuals requiring more intensive medical attention than they could receive at home. SNFs are equipped with trained healthcare professionals, including nurses and therapists, who can address the complex needs of patients. SNF care is often required when individuals have conditions that require ongoing medical monitoring, such as chronic illnesses or post-surgical recovery. Medicare covers certain SNF services, including skilled nursing care, rehabilitation therapy, and medications. However, it’s important to note that not all services provided in a SNF are covered by Medicare, and this includes hospice care.
Medicare Coverage for Hospice in a Skilled Nursing Facility
 Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, or a skilled nursing facility. However, there are specific criteria that must be met in order for Medicare to pay for hospice care in a skilled nursing facility.
The criteria are the same as for hospice. Firstly, the individual must be eligible for Medicare Part A, which covers inpatient hospital stays, skilled nursing facility care, and hospice care. Secondly, the hospice care must be certified by a Medicare-approved hospice provider. Thirdly, the individual must have a life expectancy of six months or less, as certified by a physician. Lastly, individuals must agree to forgo curative treatments for their terminal illness and receive only palliative care.
The SNF is not primarily providing hospice care. A hospice team coordinates with the SNF to provide the service in the SNF. The location of the hospice care is secondary. The SNF is a location, like the home.
However, there must be a Medicare-covered reason or treatment to be granted admittance to a skilled nursing facility. The SNF is primarily a medical facility for patients to get better. It is not a hospice facility providing room and board, housekeeping, bathroom transfers, etc.
Medicare Hospice Benefits for My Mom
The doctors diagnosed my mother with ovarian cancer in 2012. I was living in Kansas at the time. I wasn’t able to go on doctor visits with her. My brother, Paul, was taking care of my mom. I would get information about her situation, but it was spotty.
My mother was an ‘I’m in charge’ type of person. Phyllis determined the flow of information, and it was sparse.
Talking with your mother about her health when her mortality is so tightly fixed to it is hard. Looking back now, I was a chicken. Who wants to talk about saying goodbye? I didn’t realize the seriousness of her health situation until much later. I assumed she didn’t speak about her own death, and I didn’t know how to initiate the conversation. We were all in different forms of denial.
At the end of 2012, the doctors said there was nothing more to be done. I don’t think I fully grasped what that meant at the time. I also did not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
not anticipate how quickly time would slip away from that moment onward. I’m sure my mother was scared, but she didn’t let on. I stupidly didn’t realize the magnitude of the moment and how she was probably feeling. My own feelings and denial fogged the situation.
My mother was admitted to hospice care (Medicare Hospice Benefits Booklet).
Mom’s Terminal Illness
Nature, in its less than glorious side, took its course rapidly. My mother’s health deteriorated in a few short weeks.
Cancer is a painful disease. The healthcare personnel gave her various painkillers, but even as they did so, we all insanely talked about not wishing to cause addiction. The pain had its own mind.
At various times, my mother’s suffering would be such that she needed to go to the hospital. There, the doctors administered intravenous medications that were faster acting and stabilized her pain level.
During the last visit, it became clear that we could not care for her at home. My father, John Grimmond–who would pass away six months later–was not physically able to care for our mother. I was in Kansas, my other brother, Tom, was in Sioux Falls, and Paul was in Omaha but busy with his career and family.
My mother needed around-the-clock care. We asked, ‘Does Medicare pay for hospice in a skilled nursing facility?’ The real question was whether Medicare would pay for a skilled nursing facility while my mother died. Strictly speaking, Medicare does not pay for custodial care. Custodial care is bathing, feeding, toileting, etc. Medicare doesn’t cover room and board if you get hospice care while in a nursing home or a hospice inpatient facility. That is out of your pocket.
Qualifying for Skilled Nursing Facility Care while on Hospice
The staff at the hospital initially told us that our mother needed to go to a skilled nursing facility (SNF) because they recognized she required more care than we could provide. They informed us that Medicare would provide and pay for hospice care in the Skilled Nursing Facility, but the cost of room and board and custodial nursing care would not be covered, and they were correct. Medicare coverage for skilled nursing when you are in hospice is tricky.
skilled nursing when you are in hospice is tricky.
The fortunate occurrence, however, was the intravenous nature of my mother’s painkillers. Other than a hospital, you can only receive intravenous medication treatment in a skilled nursing facility. The nature of my mom’s treatment triggered a reason Medicare would accept her being admitted to a skilled nursing facility and pay for it.
Medicare does cover skilled nursing care after a qualifying hospital stay of 3-days or more. Intravenous medication administration also requires a skilled nursing facility. A home health care nurse showing up several times at home would not be adequate. Also, my mother needed physical therapy to improve her strength after the reaction to the pain. From Medicare Part A and Part B, there were sufficient reasons for Medicare to pay for her stay in the skilled nursing facility (SNF) while she was in hospice.
Does Medicare Pay For Skilled Nursing Care During Hospice?
Strictly speaking, Medicare does not pay for skilled nursing care because someone is in hospice, but other triggering events often cause Medicare to cover skilled nursing care.
For example, someone who is in hospice falls and breaks a hip. That situation would justify skilled nursing care. A person develops an infection or pneumonia that results in hospitalization. Then, they qualify for a skilled nursing stay.
