Medicare Advantage PlansCategory:
 Are you considering enrolling in a Medicare Advantage plan? Before making a decision, it’s crucial to understand the coverage options and potential limitations. One common concern is whether Medicare Advantage plans can deny coverage because they require prior authorization.
Are you considering enrolling in a Medicare Advantage plan? Before making a decision, it’s crucial to understand the coverage options and potential limitations. One common concern is whether Medicare Advantage plans can deny coverage because they require prior authorization.
Medicare Advantage plans, or Medicare Part C, are offered by private insurance companies approved by Medicare. These plans provide all the benefits of Original Medicare (Parts A and B) and often include additional benefits such as prescription drug coverage and dental, vision, and hearing services.
We will delve into the specific circumstances in which a Medicare Advantage plan requires prior authorization and could potentially deny coverage, the appeals process for denied claims, and what steps you can take to ensure you receive the coverage you need. By understanding the ins and outs of Medicare Advantage plans, you can make an informed decision about your healthcare coverage. So, let’s unlock the truth together and navigate the world of Medicare Advantage plan prior authorization.
What is the Purpose of Prior Authorization?
Prior authorization (or Pre-Authorization) is a utilization management tool used to contain costs. It consists of a third party, usually employed by the insurance company, making determinations about a request for service. The third party, who may be a doctor, nurse, or non-medical staff, approves or denies a request based upon predetermined criteria.
• Is the service covered?
• Is it a duplicate?
• Does the request contain the proper codes and supporting documentation?
• Is the service “medically necessary” as defined by CMS’s standard of care?
The purpose of Medicare Advantage plans requiring prior authorization is to ensure that the medical procedures are necessary and that the payer (insurance company) and patient are not wasting money.
Health care involves a great deal of money. There are three primary interested parties: the patient, who wants to pay as little as possible, the doctor, who provides a service for a fee, and the insurance company, which protects the patient from overwhelming healthcare costs for a premium.
Each has different and conflicting interests. Each is making a cost-benefit analysis to determine if the activity is worth it.
The patient wants good care for minimal cost. The doctor wants to be paid as much as possible for skills and services rendered. The insurance company wants to provide protection at the lowest cost to itself to maximize profit. Each is attempting to protect its interests. The insurance company uses prior authorization to make sure the service is, in fact, medically necessary so it does not waste money on unnecessary services.
The tradeoff is that prior authorization creates a barrier that potentially delays care and adds to its cost. There is also the potential that needed healthcare is wrongly delayed or withheld.
Medicare Advantage Utilizes Prior Authorization
Like commercial health insurance your employer purchases for employees, Medicare Advantage requires prior authorization for a majority of procedures, tests, and treatments, especially the more costly treatments. If approval is not granted, the insurer does not pay. There is an appeal process; however, many do not utilize the appeal process.
Traditional Medicare does not employ utilization management tools like prior authorization except in a few instances. The lack of any supervision of the medical necessity of services and payments has resulted in some high-profile cases of fraud, waste, and abuse. The only mechanism to combat abuse is self-reporting, whistle blowers, and fraud hotlines.
Optimally, prior authorization deters patients from getting care that is not truly medically necessary, reducing costs for both insurers and enrollees. Prior authorization requirements, however, can also create hurdles and hassles for beneficiaries and their physicians and may limit access to both necessary as well as unnecessary care. It also adds the burden of expense to providers who pay staff to work with insurance companies through the prior authorization process.
Data suggests that Medicare Advantage members save an average of $1,965 per year in total health expenditures compared to fee-for-service Traditional Medicare. Medicare Advantage members have lower hospitalization rates and fewer readmissions than their Traditional Medicare counterparts.
Does Original Medicare Utilize Prior Authorization?
From its inception, Traditional Medicare (Original Medicare) has not used prior authorization. There was little, if any, oversight until the electric wheelchair scandal.
A Washington Post article published in August 2014 highlighted the massive fraud of Medicare’s resources. The article chronicled the sensational scams and trials of many Medicare swindlers. The outrageous theft of public funds and the massive fraud shamed CMS to amend its regulations to finally require pre-authorization for some “durable medical equipment,” i.e., electric wheelchairs.
Bureaucrats inside CMS admitted they knew how the wheelchair scheme worked as early as 1998. However, it was not until 15 years later that officials finally did enough to curb the practice significantly. Durable medical equipment—electric wheelchairs—is the only exception to the “reasonable and necessary” practice. They must be preapproved.
The Government Accountability Office (GAO) examined a prior authorization program that CMS ran in seven states in 20212. During the short duration of the program, Medicare saved $1.9 billion. The GAO recommended that CMS continue to study the subject and implement a prior authorization program for all of Original Medicare in its 2018 published study. CMS discontinued the program.
 The Effect of Medicare Advantage Denials
The Effect of Medicare Advantage Denials
There may be severe consequences when a Medicare Advantage Organization (MAO) denies authorization for a procedure.
- Patient access to medical care is delayed or denied.
- Potentially, it results in the patient paying out of pocket for something Medicare should have covered.
- It causes an administrative burden for the patient and providers because they must devote resources to an appeal.
None of these have positive consequences and are a cause of frustration with Medicare Advantage for some.
How Common is Medicare Advantage Prior Authorization Denials?
The Kaiser Foundation examined CMS data from MAOs from 2021. They found that more than 35 million prior authorizations were submitted to Medicare Advantage insurers. Over 2 million prior authorization requests were fully or partially denied by the insurance companies.
The percentage of prior authorization requests and denials depends upon individual plans. They are not identical. Of the 2 million denials, some were partial denials, totaling 380,000.
Partial denials would be, for example, physical therapy sessions. The physician requests 10 sessions, but only 5 are granted. That leaves 1.6 million prior authorizations completely denied. The average for Medicare Advantage plans as a whole was less than 6 percent, with individual MAO falling slightly above or below that average.
How About Appeals of Prior Authorization Denials?
Each Medicare Advantage plan has an appeal process. Data from the same group revealed that only 11 percent (or 212,000) of appeals were made, including partially and fully denied requests. The insurance companies overturned 82 percent (or 173,000) of the appeals.
insurance companies overturned 82 percent (or 173,000) of the appeals.
The high number of repeals was cause for concern. Are Medicare beneficiaries being unjustly denied services? Are the insurance companies creating unfair obstacles to reduce costs?
The study’s data, however, do not describe in detail the causes of the denials. In general conversations with insurance carriers, the authors discovered that prior authorizations are denied for a number of common reasons.
- Incorrect coding and insufficient documentation
- Less intrusive or costly services were not first tried.
- The provider was not in the network
- Service is not covered
- Human error
All of these reasons may result in a denial of service, but the data does not identify the various causes, some of which are easily rectified upon review or appeal.
We have thousands of clients who call us when there are issues. I am amazed at how often the provider’s back office does not file the proper paperwork, use the correct codes, or include essential documentation such as X-rays or tests.
Then, when the pre-authorization is denied, the insurance company is blamed, and the subject is dropped. The back office is understaffed, doesn’t have the time, and doesn’t sufficiently understand the insurance company’s processes, so they cut their losses and move on to other cases. Sometimes, the provider moves on to the less costly treatment, knowing that it will be immediately approved.
How Many Are Denied Coverage Unnecessarily?
The Office of Inspector General (OIG) for the Department of Health & Human Services published a report in April 2022 regarding the denial of medically necessary services by some Medicare Advantage Organizations (MAO). The study discovered that MAOs denied services to Medicare beneficiaries on some MAO plans even though the prior authorization request did meet the standard for Medicare coverage rules.
The OIG study sample was taken from 15 of the largest MAOs during the week of June 1-7, 2019. The sample size was 500—250 prior authorizations and 250 denials of claims. Eventually, the number was reduced to 430 as the data was further sifted.
The OIG dug into the details of each of the 430 cases. In the course of the review of the cases, OIG found a conflict in the standards.
Conflict in Standards
CMS has its own guidance regarding the standard of care. The MAOs, however, have developed their own internal clinical criteria that go beyond Medicare coverage rules even though the case would pass CMS’s standards. In the past, CMS has left the MAOs to develop their own criteria where CMS is unclear. For example, a less intrusive or costly treatment may be required before a more expensive service is authorized by the MAO. Physical therapy may be more appropriate first before an MRI is prescribed.
Second, MAOs indicated that some prior authorization requests did not have enough documentation to support approval, yet OIG reviewers found that the existing beneficiary medical records were sufficient to support the medical necessity of the services.
On payment requests, the OIG found that the MAOs denied 18 percent of the cases that would have met the Medicare coverage and MAO billing rules. Most of these payment denials in the sample were caused by human error during manual claims processing reviews (e.g., overlooking a document) and system processing errors (e.g., the MAO’s system was not programmed or updated correctly).
In the end, OIG determined that 13 percent of the 250 prior authorization cases studied should not have been denied based upon CMS stands (or approximately 32 individuals).
How Many Denied Coverage Should Be Approved?
If we combine the two studies, Kaiser Foundation and Office of Inspector General for the Department of Health & Humana Services—we actually get an idea of who should have been approved.
The Kaiser Foundation consists of 35 million prior authorizations, with less than 2 million being denied, which is a 5 percent denial rate.
The OIG’s study discovered that only 13 percent of those denied should have been approved.
So, when we apply the average of 13% of wrongly denied prior authorization requests to the 2 million denials in the Kaiser study, that is approximately 260,000 individuals who should have been approved but were not out of 36 million prior authorization requests.
That means out of 36 million prior authorization requests, only 0.7 percent were wrongly denied coverage. In other words, 99.3 percent of prior authorizations are processed correctly.
I find that an incredibly high degree of accuracy.
Appeals and Reconsiderations for Denied Coverage
The appeals process for denied coverage with Medicare Advantage plans involves several levels, each with its own deadlines and requirements. Understanding these steps can help you navigate the process effectively and increase your chances of a successful appeal.
Redetermination
The first level of appeal is the “Redetermination” process. You must submit a written request to your Medicare Advantage plan within a specified timeframe, usually 60 days from the date of the denial letter. Include all relevant documentation and explain why you believe the service or procedure should be covered. The plan must review your appeal and provide a written decision within 30 days.
Reconsideration
If your appeal is denied at the redetermination level, you can proceed to the second level, known as a “Reconsideration.” This involves submitting a request to an independent review entity contracted by Medicare within 60 days of receiving the redetermination denial. The review entity will conduct a thorough review of your case, including any additional evidence you provide, and issue a written decision within 60 days.
Administrative Law Judge
If your appeal is still denied at the reconsideration level, you have the option to request a hearing before an administrative law judge (ALJ). This request must be made within 60 days of receiving the reconsideration denial. The ALJ will hold a hearing, either in person or by video conference, where you can present your case. The ALJ will issue a written decision within 90 days.
Medicare Appeals Council
If you are dissatisfied with the ALJ’s decision, you can further appeal to the Medicare Appeals Council. This request must be made within 60 days of receiving the ALJ’s decision. The council will review your case and issue a written decision.
Federal District Court
The final level of appeal is to seek judicial review in a federal district court. This step involves filing a lawsuit against the Medicare Advantage plan in a federal court. It’s important to consult with legal counsel if you reach this stage, as the process can be complex.
Bottom Line: Medicare Advantage Prior Authorization Is a Required Tool
No one writes a blank check. When money is being spent, there is oversight. When there is a lot of money from a lot of people, there will be a lot of accountability. The Medicare Advantage oversees that taxpayers’ and beneficiaries’ money is spent in accordance with the norms and procedures that CMS has laid down. Medicare Advantage requires prior authorization to protect resources and clients, but like any institution that is carrying out millions of actions among thousands of people, there are errors. The appeals process is supposed to remedy those errors, but in an imperfect world, not always.
clients, but like any institution that is carrying out millions of actions among thousands of people, there are errors. The appeals process is supposed to remedy those errors, but in an imperfect world, not always.
Currently, no one has complete and adequate data to give an accurate idea of inappropriate Medicare Advantage denials, but the data and studies recently done show that the level of error is incredibly low.
 Are you feeling lost and confused about Medicare Advantage prior authorization? You’re not alone. Navigating the healthcare system can be overwhelming, especially regarding insurance processes. But fear not—we are here to demystify it all for you.
Are you feeling lost and confused about Medicare Advantage prior authorization? You’re not alone. Navigating the healthcare system can be overwhelming, especially regarding insurance processes. But fear not—we are here to demystify it all for you.
This comprehensive guide will delve into everything you need to know about Medicare Advantage prior authorization. From understanding what it is, why it’s necessary to learn how it works, and the steps involved, we’ll break it down in simple terms. There will be no jargon, no confusing terms—just clear and concise information.
What is Prior Authorization?
Prior authorization is a process used by insurance companies to determine whether they will cover a specific medical procedure, treatment, or prescription drug. It is required for certain services to ensure that they are medically necessary and cost-effective.
Why is Prior Authorization Necessary?
Prior authorization prevents unnecessary medical procedures, reduces healthcare costs, and ensures patients receive appropriate care. Insurance companies can control expenses and ensure that resources are allocated efficiently by reviewing and approving or denying requests for certain healthcare services.
Problems With Medicare Advantage Prior Authorization
However, prior authorization can be complex and time-consuming. It requires healthcare providers to submit detailed information about the patient’s condition, medical history, and proposed treatment plan. The insurance company then reviews this information to determine whether the requested service meets its coverage criteria.