How to Navigate the Medicare Coverage Process for Hospice in a Skilled Nursing Facility
 Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
Navigating the Medicare coverage process for hospice care in a SNF can be complex, but it can be made easier with the correct information and guidance. Here are some steps to help you navigate the process:
1. The first step is to consult with the individual’s physician to determine if they meet the eligibility criteria for hospice care in a SNF. The physician can provide the necessary certification and guidance through the process. He knows the triggering circumstances that justify a skilled nursing facility stay.
2. It’s important to choose a Medicare-approved hospice provider with experience providing SNF care. They will be able to guide you through the necessary paperwork and ensure that all requirements are met. The health professionals are very familiar with Medicare’s billing codes and protocols for admittance to a SNF.
3. If the individual is already receiving care in a SNF, it’s important to coordinate with the facility to ensure a smooth transition to hospice care. The SNF staff can provide valuable information and support during this process.
4. Familiarize yourself with Medicare’s costs and coverage for hospice care in a SNF. This will help you plan and make informed decisions regarding the individual’s care.
The professionals you deal with know the Medicare rules and the subtleties of maximizing coverage in different circumstances. Listen attentively to their guidance.
Common Misconceptions about Medicare Coverage of SNF During Hospice
Several common misconceptions exist about Medicare coverage for hospice care in a SNF. Let’s address some of these misconceptions and provide clarity:
provide clarity:
1. Medicare only covers hospice care in certain settings: Medicare provides coverage for hospice care in various settings, including inpatient hospice facilities, the patient’s home, and skilled nursing facilities. As long as the eligibility criteria are met, Medicare will cover hospice care in a SNF.
2. Medicare covers room and board in a SNF. As a rule, Medicare does not cover room and board in a SNF because the individual is receiving hospice care, though room and board may be covered because the patient is in the SNF for reasons other than hospice.
3. Medicare coverage for hospice care is limited to specific conditions: Medicare coverage for hospice care is not limited to specific conditions or illnesses. As long as the eligibility criteria are met, Medicare will provide coverage for hospice care in a SNF for any terminal illness.
4. Medicare coverage for hospice care is limited to a certain time frame: Medicare does not limit the duration of hospice care coverage in a SNF. As long as the individual meets the eligibility criteria, Medicare will continue to cover the necessary services.
Bottomline: Ensuring Quality Care and Coverage for Hospice in a SNF through Medicare
Maximizing Medicare coverage for hospice care in a skilled nursing facility is essential for ensuring quality end-of-life care. By understanding the eligibility criteria, coverage details, and navigating the Medicare system, you can advocate for yourself or your loved one and ensure all available resources are utilized.
Remember, hospice care is a compassionate and holistic approach that focuses on providing comfort and support during the final stages of a terminal illness. Medicare provides coverage for hospice care in a SNF, including room and board, medications, and necessary medical equipment. By staying informed and proactive, you can maximize Medicare coverage and ensure that the individual receives the care they need.
 Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Burying a mother is one of those milestone events in our lives. While dealing with all the emotional, spiritual, and financial challenges that accompanied that moment, health care cost was not a burden to my family and me. Medicare and my mother’s Medicare plan took excellent care of her and us. I am grateful for the wonderful program and the insurance that worked with Medicare.
Phyllis Grimmond 1935-2013 R.I.P.
The Bottomline: Benefit Knowledge Makes for Maximum Benefits
At Omaha Insurance Solutions, we understand the importance of access to accurate and reliable information regarding healthcare

Christopher J. Grimmond
decisions. We aim to empower you with the knowledge and resources to navigate the complex world of Medicare coverage. It is important to know that Medicare pays for hospice care in a skilled nursing facility.
By maximizing benefits and ensuring quality care, we can make a difference in the lives of individuals and their loved ones during this challenging time. Call us at 402-614-3389 to ensure you have a Medicare plan protecting you and your loved ones. Speak with an experienced licensed insurance agent profession.
What Are Skilled Nursing Facilities?

All of us have strong memories of visiting the “old folks’ home.” Whether grandparents, relatives, or friends, we recall the smells, linoleum, long hallways, and institutional dormitory rooms. “Old folks’ homes” or nursing homes fall under the category of Skilled Nursing Facilities (SNF). Medicare covers skilled nursing facilities within limits.
Patients go to the SNF after surgeries to recover, from illnesses to heal, and from injuries to recover and strengthen. Skilled Nursing Facilities are for temporary treatment, not long term residential care or custodial care, like memory care. Other facilities, like senior living communities, assisted living, or senior care centers describe other types of facilities that assist seniors.
A skilled nursing facility provides highly skilled professionals, such as occupational therapists, physical therapists, registered nurses, speech therapists. The advantage of an SNF is these professions are available 24 hours a day for the patients. The level of care is very high but short term.
Post-Acute & Skill Rehab Services
 Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Skilled Nursing Facilities are institutions that provide post-acute skilled nursing care and rehabilitation services. People sometimes confuse skilled nursing care with nursing home care because most of the time skill nursing usually takes place in a nursing home location. Medicare, however, doesn’t pay for “nursing home care”.
Medicare covers skilled nursing facilities within specific parameters. Nursing home care is for individuals who have reached a point in life when they can no longer perform activities of daily living. This is referred to as custodial care. In other words, they cannot bath, feed, and dress themselves. Medicare will not pay for those services to be provided exclusively.