While prior authorization can be beneficial in some cases, it can also lead to delays in care and administrative burdens for both healthcare providers and patients. There are many elements, moving parts, and hands that touch a prior authorization request. Thus, the process is ripe for mistakes, misunderstandings, and delays. Understanding the process and requirements can help you navigate this system more effectively.
Prior Authorization Process for Medicare Advantage
Obtaining prior authorization for Medicare Advantage plans involves several steps. Here’s a breakdown of the process.
Consultation with Healthcare Provider
The first step is to consult with your healthcare provider. They will determine if the service or treatment you need requires prior authorization and initiate the process on your behalf.
Submission of Prior Authorization Request
Once your healthcare provider has determined that prior authorization is necessary, they will submit a request to your insurance company. This request includes all the necessary documentation, such as medical records, test results, and treatment plans. This is where I see problems arise. The doctor’s back office uses incorrect codes, forgets test results, and the doctor’s notes are missing essential language. Then, the request is denied.
Review by the Insurance Company
The insurance company will review the submitted request and evaluate the medical necessity of the service requested. It may also consider factors such as cost-effectiveness and alternative treatment options.
 Approval or Denial
Approval or Denial
The insurance company will either approve or deny the prior authorization request based on their evaluation. If approved, you can proceed with the recommended treatment. If denied, you have the option to appeal the decision. The additional problem is the insurance company does not give a reason for the denial, so the provider is clueless about where to begin. The carrier is not required to give a reason, so the provider needs to commit more resources to find out what is needed or let it go.
Appeals Process
You can appeal the decision if your prior authorization request is denied. This involves providing additional documentation or evidence to support the medical necessity of the requested service. The insurance company will review your appeal and make a final determination.
necessity of the requested service. The insurance company will review your appeal and make a final determination.
It’s important to note that the prior authorization process may vary slightly depending on your specific Medicare Advantage plan and the services you need. For detailed information about the process, consult with your healthcare provider, insurance company, and Center for Medicare & Medicaid Services (CMS).
Standard Medicare Procedures & Services Requiring Prior Authorization
 Prior authorization is typically required for certain medical procedures, treatments, and prescription drugs. While the specific requirements may vary depending on your Medicare Advantage plan, here are some standard procedures and services that often require prior authorization.
Prior authorization is typically required for certain medical procedures, treatments, and prescription drugs. While the specific requirements may vary depending on your Medicare Advantage plan, here are some standard procedures and services that often require prior authorization.
Specialized Surgeries
Complex surgical procedures, such as organ transplants or bariatric surgery, often require prior authorization. This ensures that the procedure is medically necessary and appropriate for the patient’s condition.
High-Cost Medications
Certain prescription drugs, especially those with high costs, may require prior authorization. This helps insurance companies manage expenses and ensure patients receive appropriate medications.
Imaging Tests
Advanced imaging tests like MRI or CT scans may require prior authorization. This ensures that these tests are necessary and will provide valuable information for diagnosis or treatment.
Physical Therapy or Rehabilitation Services
Medicare Advantage plans often require prior authorization for physical therapy, occupational therapy, or other rehabilitation services. This helps ensure that these services are appropriate and will contribute to the patient’s recovery.
I have found that skilled nursing facility care is very difficult to get approved, especially if the stay exceeds the initial twenty days. The impasse is a combination of the skilled nursing facilities (SNF) refusing to submit for a patient with a Medicare Advantage plan. Many SNFs will not even consider submissions for stays beyond twenty days. Some seem to not know how to properly submit a reauthorization or claim. From the insurance company’s side, their restrictions seem overly prohibitive. This has been a huge source of complaints to CMS and Congress.
 Durable Medical Equipment
Durable Medical Equipment
Equipment such as wheelchairs, oxygen tanks, or home healthcare supplies may require prior authorization. This ensures that the items are medically necessary and will improve the patient’s quality of life. CMS has a significant history of fraud, waste, and abuse regarding durable medical equipment.
It’s important to check with your specific Medicare Advantage plan to understand which procedures and services require prior authorization. Your healthcare provider can also provide guidance based on your individual needs.
Benefits of Medicare Advantage Prior Authorization
While the prior authorization process can be perceived as burdensome, it offers some benefits for patients and insurance companies. Here are a few advantages of Medicare Advantage prior authorization:
- Cost control: Prior authorization helps insurance companies control healthcare costs by ensuring that services are medically necessary and cost-effective. This helps keep premiums affordable for all members.
- Appropriate care: Prior authorization ensures that patients receive appropriate care by evaluating the medical necessity of requested services. This helps prevent unnecessary procedures or treatments that may not be beneficial.
- Improved outcomes: By reviewing and approving requests for certain healthcare services, insurance companies can help ensure that patients receive the most effective and evidence-based treatments. This can lead to improved health outcomes and better quality of life.
- Resource allocation: Prior authorization helps allocate healthcare resources efficiently by ensuring that they are used for the most appropriate and effective services. This helps prevent overutilization of healthcare services and ensures that resources are available for those who need them.
While there are benefits to prior authorization, it’s important to acknowledge the challenges and drawbacks of the process as well.
Challenges & Drawbacks of the Medicare Prior Authorization Process
While prior authorization serves a purpose in the healthcare system, it has its challenges and drawbacks. Here are some common challenges that patients and healthcare providers may encounter.
Prior Authorization Administrative Burden
The prior authorization process can be time-consuming and requires healthcare providers to gather and submit extensive documentation. This administrative burden can take away valuable time that could be spent on patient care.
Dr. Jesse M. Ehrenfeld, M.D., president of the AMA (American Medical Association), says,
The need to right-size prior authorization has never been greater—mountains of administrative busywork, hours of phone calls, other clerical tasks that are tied to this onerous review process. It not only robs physicians of face time with patients, but studies show that it contributes to physician dissatisfaction and burnout.
Delayed Care
Prior authorization can sometimes lead to delays in care, as the review process may take time. This can be frustrating for patients who need immediate treatment or services.
Starting in 2026, CMS is shortening the time frames for prior authorization decisions. Insurance payers must respond within 72 hours for an expedited or urgent request and seven calendar days (not business days) for a standard request.
 Denial of Coverage
Denial of Coverage
There is always a risk of prior authorization requests being denied. This can be disappointing for patients hoping to receive a particular treatment or procedure.
Lack of Transparency
Insurance companies may have different criteria and guidelines for prior authorization, leading to confusion and lack of transparency. Patients and healthcare providers may struggle to understand the reasons for a denial or how to navigate the process effectively.
Dr. Jesse M. Ehrenfeld, M.D. describes the problem of the lack of transparency with the insurance companies.
When a request is denied, we often don’t know why. We don’t tell you the reasoning behind the denial. It can take hours and hours to appeal a decision. And then sometimes you wait weeks or even months for a peer-to-peer consult.
The CMS final rule will require insurers to provide specific, very specific denial reasons and public reporting of metrics. How often do they approve? How often do they deny things? How long does it take for a process to actually give a result for a request?
Insurers will also be required to share that information with patients, so that our patients can become informed decision makers when they buy health insurance on the exchanges and make planned decisions. That’s going to begin in 2026 and will go a long way in bringing much-needed transparency and accountability to the entire process.
Appeals Process
While the option to appeal a prior authorization denial exists, it can be a lengthy and complex process. Patients may need to provide additional documentation and evidence to support their case, which can be challenging and time-consuming.
In the efforts to improve the Medicare Advantage prior authorization process, CMS will require, according to Dr. Ehrenfeld,
Plans to support an electronic prior authorization process that’s embedded in the physician’s electronic health records, bringing much needed automation and efficiency to our current very manual and very time-consuming workflow. That change is going into effect in 2027—it’s going to be a game-changer for everybody.
So having direct integration of prior authorization into the EHR (electronic health record) is going to significantly reduce the burden on physicians. And this is where so much of that $10 to $15 billion in savings is going to come from.
Despite these challenges, some strategies and tips can help you navigate the prior authorization process more effectively.
 Navigating the Prior Authorization Process Effectively
Navigating the Prior Authorization Process Effectively
Navigating the prior authorization process can be overwhelming, but with the right strategies, you can streamline the process and ensure a smoother experience. Here are some tips to help you navigate prior authorization effectively:
Understand your Medicare Advantage Plan
Familiarize yourself with your Medicare Advantage plan’s specific requirements and guidelines. This will help you understand which procedures and services require prior authorization and what documentation is needed. This is important because you may have to be the force behind the doctor’s office to pursue approval beyond the initial request.
Communicate with Your Healthcare Provider
It is crucial to communicate openly and clearly with your healthcare provider. They can guide you through the prior authorization process, provide necessary documentation, and advocate for your needs. The office needs to see that you want the procedure or test because they have limited resources to pursue further requests or appeals from the insurance company.
Gather All Necessary Documentation
Before submitting a prior authorization request, ensure you have all the necessary documentation. This may include medical records, test results, treatment plans, and any additional information requested by your insurance company. If you can assist in the process, then dig in. You may also have to be the supervising authority to make sure the office’s back office submits all relevant materials.
Be Proactive
Start the prior authorization process as early as possible to avoid delays in care. Submit your request well in advance of your scheduled procedure or treatment to allow ample time for review. Doctor’s offices are usually overworked and understaffed. To ensure you are taken care of in a timely way, contact the office yourself to see where your prior authorization is in the process. Ask for dates when you should expect tasks to be completed by the doctor’s office and insurance company.
Keep Copies of All Documents
Make copies of all documents related to the prior authorization process, including your request, supporting documentation, and any communication with your insurance company. This will help you stay organized and provide evidence if needed for an appeal. The documents are your records. You and the insurance company paid for the tests, and you have a right to your own copies.
Follow Up with Your Insurance Company
Stay proactive and follow up with your insurance company to ensure your prior authorization request is processed. This will help you stay informed and address any issues or concerns in a timely manner. Everyone is busy. Balls are dropped. People forget. You make sure none of that happens with your case because you are on it.
How to Appeal a Prior Authorization Denial
If your prior authorization request is denied, you have the option to appeal the decision. Here’s a step-by-step guide on how to appeal a prior authorization denial.
- Understand the denial: Carefully review your insurance company’s denial letter. Understand the reasons for the denial and the specific requirements for appealing the decision.
- Gather additional documentation: If you believe that the denial was made in error or that additional information could support your case, gather all the necessary documentation. This may include medical records, test results, or a letter of medical necessity from your healthcare provider. Your provider will need to perform most of this work.
- Submit an appeal letter: Write a formal appeal letter to your insurance company. Generally the doctor will need to draft and submit the letter. He will need to more clearly state the reasons for your request, provide supporting documentation, and explain why you believe the requested service is medically necessary.
- Follow up with your insurance company: This is where you can help the process. Stay in contact with your insurance company to ensure your appeal is processed. Follow up regularly. You will be able to follow up more readily than the provider’s office. Get any additional information or documentation requested.
Remember, the appeals process may take time, and no approval is guaranteed. However, following these steps and providing compelling evidence increases your chances of a favorable outcome.
Bottom Line: Understanding Medicare Advantage Prior Authorization May Determine Your Success
In conclusion, understanding and managing Medicare Advantage prior authorization is crucial for both patients and healthcare providers. While the process can be complex and time-consuming, it ensures that healthcare services are medically necessary and cost-effective.
By familiarizing yourself with the prior authorization process, understanding your Medicare Advantage plan requirements, and effectively communicating with

your healthcare provider and insurance company, you can navigate this system with confidence and ease.
Remember to stay proactive, gather all necessary documentation, and be prepared to advocate for your needs. In the event of a denial, don’t hesitate to appeal and seek assistance if needed.
Empower yourself with knowledge and take control of your healthcare journey. With the right information and resources, you can successfully navigate Medicare Advantage prior authorization and receive the care you need.
Are you searching for a trustworthy Medicare Advantage plan insurance agent near you? Look no further! In this article, we will provide you with key tips and insights to help you find the right agent to meet your healthcare needs. Medicare Advantage plans offer additional benefits beyond the basic coverage of Original Medicare. Choosing the right plan can be overwhelming. So, who’s the trustworthy Medicare Advantage plan insurance agent near me?
Finding a trusted agent involves more than just a quick Google search. It requires careful consideration and research. We will guide you through the process, outlining important factors to consider when selecting an agent. From checking their credentials and experience to evaluating their customer satisfaction ratings, we will provide you with the tools you need to make an informed decision.
By the end of this article, you will clearly understand what to look for in a Medicare Advantage plan insurance agent near you. So, let’s dive in and find the perfect agent to help you navigate the complex world of Medicare Advantage plans.
 Understanding Medicare Advantage Plans
Understanding Medicare Advantage Plans
Medicare Advantage plans, also known as Medicare Part C, are private health insurance plans that provide an alternative to Original Medicare. These plans are offered by private insurance companies approved by Medicare. They combine the coverage of Medicare Parts A and B, and often include additional benefits such as prescription drug coverage, dental, vision, and hearing services, and wellness programs.
Medicare Advantage plans come in different types, including Health Maintenance Organizations (HMO), Preferred Provider Organizations (PPO), and Special Needs Plans (SNPs). Each type has its own network of doctors, hospitals, and other healthcare providers. It’s important to understand the differences between these plan types and choose the one that best suits your needs.
The Importance of a Trustworthy Medicare Advantage Insurance Agent
Navigating the world of Medicare Advantage plans can be confusing. That is why working with a trustworthy insurance agent is crucial. A reliable agent can help you understand the complexities of different plan options, guide you through the enrollment process, and provide ongoing support for any questions or concerns you may have.