Skilled Nursing is for after surgery or acute illness, for example, hip surgery for a fractured hip or a stroke. A skilled nursing facility admits patients for a short period of time after being in the hospital to aid in their healing and/or rehabilitation. Hospitals are incredibly expensive, and a skilled nursing facility can provide the necessary treatment at a lower cost.
Medicare Criteria For Skilled Nursing Facilities
The tricky part about skilled nursing facilities is admittance. A skilled nursing facility requires patients to meet certain essential criteria for admittance and for Medicare to pay. This is the complex checklist:
- The patient must be admitted to a hospital as an “inpatient” for at least three consecutive days, not including the day of dismissal. She can’t be in the
 hospital for “observation” for it to count for Medicare to pay.
hospital for “observation” for it to count for Medicare to pay. - Medicare mandates patient admittance to the skilled nursing facility within 30 days of discharge from the hospital. If problems arise later—past 30 days—the patient cannot go to the skilled nursing facility and have Medicare pay for it.
- Only a skilled nursing facility can provide the type of care necessary for the patient’s recovery. A skilled nursing facility would provide intense physical therapy for a hip injury or occupational therapy after a stroke. Going to the physical therapist’s office a couple of times a week would not be sufficient in those cases.
- A doctor, or appropriate medical professional, must certify that skilled nursing care is required for recovery.
- The patient must be treated for the same condition for which she was in the hospital.
There are nuances and exceptions to some of these rules. The list gives you a good idea about how skilled nursing fits into your Medicare health insurance. The Omaha, NE area has many quality Medicare certified facilities, and You can find them on the Medicare.gov website.
With all the information out there about Medicare Benefits, it’s easy to be confused, or even misinformed. It’s vital for those who are eligible for Medicare to understand the details about this long-standing, much needed program. The following are a few common Medicare misconceptions and the facts recipients need to set them straight.
Myth #1: Medicare Covers Everything
It is possible for Medicare recipients to piece together coverage that will imitate employer-sponsored health insurance, however there are differences in coverage depending on whether you have Medicare A, B, or D. For example, Part A pays for in-patient hospitalization or skilled nursing, but only after a deductible has been met, and only if the hospitalization requires staying for “two midnights.” Most people are automatically enrolled in Medicare Part B, which covers outpatient healthcare costs. Please see our previous blog post describing the features of each.
Myth #2: Medicare is Going Bankrupt
There have been significant concerns about this, especially with the progression of the ACA. The belief is that since more employees will retire than join the labor force in the coming decades while healthcare costs increase, the amount of money in the Hospital Insurance Trust Fund is expected to peak in 2019 and then drop from $204 billion to $124 billion by 2025. Rather than being Medicare’s undoing, however, healthcare experts believe that the change will be in how Medicare Part A pays for healthcare services, or in payroll taxes.
Myth #3: Medicare is Unnecessary
Medicare is expected to remain a critical program for retirees as baby boomers are living longer and the costs of healthcare continue to climb. Medicare is needed to protect the financial security of millions of senior citizens.
The Future
Regardless of what happens with Medicare, it’s essential that working individuals take the necessary steps to prepare a retirement plan with a savings target that considers their personal and family health history. It’s equally important to factor in the costs associated with Part B and Part D coverage, deductibles, and potential out-of-pocket healthcare expenses.
As we’ve mentioned previously, medical expenses can be astronomical. If the correct insurance is not in place with sufficient coverage, costs may surprise and overwhelm you. Not following the eligibility requirements could result in surprise penalties and permanent costs from Medicare. Call Omaha Insurance Solutions at 402-614-3389 or email us at [email protected] for a free consultation.
I learned to sing the alphabet before I learned to say it, and from that humble beginning, language opened up to me.
You can’t understand language without first understanding its alphabet. Medicare has a language, and Medicare has an alphabet. It begins with A, B, & D. They are the three essential components of Medicare.
A is for Medicare Part A. A covers the hospital 100% for 60 days but only after you pay a $1,260 deductible out of your pocket. Ouch! Part A is free because you paid for it during your working years. Eligibility for A is 3 months before your 65th birthday, the month of your birthday, & three months after. If you don’t enroll then, there will be a penalty.
B is for Medicare Part B. B covers doctor visits and outpatient procedures, such as, blood work, x-rays, emergency room, ambulatory surgeries, walkers, wheel chairs, oxygen tanks, etc. Part B does cost something. Currently $104.90 per month. Medicare Part B pays 80% of the costs. Your portion is 20%. Important fact about your 20% co-insurance is that there is no cap. As long as the bills roll in, your money rolls out. Bigger Ouch! The penalty for late enrollment for Part B is 10% for every 12 month period.
The final letter is not C. It’s D—D as in drugs. Medicare Part D was started in 2006 after people complained about the crushing cost of medications. Prescription drug plans are administered by private insurance companies approved by Medicare. Prescription Drug Plans (PDP) can range in cost from $20–$50 per month with deductibles and co-pays. There is a penalty for not enrolling in a Part D plan when you are eligible. It accrues each month you are not enrolled and is permanently added to your Medicare premium when you do enroll.