A trustworthy insurance agent is knowledgeable about Medicare rules and regulations, stays up to date with changes in the healthcare industry, and has a good understanding of the Medicare Advantage plans available in your area. They should be able to explain the pros and cons of each plan, and help you determine which plan aligns with your specific healthcare needs and budget.
Researching Medicare Advantage Insurance Agents Near Me
When searching for a Medicare Advantage plan insurance agent near you, it’s important to conduct thorough research to ensure you find a trustworthy professional. Here are some key steps to follow.
 Checking for Licenses and Certifications
Checking for Licenses and Certifications
Start by checking if the agent is licensed to sell Medicare Advantage plans in your state. The agent should hold a valid insurance license and be authorized to sell Medicare products. You can verify their license status with your state’s insurance department or through the National Insurance Producer Registry (NIPR) website.
Local Department of Insurance Website
For Nebraska, you can go to the Nebraska Department of Insurance website. Once there, look at the tabs on the top of the page. Go to Policyholder. Under that tab, there is Agent/Company Search. Click Agent/Agency Search. Pick the state and choose the licensee. Type in the last name. You don’t need the agent number, but it helps, especially with common last names. There is your agent.
The importance of checking out an agent is you can quickly verify if he is licensed in your state. You can see how long he has held an insurance license. The date of the first activation will be there.
That may not be completely accurate, however. I noticed my activation date is 2012. I was first licensed in Nebraska in 2002, but I moved outside of Nebraska for a short time. My residence insurance license was not Nebraska, I was a non-residence licensed agent for Nebraska. Then, I returned in 2012 to Nebraska. So, the Nebraska Dept of Insurance site does not show the lifetime duration of a licensee.
Insurance Company Appointments
Toward the bottom of the page are the agent’s appointments. You must be licensed to sell insurance in a particular state. You must be licensed in each state you sell, and you must be appointed with each insurance company before you sell their products.
Medicare Certification
Insurance company appointments may require product training before you can be appointed. Sometimes you must pay a fee to be appointed. Insurance companies that offer Medicare Advantage plans require the agent to pass the AHIP exam. You only get three tries to pass the exam. If you fail the 3rd try, you cannot sell any Medicare Advantage plans or Part D prescription drug plans for any insurance company in any state.
After you pass the AHIP, you submit the certification to the insurance company. Then, you must pass the individual product training for each Medicare product you wish to sell. Again, there is a limited amount of time you can take the test to pass.
Then, the appointment paperwork is completed. Your appointment is listed on your state insurance department’s website. If not appointed, the agent cannot sell that company and/or product.
I recall meeting with a couple once whose financial advisor said he could get them any plan they wanted, including Medicare Advantage. I was suspicious because most financial advisors who offer financial advice as their primary business generally do not get deeply involved in Medicare. When I looked them up on the Nebraska Dept of Insurance, they were not appointed with any of the Medicare Advantage carriers in the area.
Reading Reviews & Testimonials
Online reviews and testimonials can provide valuable insights into the quality of service provided by the Medicare Advantage insurance agents near you.
I do not like to shop, so I use Amazon for a lot of my shopping. Once I know what I want, I look at star ratings and reviews. More and better reviews, the higher the chance I click on that product.
Look for reviews on reputable websites, such as Google, Facebook, or the Better Business Bureau. Pay attention to overall ratings, as well as specific feedback regarding the agent’s knowledge, responsiveness, and ability to help clients find suitable Medicare Advantage plans.
It’s important to note that while reviews can be helpful, they should be considered along with other factors. Negative reviews may not always reflect the agent’s true capabilities, as individual experiences can vary. Use reviews as a starting point for further investigation and gathering more information about the agent.
Referrals from Friends and Family
Reach out to friends, family members, or colleagues who have experience with Medicare Advantage plans. Ask them if they have worked with a trustworthy insurance agent and if they would recommend their services. Personal recommendations can be invaluable, as they come from people you trust who have first-hand experience with the agent’s professionalism and expertise.
Keep in mind that everyone’s healthcare needs are different, so while a certain agent may have been a great fit for someone you know, it doesn’t guarantee the same experience for you. Still, personal recommendations can help you narrow down your options and consider agents who have a proven track record of delivering excellent service.
Most of my new clients come from client referrals. The difference between referrals and prospects who come to us through other marketing avenues is usually night and day.
The trust level is already there because a trusted friend or family member referred them. The prospect starts learning about Medicare and the insurance products right from the start because they trust us. While we still work on building repertoire, there is enough trust present so they are listening attentively and learning what they need to know from the beginning. They can make much better decisions about their Medicare.
 Meeting with a Medicare Advantage Insurance Agents Near Me
Meeting with a Medicare Advantage Insurance Agents Near Me
Once you have identified a few potential Medicare Advantage insurance agents near you, it’s time to schedule consultations to further assess their suitability. Meeting face-to-face or having a phone conversation allows you to gauge their expertise, ask important questions, and evaluate their communication skills. Trust is built not only upon believing the person has your best interest at heart. Trust is also built on competence. Does he know what he’s talking about?
During the meeting, pay attention to the agent’s ability to explain complex concepts clearly and understandably. They should be patient, attentive, and willing to address your concerns. Consider their level of professionalism, as well as their ability to listen and tailor their recommendations to your unique needs.
Do they show you the universe of Medicare Supplements, Medicare Advantage plans, and Medicare Part D Prescription Drug plans in your area? Or do they go immediately to only one or two companies? Or do they only do Medicare Advantage or only offer Medicare Supplements?
You want an independent agent or broker who represents most companies and plans in your areas and can objectively and impartially present all your Medicare options. Then, he can take you through the process of matching the various plans and their benefits to your unique needs and concerns. One size does not fit all.
Questions to Ask a Medicare Advantage Insurance Agent
To ensure you make an informed decision, it’s essential to ask the right questions during your meetings with potential insurance agents. Here are some basic questions to consider:
- Can you explain the different types of Medicare Advantage plans available in my area?
- How do these plans differ in terms of cost, coverage, and network of providers?
- What additional benefits can I expect from the Medicare Advantage plans you recommend?
- How do I know if my preferred doctors and hospitals are included in the plan’s network?
- What prescription drug coverage options are available?
- Can you provide an estimate of the monthly premiums, deductibles, and out-of-pocket costs for the plans you recommend?
- How do I qualify for extra help with Medicare costs, such as the Low-Income Subsidy?
Asking these questions will help you gain a better understanding of the agent’s knowledge, expertise, and ability to find a plan that meets your healthcare and financial needs.
Comparing Quotes and Plans
 After meeting with several insurance agents and gathering information, it’s time to compare the quotes and coverage options they have provided. Keep in mind that the lowest premium may not always be the best option, as it’s important to consider factors such as deductibles, copayments, and the network of providers.