Medical expense can be astronomical. If the correct insurance is not in place with sufficient coverage, costs may surprise and overwhelm you. Not following the eligibility requirements could result in surprise penalties and permanent costs from Medicare. Call 402-614-3389 or email us at [email protected] for a free consultation to make sure all your letters are in place.
The Affordable Care Act (ACA) has brought many questions to business owners and individuals alike. What plan is the best? What kind of healthcare will you qualify for? Will you get to keep your same doctors? For those who are retired or close to retirement, the subject can be even more complicated. When you retire or turn 65, do you have to enroll in a Medicare Plan?
Essentially, yes. Joe Baker, president of the Medicare Rights Center, a national, nonprofit advocacy organization, warns that if you don’t enroll in Medicare at the age of 65, “you don’t have primary coverage, which means that you basically don’t have coverage for most of your healthcare needs.”
Many individuals are confused by this, perhaps rightfully so. The fact is, although your health insurance plan bought through an ACA marketplace will not automatically end when you turn 65, its coverage decreases dramatically. The message that Baker and other Medicare professionals are trying to get out to the public is that these individuals who are currently covered by the ACA before turning 65 must enroll in Medicare once they reach that age.
Now, it is important to realize that if you’re 65 or older and are covered by large-employer insurance, this rule doesn’t apply to you; however most people in this situation should at least take Part A, which is hospital insurance. Without this exception however, new Medicare enrollees must apply at least four months after they turn 65, otherwise they’ll have to wait until the next open-enrollment period, with no coverage in the meantime.
Timing is also important when switching from the ACA Marketplace to Medicare coverage; with individuals being warned to take care when they discontinue their exchange coverage as to not leave a gap between that coverage and Medicare enrollment.
The licensed insurance agents at Omaha Insurance Solutions are here to answer any of your questions you may have about Original Medicare, an Omaha Medicare Advantage Plan, and any other Medicare concerns you may have. Please contact us today at (855) 367-3631.
You can also find more information at Medicare.gov.
Sheep get sheared. They follow the other sheep into the pen, down the shoot, then in to the hands of the shearer and are fleeced. The ram is a alert. He doesn’t go with the flow he leads the way and butts heads when he is force to go where he doesn’t want to go.
How do people pick their Medicare supplement plan and company? They talk with their buddy on the left and their buddy on the right. ‘They both can’t be wrong.’ Everyone says Plan F is “the best.” “I never have to pay anything”—no co-pays. That’s great! Sign me up. That is the thought process of the sheep. Insurance companies love it. Insurance agents love it. Plan F is the most expensive plan in all kinds of way.
There are ten possible Medicare supplement plan types that an insurance may offer–A–N. In reality, they usually only offer 4 or 5. Plan F is the most popular as well as the most expensive. Insurance companies and agents like that because it brings in the most money and pays the highest commission. But is it the best for a client?
Plan F does cover all the deductibles and co-insurance that Medicare doesn’t cover. That is nice, but you pay a price for that convenience. It raises the question whether Plan F is the best.
Is there an alternative? How about Plan G? Plan G is very close to Plan F. The difference is that you pay the Part B deductible of $147. It is a one-time annual deductible. Once you pay your Part B deductible of $147, for let’s say a doctor’s visit, you are done for the year. Everything else will be covered 100% which is similar to a Plan F. So why plan G? Because the premium is lower—quite a bit.
Let’s do some simple math. Let’s say that a plan F is $150 per month for a 65 year old male and a plan G is $110 for the same person. The difference is $40 per month and $480 per year less for the Plan G. Subtract the $147 Part B deductible, and you are still ahead $333. Putting it another way, you are paying $333 for the convenience of having the insurance company pay your Part B deductible so that you don’t have to write a check IF you go to the doctor or have some other procedure. Multiply that times 10 years and you are at $3,330.
The second and more important consideration about Plan G is that the rate increases are smaller and less frequent. Yes premiums go up because medical costs go up, but the unusual reality about Plan G policy holders is that they generally do not go to the doctor or emergency room as frequently as Plan F policy holders. There is something about the $147 deductible that causes people to pause and think. ‘Is this really medically necessary?’ The result is that, because Plan G policy holders do not over use medical benefits to the extent Plan F policy holders do, the claims and cost are not has high. Consequently the rate increases for Plan G’s are fewer and smaller than Plan F. Plan F is the best?
Don’t be a sheep. Don’t follow the herd. Stop and look at the different plans. Ask yourself the hard question in light of the facts whether Plan F is the best. Do some analysis, and you will save money in the short, long, and longer run.
 402-614-3389; [email protected]
402-614-3389; [email protected]
 What Does Medicare Cover For Diabetics?
What Does Medicare Cover For Diabetics?
Diabetes is one of the fastest-growing medical conditions in America and can be one of the most costly conditions to treat. Diabetes costs for Medicare are important for Medicare beneficiaries to know.
According to the Center for Disease Control, there are currently 21.0 million Americans who have been diagnosed with at least one type of diabetes and millions more who have yet to be diagnosed. An additional 79 million people over age 20 living in the United States have blood sugar levels higher than usual but not high enough to be classified as pre-diabetic. With such dramatic numbers, it is no wonder that direct medical costs for diabetes treatment total over $176 billion each year. Nebraska and Iowa have their statistics. What Medicare covers for diabetics is critical for their sustained health and improvement.