After meeting with several insurance agents and gathering information, it’s time to compare the quotes and coverage options they have provided. Keep in mind that the lowest premium may not always be the best option, as it’s important to consider factors such as deductibles, copayments, and the network of providers.
Evaluate the coverage options based on your specific healthcare needs. Consider factors such as prescription drug coverage, access to specialists, and the availability of preferred hospitals or healthcare facilities. Consider the estimated out-of-pocket costs for each plan, including copayments, coinsurance, and deductibles.
Enrolling in a Medicare Advantage Plan with Your Local Agent
Once you have thoroughly researched and compared the different Medicare Advantage plans and insurance agents, you should have at least a couple of names to answer the questions: who’s the trustworthy Medicare Advantage plan insurance agent near me?
Contact the chosen agent and inform them of your decision. They will guide you through the enrollment process, ensuring that you understand the terms and conditions of the plan you have selected.
Remember to review all the relevant documents, including the Summary of Benefits and the plan’s provider directory. If you have any doubts or questions, don’t hesitate to reach out to your agent for clarification.
At Omaha Insurance Solutions, we have taken thousands of clients over the years through the process of understanding and selecting the Medicare plan that best fits their needs, and each year, we review that

Christopher Grimmond
plan to make sure it still meets their needs.
Give us a call at 402-614-3389 for a free, no-obligation consultation to find out your Medicare options.
 Are you ready to unlock the potential benefits of Medicare Advantage in your area? Look no further. This informative article will explore the advantages of Medicare Advantage plans and how they can enhance your healthcare coverage.
Are you ready to unlock the potential benefits of Medicare Advantage in your area? Look no further. This informative article will explore the advantages of Medicare Advantage plans and how they can enhance your healthcare coverage.
Medicare Advantage, also known as Medicare Part C, goes beyond what Original Medicare provides. With a Medicare Advantage plan, you can enjoy additional benefits like prescription drug coverage, dental care, and vision services in one convenient package. But that’s not all – some plans even offer fitness memberships, transportation services, and telehealth options.
By delving into the specifics of Medicare Advantage, we’ll help you understand how these plans work, what they cover, and whether they align with your unique healthcare needs. We’ll also examine how you can find the right plan for you in your local area.
Don’t settle for one-size-fits-all healthcare coverage. Discover the customized benefits and added features that Medicare Advantage plans can offer. Read on to learn more about the advantages waiting for you right around the corner.
What is Medicare Advantage?
Medicare Advantage, also known as Medicare Part C, is a type of health insurance plan offered by private insurance companies that contract with Medicare. These plans provide an alternative way to receive your Medicare benefits, combining the coverage of Parts A (hospital insurance) and B (medical insurance) and often including additional benefits not covered by Original Medicare.
One key characteristic of Medicare Advantage plans is that they are required to provide at least the same level of coverage as Original Medicare. However, many plans go above and beyond. They put a cap on spending. Original Medicare is unlimited. There are small copays for services. Original Medicare Part B is an unlimited 20%. Part D prescription drug plans are usually included. With Original Medicare, you must purchase a separate Part D plan. Many Medicare Advantage plans have no deductible for the prescription side of the plan in the Omaha, Lincoln, & Council Bluffs areas. Most of the Part D plans have a large deductible. The most common deductible for 2024 is $545. Medicare Advantage offers additional benefits such as dental care, vision services, and hearing aids. That would be a separate policy and monthly premium on Original Medicare.
In summary, Medicare Advantage plans offer a comprehensive and convenient way to receive your Medicare benefits, often with added benefits not available through Original Medicare alone.
Medicare Advantage Enrollment & Eligibility
Now that we’ve explored the benefits of Medicare Advantage let’s discuss how you can enroll in a plan and determine your eligibility.
To be eligible for Medicare Advantage, you must meet the following criteria:
- You must be enrolled in both Medicare Part A and Part B. You still must continue to pay your Medicare Part B premium.
- You must live in the service area of the Medicare Advantage plan you wish to enroll in. If you leave that area, you will be disenrolled. You will then need to enroll in another plan in your new area in a timely manner.
Once you meet these eligibility requirements, you can enroll in a Medicare Advantage plan during specific enrollment periods.
- Initial Enrollment Period (IEP) occurs when you first become eligible for Medicare, typically three months before your 65th birthday, the month of your 65th birthday, and three months afterward.
- Annual Enrollment Period (AEP) takes place from October 15th to December 7th each year, during which you can switch or enroll in a Medicare Advantage plan.
- Special Election Periods (SEP) occur for special circumstances. For example, you move out of the service area. Another common SEP is when you lose employer health coverage. There are many others.
It’s important to note that Medicare Advantage plans may have different networks of doctors and healthcare providers, so it’s essential to confirm that your preferred healthcare providers are included in the plan’s network before enrolling. Each area has its unique circumstances.
Medicare Advantage in the Omaha, Lincoln, & Council Bluffs areas is exceptionally good when it comes to networks. There are four provider networks: CHI (Catholic Health Initiative), Methodist Health Systems, Nebraska Medicine (UNMC), and Bryan Health. All of these networks work with the six insurance companies with Medicare Advantage contacts in the area.
 Original Medicare vs. Medicare Advantage
Original Medicare vs. Medicare Advantage
Original Medicare is only Part A for hospital and Part B for doctor visits and outpatient services. Part A currently has a deductible of $1,632 for an event in 60 days. Part B is a 20% coinsurance that is unlimited.
Medicare Advantage covers the same as Part A & Part B, but there is a maximum out-of-pocket (MOOP). The MOOP is potentially $8,850 in-network and $13,300 out-of-network. These amounts are the maximum cap a plan can have. All Medicare Advantage plans MOOPs in Omaha, Lincoln, and Council Bluffs are much lower. The most popular plan MOOP is $3,800.
Medicare Advantage plans have small copays for various services. For example, doctor visits maybe 0-$10, emergency rooms $120-$135, and outpatient surgeries $250-$350. All of the copays go against the maximum out-of-pocket (MOOP).
How to choose the Right Medicare Advantage Plan for You
With numerous Medicare Advantage plans available, choosing the right one that meets your healthcare needs is crucial. Here are some factors to consider when selecting a Medicare Advantage plan:
Medications Covered
Run your medications through the various software available, including the Plan Finder on the Medicare.gov website. Make sure your medications are on the formulary. Look for the plans with the lowest total copays for your medications.
Provider Network
 Medicare Advantage is managed care, so there are networks, versus Original Medicare, which is fee-for-service (FFS). Check to make sure your doctors and hospitals are in the plan network.
Medicare Advantage is managed care, so there are networks, versus Original Medicare, which is fee-for-service (FFS). Check to make sure your doctors and hospitals are in the plan network.