What Does Diabetes Cost For Medicare?
Prevention and screening are high priorities for Medicare diabetes coverage. Medicare covers prevention programs and screening to detect pre-diabetic persons and high-risk individuals. Medicare can then more proactively treat and advise Medicare beneficiaries on how to avoid developing diabetes.
pre-diabetic persons and high-risk individuals. Medicare can then more proactively treat and advise Medicare beneficiaries on how to avoid developing diabetes.
For those with diabetes, Medicare covers insulin, anti-diabetic drugs, diabetes supplies, diabetes self-management training, nutritional therapy services, foot exams, blood testing mentors, and glaucoma exams.
Diabetes-related expenses can be a significant burden, especially for older Americans who rely on Medicare and government-funded healthcare systems. Unfortunately, Original Medicare (Medicare Part A and Part B only) will not cover diabetes costs 100% unless you have a Medicare supplement that may cover the remaining costs.
Not all Medicare Advantage Plans will completely cover testing or medications that help patients manage their diabetes, and even when coverage is extended, patients still face out-of-pocket expenses. Therefore, it is essential to read the Evidence of Coverage for your particular Medicare Advantage plan so that you understand Medicare diabetes prevention program billing and other services.
It is typical for Medicare Part B to cover blood glucose tests for diabetes screening, and two diabetes screenings each year for beneficiaries at high risk for diabetes, but drugs are not covered. As a result, patients are still often responsible for co-payments, office visit fees, and other expenses.
Part D Is the Achilles Heel of Medicare
 On the other hand, Medicare Part D will generally help some patients cover the supplies needed to control diabetes by helping patients pay for insulin and blood sugar monitoring equipment. However, in nearly all situations, diabetes costs for Medicare do not cover the full cost of these expenses unless the individual has a supplement or is on Medicaid. Insulin and anti-diabetic prescriptions are costly and can quickly drive patients into the Part D gap (donut hole).
On the other hand, Medicare Part D will generally help some patients cover the supplies needed to control diabetes by helping patients pay for insulin and blood sugar monitoring equipment. However, in nearly all situations, diabetes costs for Medicare do not cover the full cost of these expenses unless the individual has a supplement or is on Medicaid. Insulin and anti-diabetic prescriptions are costly and can quickly drive patients into the Part D gap (donut hole).
When prospective clients come to my office, my heart drops slightly when they say they are on insulin or the well-known expensive anti-diabetic prescriptions. I know how expensive these medications can be, especially on a limited and fixed income.
What Kind of Diabetic Costs for Medicare Are Included?
Diabetes wears the body down, and there are lots of side effects. Diabetes may cause nerve damage to your feet. Part B covers a foot exam every six months by a podiatrist. Medicare might cover even more visits if you had a non-traumatic amputation of all or part of your foot.
Your doctor may order Hemoglobin A1c tests to determine your blood sugar levels over the past three months. Medicare will cover diabetic services such as that when prescribed by your doctor.
Glaucoma is another adverse side effect of diabetes. Medicare Part B pays for eye exams for glaucoma once a year, especially if you have retinopathy or a family history of glaucoma.
These are all efforts to curb the negative effects of diabetes and maintain the highest possible quality of life.
What Are the Medicare Diabetes Prevention Programs?
“An ounce of prevention is worth a pound of cure,” we’ve always heard. 
The Medicare diabetes prevention programs begin with screenings. Diabetes screenings help detect early-stage or pre-diabetes in patients. Doctors can help their patients attack the causes when they can identify at-risk individuals. Medicare Part B covers diabetes screening tests when your physician prescribes a screening. Medicare may pay for as many as two diabetes screening tests in a 12-month period.
Symptoms like high blood pressure, a history of abnormal cholesterol and triglyceride levels, obesity, and impaired glucose tolerance, may indicate a higher likelihood of developing diabetes. Once identified, medical professionals can address the issue directly.
For those at risk, Medicare diabetes prevention programs may be in order. A once-per-lifetime behavior change program to help you prevent type 2 diabetes is covered by Part B. Medicare Advantage, which is Medicare delivered by a private insurance company, is highly motivated to keep its patients’ healthy. Diabetes is a costly disease, so Medicare Advantage plans are very generous with prevention services, especially diabetes. Read the Evidence of Coverage for your particular Medicare Advantage plan so that you understand Medicare diabetes prevention program billing and other services.
Prevention Program Criteria
 Medicare establishes specific criteria your doctor must follow before prescribing a Medicare diabetes prevention program. You must have:
Medicare establishes specific criteria your doctor must follow before prescribing a Medicare diabetes prevention program. You must have:
- Part B (or a Medicare Advantage Plan).
- A fasting plasma glucose of 110-125mg/dL, 2-hour plasma glucose of 140-199
mg/dL (oral glucose tolerance test), or a hemoglobin A1c test result between
5.7 and 6.4% within 12 months before attending the first core session. - A body mass index (BMI) of 25 or more (BMI of 23 or more if you’re Asian). No history of type 1 or type 2 diabetes.
- No End-Stage Renal Disease (ESRD).
- Never participated in the Medicare Diabetes Prevention Program.
To be eligible for the program. You may pay nothing if you are eligible.
The program consists of a weekly core session over a 6-month period with a peer group. The topics covered are changing behavior around diet and exercise, weight control, motivation, group support.
After completing the initial core session, you will have a six-month follow-up program with monthly sessions to help you maintain the healthy habits you established in the core program. After the 6 month follow-up, you may qualify for an additional 12 month ongoing maintenance program if you have met personal weight loss outcomes.
How Does Medicare Help You Self-Manage Your Diabetes?
Once someone has diabetes, their situation can be managed and even improved. Medicare offers self-management training to help you learn how to control your diabetes successfully. Diabetes self-management training requires a doctor’s prescription. Diabetes self-management training falls under Part B, which is Original Medicare.
Like any program, you need to meet the prerequisites.
- You were diagnosed with diabetes.
- You changed from taking no diabetes medication to taking diabetes
medication, or from oral diabetes medication to insulin. - You have been diagnosed with diabetes and are at risk for complications.
Further, your primary care physician considers you at increased risk because of one or more of these conditions:
- Problems controlling blood sugar, have been treated in an
emergency room, or have stayed overnight in a hospital because of your
diabetes. - Diagnosed with eye disease related to diabetes.
- Lack of feeling in your feet or some other foot problems, like ulcers,
deformities, or have had an amputation. - Diagnosed with kidney disease related to diabetes.
Like most Medicare-covered services, the training program must be Medicare-certified and accredited by the American Diabetes Association or the American Association of Diabetes Educators.
Special Individual Training
The program is taught by specially trained healthcare professionals with a thorough knowledge of diabetes. Medicare covers up to 10 hours of initial training and 2 hours of follow-up training if necessary. They must complete the program within 12 months once it has begun.
The diabetes self-management training will cover:
- General information about diabetes, the benefits of blood sugar control, and poor blood sugar control risks.
- Nutrition and how to manage your diet.
- Options to manage and improve blood sugar control.
- Exercise and why it’s vital to your health
- Taking medications properly
- Blood sugar testing
- Foot, skin, and dental care.
Does Medicare pay for Diabetic Supplies?
Medicare Part B covers “durable medical equipment.” This category covers everything from CPAP machines to electric scooters. Diabetic supplies, like monitors, test strips, and lancets, fall under durable medicare equipment. Durable medical equipment even includes disposable items. Medicare covers diabetic supplies.
supplies, like monitors, test strips, and lancets, fall under durable medicare equipment. Durable medical equipment even includes disposable items. Medicare covers diabetic supplies.
With advances in diabetic technology, Medicare coverage of diabetes supplies includes new devices, like therapeutic continuous glucose monitors. The doctor, however, needs to make a case for you that a newer, more expensive device is medically necessary. In many cases, approval hinges on the doctor’s office making a case for the prescription. The prescription notes need to explain to Medicare or the insurer why the treatment would be beneficial to the health of the patient. In diabetes, especially, the insurance company and Medicare are trying to avoid more costly treatments that may result from further deterioration due to the illness. Even applying after a denial would be good. Sometimes it just takes a little more effort to get the best result.
So what diabetic testing supplies are over by Medicare?
Diabetes Test Strips Are Expensive!
 I have learned a lot about diabetes over the years from my clients. They tell me in unambiguous and sometimes loud terms the cost of things like test strips. Syringes, insulin pens, needles, alcohol swabs, gauze, inhaled insulin devices, test strips are all covered. The issue is not usually coverage but cost. Depending on your supplement or Medicare Advantage plan, your supplies may be nothing to very little. That is why it is critical to know how your Medicare plan affects those particular areas and costs for your health.
I have learned a lot about diabetes over the years from my clients. They tell me in unambiguous and sometimes loud terms the cost of things like test strips. Syringes, insulin pens, needles, alcohol swabs, gauze, inhaled insulin devices, test strips are all covered. The issue is not usually coverage but cost. Depending on your supplement or Medicare Advantage plan, your supplies may be nothing to very little. That is why it is critical to know how your Medicare plan affects those particular areas and costs for your health.
Does Medicare Cover An Insulin Pump?
I am always delighted when someone tells me they use an insulin pump. I am happy for them because the insulin that goes with the insulin pump does not come under Medicare Part D. The insulin for the pump comes under Part B. Those clients with Original Medicare and a Medicare Supplement (Medigap) policy will pay little or nothing for their insulin. Insulin can be incredibly expensive.
Part B covers insulin pumps worn outside the body (external), including the insulin used with the pump. Insulin pumps are considered durable medical equipment. With a Medigap plan, the patient will pay little or nothing for the pump and insulin. Medicare covers insulin pumps and supplies. The insulin that goes with the pump is considered supplies. This is all contained in the Medicare insulin pump guidelines.
 Medicare Covered Therapeutic Shoes Or Inserts for Diabetics
Medicare Covered Therapeutic Shoes Or Inserts for Diabetics
If you have Part B, have diabetes, and meet certain conditions, Medicare will cover therapeutic shoes if you need them.