We are fortunate to have strong network affiliations with the Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs. There are four networks: CHI, Nebraska Medicine, Methodist Health Systems, and Bryan Hospital. All six Medicare Advantage companies in our area work with these networks. However, we still check to confirm providers are in the network.
Maximum Out-of-Pocket in Budget
The maximum out-of-pocket is the most you must pay in a calendar year. Does that amount work in your budget? A Medicare Supplement coupled with Original will cost approximately $2,000-$3,000 per year, depending upon your age and location. You will pay the monthly Medicare Supplement premium regardless of any medical expenses. With an Advantage plan, you only pay copays if you see a doctor or have something done medically.
HMO vs. PPO
Medicare Advantage plans that are Health Maintenance Organizations (HMO) will only pay for services provided in the plan’s network. That is the limitation. When traveling, you are covered anywhere for an emergency.
Medicare Advantage plans that are Preferred Provider Organizations (PPO) cover services in and out of the network. Out-of-network care providers who accept Medicare but are not in the local service area network are covered. Those providers may charge more, and the maximum out-of-pocket expenses are usually larger.
PPO plans are best for people living in multiple locations or with limited local network coverage. Again, a PPO Medicare Advantage Plan has no real advantage in the Omaha, Lincoln, and Council Bluffs areas because all providers are in the four local networks.
Many insurance companies with Medicare Advantage contracts also have national networks. That means you can access doctors and hospitals in other parts of the country far from home, still be in the network, and pay in-network copays. It is always important to confirm a provider’s status before seeking treatment. I have had a number of clients leave the Omaha area and go to facilities in other states while on their HMO Medicare Advantage plan and pay in-network copays.
 Copays
Copays
To explore the Medicare Advantage plans available in your area, you can use the Medicare Plan Finder tool on the official Medicare website (medicare.gov). This tool allows you to enter your zip code and compare the different plans offered in your local area.
The Medicare Advantage comparison tool is helpful when looking at copays. There are many plans, and copays differ from plan to plan and service to service. If you are looking through company sales brochures, you will become cross-eyed. A comparison tool, either at Medicare.gov or through an insurance agent you are working with, will make the review process much more manageable.
Over the years, I have listened to many clients voice their opinions on which copays are more important than others. I try to make clients aware of essential copays and the differences between the plans. They come to their own conclusions and rankings for the plans based on what they see.
Additional Benefits
The big attraction of Medicare Advantage is the additional benefits. It is interesting to listen to clients’ comments and compare the additional benefits between plans. Those who don’t wear glasses pass over that benefit, and those who have issues with their teeth will laser focus on the size of the dental benefit and the network.
Over-the-counter (OTC) benefits are getting a second glance this year because some companies reduced their amount, and another company kept it comparatively large. When the plans are very similar in terms of all other benefits, one benefit, like OTC, can make the deciding difference.
Once you have covered these essential aspects of the plans in your area, you should have a feeling about which plan (or plans) best address your needs. Going through this checklist will narrow your selection to a plan or couple of plans that will serve you best.
Exploring Medicare Advantage Plans in Your Area
 Some large metro areas have many, many plans. In the Omaha area, we have six insurance companies that offer 27 Medicare Advantage plans in the Nebraska counties of Douglas, Sarpy, Washington, Cass, Saunders, and Lancaster, and five insurance companies offer 26 plans in Pottawatomie County in Iowa.
Some large metro areas have many, many plans. In the Omaha area, we have six insurance companies that offer 27 Medicare Advantage plans in the Nebraska counties of Douglas, Sarpy, Washington, Cass, Saunders, and Lancaster, and five insurance companies offer 26 plans in Pottawatomie County in Iowa.
So there is an excellent variety. The complaint I hear quite often is that there are too many choices. The large number of plans and the different copay amounts and benefits are overwhelming and make the selection process confusing for many of my clients.
If an independent agent lives and works in the area, he should be able to compare and explain most plans. One of the problems I have with agents out of call centers in Florida, California, or the Philippines is that they do not know the local area and the plans because they don’t live here. They are unaware of the subtle differences between the companies and plans. The telesale agent has no lived experience or history with the Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs.
Their primary concern is to switch you into the plan they are selling so they get paid. If there are problems later, they will not be there to answer your calls. They may not even be in the business after Open Enrollment.
Bottom Line: Is Medicare Advantage Right for You?
Medicare Advantage plans offer a wealth of benefits and added features that can enhance your healthcare coverage. From additional benefits like prescription drug coverage and dental care to added perks like fitness memberships and telehealth options, Medicare Advantage plans provide a comprehensive and convenient way to receive your Medicare benefits.
When considering Medicare Advantage, it’s important to carefully compare the plans available, review their coverage and benefits, and consider your specific healthcare needs. Doing so lets you choose the right Medicare Advantage plan that aligns with your preferences and provides the coverage you require.
Unlock the potential benefits of Medicare Advantage in your area. With over two decades of experience at Omaha Insurance Solutions, we know the Medicare Advantage plans well in Nebraska & Iowa. We can guide you through the selection process.
 With the right plan, you can enjoy comprehensive benefits, cost savings, and a more convenient healthcare experience. Take control of your healthcare today and call us at 402-614-3389 to speak with an insurance agent professional to explore the possibilities of Medicare Advantage.
With the right plan, you can enjoy comprehensive benefits, cost savings, and a more convenient healthcare experience. Take control of your healthcare today and call us at 402-614-3389 to speak with an insurance agent professional to explore the possibilities of Medicare Advantage.
 Are you looking to maximize your healthcare coverage? In this article, we will explain the benefits of Medicare Advantage Part C, helping you make informed decisions about your healthcare options. Medicare Advantage Part C offers an alternative to traditional Medicare coverage, providing additional benefits and services to enhance your overall healthcare experience.
Are you looking to maximize your healthcare coverage? In this article, we will explain the benefits of Medicare Advantage Part C, helping you make informed decisions about your healthcare options. Medicare Advantage Part C offers an alternative to traditional Medicare coverage, providing additional benefits and services to enhance your overall healthcare experience.
With Medicare Advantage Part C, you can enjoy prescription drug coverage, vision and dental care, and even fitness programs. These additional services can save you money and provide comprehensive coverage tailored to your specific needs.
But how do you know if Medicare Advantage Part C is correct for you? We’ll explore the eligibility criteria and factors to consider when weighing your options. Understanding the ins and outs of Medicare Advantage Part C will empower you to make the best choice for your healthcare needs.
So, if you’re ready to take control of your healthcare coverage and get the most out of your benefits, keep reading. Let’s dive into the Medicare Advantage Part C world and discover the possibilities it holds for you.