The types of shoes Part B covers each year include one of these:
• One pair of depth-inlay shoes and 3 pairs of inserts
• One pair of custom-molded shoes (including inserts) if you can’t wear depth-inlay shoes because of a foot deformity, and 2 additional pairs of inserts
Doctor Certification for Therapeutic Shoes
For Medicare to pay for your therapeutic shoes, the doctor treating your diabetes
must certify that you meet these 3 conditions:
1. You have diabetes.
2. You have at least one of these conditions in one or both feet:
• Partial or complete foot amputation
• Past foot ulcers
• Calluses that could lead to foot ulcers
• Nerve damage because of diabetes with signs of problems with calluses
• Poor circulation
• A deformed foot
3. You’re being treated under a comprehensive diabetes care plan and need
therapeutic shoes and/or inserts because of diabetes.
Medicare also requires:
• A podiatrist or other qualified health care provider prescribes the shoes.
• A doctor or other qualified individuals like a podiatrist, orthopedist, or prosthetist fit and provide the shoes.
Are Medicare Diabetes Mail Order Suppliers Covered?
You can receive your diabetic supplies and medications through the mail. It is essential that the Medicare diabetes mail-order supplier be Medicare-certified and/or contracted with the Medicare Advantage plan. Insulin and anti-diabetic medications will usually come under Part D. The prescription drugs can be delivered by a stand-alone Part D plan or a Part C Medicare Advantage plan that includes prescription drug coverage. Prescription drug costs will be substantially different than those costs that fall under Part B. Check and confirm that company’s status before ordering, but mail-order is definitely an option.
Do Medicare Supplements Cover Diabetes?
The above discussion of Medicare coverage for diabetes has been reserved mostly to just Original Medicare (Part A and Part B). Medicare Supplements and Medicare Advantage add additional coverage but also another wrinkle to what is covered.
Medicare Supplements (Medigap) policies are simple because they are universal–the same everywhere. Plan G and Plan N are the most popular Medigap policies. Medigap covers whatever Medicare covers. They fill in the gaps in Original Medicare coverage. Under Part B, they take care of the insulin pump, and insulin for the pump, and durable medical equipment. Minus the Part B deductible, the Medigap policy almost completely covers any cost.
What Does Medicare Part C – Medicare Advantage Do For Diabetes?
Medicare Advantage plans all differ. Coverage varies from plan to plan and region to region. Reading the Evidence of Coverage that each plan has for the details of the plan is essential to find out how much is covered or not covered for things like orthopedic shoes, insulin pumps, diabetic supplies. I could describe the plans in the Omaha Metro area, but that may not apply to other areas.
 What Does Medicare Drug Coverage Pay for Diabetic Prescriptions?
What Does Medicare Drug Coverage Pay for Diabetic Prescriptions?
Medicare drug coverage is very similar between stand-alone Part D and Medicare Part C plans that include drug coverage. Insulin and anti-diabetic medications are mostly very expensive unless you have EXTRA HELP. Depending on the amount and type of medication, the patient can easily be driven into the coverage gap (donut hole) and even to the catastrophic stage because of the cost. It hurts my heart when I am adding up all the medications knowing that the picture is not going to be pretty when meeting with a diabetic client. I’ve witnessed a lot of tears and fear because of the sometimes staggering drug costs.
You Need To Know Your Prices
Medicare coverage of diabetes and diabetics is comprehensive. The real question is the shared costs that beneficiaries pay out of pocket. Medicare supplies are limited. Prevention costs are very small if non-existent. The real challenge, even now after the Trump administration initiatives, is the cost of insulin and anti-diabetic medications.
For my clients who are on any expensive medications, I highly, highly encourage them to be in contact with me during the Annual Election Period (AEP) October 15th–December 7th when they can change their Part D prescription drug plan or Medicare Part C plan. Even if your medications do not change, the plan can change. You could go from paying very little for a medication to not being covered at all. An annual review is critical for those with high-end medications.
Talking with a licensed, knowledgeable, experienced insurance professional you trust is critical to get the correction information and prices to make informed decisions about your Medicare health coverage.
Like most children, I learned to sing the alphabet before I learned to read it. From that humble beginning, language opened up to me. Why does that matter when we’re talking about Medicare? You can’t understand language without first understanding the alphabet. Medicare has a language and an alphabet all its own.
Medicare Part A is the first letter in the alphabet and language of Medicare. A isn’t for apple, however. Part A is for hospital insurance, so how much is Medicare Part A deductible for 2021?
First, we let’s discuss what Part A is and what it covers.
What Is Medicare Part A?
Medicare Part A covers four areas of care: inpatient hospital stays, skilled nursing facility stays, home healthcare, and hospice.
Inpatient hospital covers, as you might expect, when patients go to the hospital. Patients can go to the hospital for treatment, they may even stay overnight, but they may not necessarily have been admitted as an inpatient. Inpatient hospital is its own category, billing codes, and Medicare costs. A patient is generally not admitted for an inpatient hospital stay unless the condition is serious enough to warrant at least a two-day hospital stay.
Observation in the hospital is not admittance. You are under hospital observation, but you are not an inpatient. Medicare Part A deductible will not cover observation in 2021, and most Medicare Advantage plans (MA plans) will not cover hospital observation, either. However, some MA plans are starting to.
Check your MA plan’s evidence of coverage before proceeding. Note that a doctor must sign an order for a medically necessary service in the hospital for a person to be admitted as an inpatient.
What Is The Medicare Part A Deductible in 2021?

Chris was very patient. He educated me on Medicare and gave me choices. He took care of everything and made Medicare simple and easy.
Part A hospital insurance covers everything during the hospital stay–except doctor’s visits– completely for 60 days, but only after you pay a $1,484 Medicare deductible out of your pocket in 2021, assuming you have no other health insurance coverage.
Medicare Part A does not have a premium. The 1.45% FICA taxes you paid for Medicare during your working years covers your Part A cost. There is only a deductible, no co-insurance.
This applies to each 60 days per event benefit period. Note, that it is possible to have multiple unrelated events overlapping within a 60 day period. In that case, you’d pay multiple deductibles. Ouch!
What Is The Medicare Part A Benefit Period?
The Part A benefit period begins the day of admittance and ends when the treatment stops. A new benefit period does not start until you are without inpatient treatment for 60 consecutive days.
If you are readmitted to the hospital within the 60 days following, the countdown starts again where you left off until you use 60 days.
 Medicare Part A Coinsurance Payments Are Covered By?
Medicare Part A Coinsurance Payments Are Covered By?
Once you exceed the first 60 days, you have a co-insurance of $371 per day from day 61-90. Medicare coinsurance is different from Medicare deductible in 2021. Again, this is assuming you have no Medigap policy or other health insurance.
Paying the Part A co-insurance amount is rare because most hospital stays end well before the 61st day.
Medicare Deductibles Affect Insurance Costs
It is important to note for those on Medigap policies or even Medicare Advantage that Medicare deductibles impact insurance costs. This extended coverage is the obligation of your Medigap policy or MA plan. Consequently, the insurance company actuaries must factor in the probability of occurrence and cost.
The cost is transferred to the price of the Medigap plan or co-pays on the MA plan. Many clients wonder why their Medigap plan premium is going up? There are many factors, but when Medicare lowers the amount it will cover, the insurance companies pass on the cost to the consumer.
 What Are Lifetime Medicare Reserve Days?
What Are Lifetime Medicare Reserve Days?
Medicare lifetime reserve days refers to the 60 days a Medicare beneficiary may use once they exhaust the first 60 days of Part A and the additional 30 days with the $371 co-insurance.
The patient dips into the lifetime reserve days Medicare provides. These days, however, are not free. The coinsurance is $742 per day. Once these 60 lifetime reserve days are exhausted, the patient assumes all costs in the hospital, assuming there is no other insurance.
What Does Part A Cover Besides Hospital?
In 2021 once you have paid the Medicare deductible, Medicare Part A covers hospital stays virtually completely: semi-private room, general nursing, drugs prescribed while in the hospital, supplies, and treatments while an inpatient. The various areas within the hospital are also covered life ICU (intensive care units), inpatient rehabilitation, inpatient psychiatric facilities, long-term care hospitals.
Does Part A Cover Skilled Nursing Care?
Most people understand Part A is for the hospital. On the Medicare card itself, the card says “Part A Hospital.” However, many people don’t realize skilled nursing care falls under Part A, as well. The rules of coverage and payment are very similar to the inpatient hospital stays. I discuss skilled nursing in another blog.
Is Home Health Care Covered Under Medicare Part A or Part B?
Home Health Care can fall under Part A. Many people assume it is exclusively under Part B, but there are circumstances when Part A may pay for home health care.
Generally, beneficiaries and doctors approach home health care from the Part B side of Medicare to avoid the high Medicare Part A deductible and the more restrictive rules of hospital confinement.
 What is the Medicare Deductible For Hospice 2021?
What is the Medicare Deductible For Hospice 2021?
Part A covers hospice completely with no deductible. Hospice includes hospice nurses, medications, and counseling. Medicare Advantage plans actually do not cover hospice, rather the beneficiary reverts back to Original Medicare, at least for the hospice care. The Medigap policy likewise does not cover the cost. Medicare picks up the entire tab.
That being said, there is some confusion about what hospice covers. I had a client’s family member call to cancel her mother’s supplement. Someone in hospice told her because hospice was paying for everything, she could save money by canceling the Medigap policy. But hospice will not cover things like your primary care physician visiting you, a special hospital bed, or other medical treatments that are not life-sustaining but you might prefer.
Those services fall under Original Medicare and your supplement or your Medicare Advantage plan. For the short time someone is on hospice, I would focus on them rather than a few dollars.
Medicare Part A Deductible Conclusion

I have discussed Medicare Part A as Part A without a supplement or referring to Medicare Advantage. Many Medicare beneficiaries have only Medicare Part A or Part A with Part B. They do not have a supplement, advantage plan, or other insurance. So this speaks to them.
However, to understand Part A and how it fits within the bigger picture of Medicare health insurance, it is important to understand what it is, what it covers, and what it costs in its various iterations.
If this is confusing–and I don’t blame you for feeling that way–give us a call. Medical expenses can be astronomical. If the correct insurance is not in place with sufficient coverage, costs may surprise and overwhelm you. Not following the eligibility requirements could result in surprise penalties and permanent premium hikes from Medicare.
Call 402-614-3389 or email [email protected] for a free consultation to make sure all letters of your Medicare alphabet are in place.