Understanding the Basics of Medicare Advantage Part C Benefits
Medicare Advantage Part C, also known as Medicare Advantage Plans, is a comprehensive healthcare option offered by private insurance companies approved by Medicare. It combines the benefits of Medicare Parts A & B, and usually Part D, as well as additional services and coverage options. Medicare Advantage Part C is managed care, which means it is a network system. Doctors, hospitals, and clinics contract with the insurance company.
One of the key advantages of Medicare Advantage Part C is that it often includes prescription drug coverage, known as Medicare Part D, which is not included in Original Medicare. This means you can cover all your healthcare needs, including medications, under a single plan. Additionally, many Medicare Advantage plans offer extra benefits such as vision and dental care, hearing aids, and even fitness programs to help you stay healthy and active.
But how do you know if Medicare Advantage Part C is right for you? Let’s explore the eligibility criteria and factors when weighing your options.
The Benefits of Medicare Advantage Part C
Medicare Advantage Part C offers a wide range of benefits that can significantly enhance your healthcare coverage. These benefits can include:
include:
- Comprehensive coverage: Medicare Advantage Part C combines the benefits of Medicare Parts A and B, providing hospital insurance (Part A) and medical insurance (Part B) in one plan. This means you have coverage for hospital stays, doctor visits, preventive care, and more.
- Prescription drug coverage: Many Medicare Advantage plans include prescription drug coverage, allowing you to obtain your medications conveniently through the same plan. This can save you money and reduce the hassle of managing multiple insurance providers.
- Additional services: Medicare Advantage Part C plans often offer additional services not covered by Original Medicare, such as vision and dental care, hearing aids, and wellness programs. These services can help you maintain your overall health and well-being.
- Out-of-pocket cost protection: Medicare Advantage plans have a cap on out-of-pocket expenses, providing financial protection in case of unexpected medical costs. This can bring peace of mind and help you plan your healthcare budget more effectively.
How to Qualify for Part C
 To be eligible for Medicare Advantage Part C, you must meet the following requirements:
To be eligible for Medicare Advantage Part C, you must meet the following requirements:
- Enrollment in Medicare Parts A and B: You must be enrolled in both Medicare Part A (hospital insurance) and Part B (medical insurance) to be eligible for Medicare Advantage Part C.
- Residency: You must reside in the service area of the Medicare Advantage plan you wish to join. Residency is important to remember. I have had clients move without telling me or the plan. They are then surprised when their coverage doesn’t work or is even canceled.
It’s important to note that eligibility requirements may vary depending on the specific Medicare Advantage plan and insurance provider. There are special needs plans for those on state Medicaid or with chronic health conditions like diabetes, COPD, or heart disease. These plans have additional requirements.
Review the requirements and seek guidance from a qualified insurance agent to ensure you meet the eligibility criteria. These plans have even richer benefits for those who qualify.
Differences Between Original Medicare Vs. Medicare Advantage
While Original Medicare and Medicare Advantage Part C both provide healthcare coverage, there are some key differences between the two:
- Coverage options: Original Medicare consists of Part A (hospital insurance) and Part B (medical insurance), while Medicare Advantage Part C combines both Parts A and B into a single plan. Medicare Advantage plans also often include additional benefits, such as prescription drug coverage and extra services.
- Network restrictions: Original Medicare allows you to go to any doctor or hospital that accepts Medicare, while Medicare Advantage plans typically have a network of providers you must use to receive full coverage. However, some Medicare Advantage plans offer out-of-network coverage for higher out-of-pocket costs.
- Cost structure: Original Medicare deductibles and coinsurance have no cap or maximum out-of-pocket. Many purchase
 additional coverage—a Medigap plan—to cover the significant gaps in coverage. This additional insurance comes at an additional cost. Medicare Advantage has minimal copays with a maximum out-of-pocket as well as additional benefits. Most of the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs area have zero monthly premium. You simply continue to pay your Medicare Part B premium, which you are paying anyway.
additional coverage—a Medigap plan—to cover the significant gaps in coverage. This additional insurance comes at an additional cost. Medicare Advantage has minimal copays with a maximum out-of-pocket as well as additional benefits. Most of the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs area have zero monthly premium. You simply continue to pay your Medicare Part B premium, which you are paying anyway. - Flexibility: Original Medicare allows you to see any specialist or visit any healthcare provider without a referral. While some Medicare Advantage HMO plans in other parts of the country require referrals to see specialists, the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas are open access. Open Access means you can see any specialist in the network without a referral.
Considering these differences can help you determine which type of coverage aligns best with your healthcare needs and preferences.
Choosing the Right Medicare Advantage Part C Plan
 Choosing the right Medicare Advantage Part C plan requires careful consideration of your healthcare needs and personal preferences. Here are some factors to consider when selecting a plan:
Choosing the right Medicare Advantage Part C plan requires careful consideration of your healthcare needs and personal preferences. Here are some factors to consider when selecting a plan:
- Coverage and benefits: Review the coverage options and benefits offered by different Medicare Advantage plans. Consider your specific healthcare needs, such as prescription drugs, vision, and dental care, or fitness programs, and choose a comprehensive plan for your requirements.
- Provider network: Check whether the plan’s network includes your preferred doctors, hospitals, and specialists. Ensure the plan’s network is convenient and accessible for your healthcare needs. All four networks work with the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas. If the provider is part of CHI, Nebraska Medicine, Methodist Health Systems, or Bryan Health, they will be in the network.
- Costs: Compare the costs associated with different Medicare Advantage plans, including monthly premiums, deductibles, copayments, and coinsurance. Consider your budget and evaluate which plan offers the most cost-effective coverage for your needs.
I recommend starting with the maximum out-of-pocket (MOOP) amount and the star rating. Maximum out-of-pocket is what you have at risk. The star rating can help you narrow down the plans that have been around for a while and have a good service record.
Researching and comparing different Medicare Advantage plans can help you select the best plan that aligns with your healthcare needs and budget. At Omaha Insurance Solutions, we help clients evaluate the universe of Medicare plans quickly & easily using our sophisticated but user-friendly software, and with over a decade of experience, we know the local Medicare plans intimately.
Exploring Additional Benefits
Medicare Advantage Part C plans often provide additional benefits that go beyond what Original Medicare offers. These benefits can vary depending on the specific plan and insurance provider, but commonly include:
- Vision and dental care: Many Medicare Advantage plans cover routine vision and dental services, including exams,
 cleanings, and eyeglasses.
cleanings, and eyeglasses. - Hearing aids: Some plans offer coverage for hearing aids and related services, helping you maintain your hearing health.
- Fitness programs: Medicare Advantage plans may provide access to fitness programs, gym memberships, or wellness classes to help you stay active and improve your overall health. I belong to the Genesis Health Clubs in Omaha. My membership is almost $600 a year. I would be very happy to have my health insurance plan pay that fee. I’m looking forward to Medicare. In the Silver Sneakers and Renew Active Programs, you can actually join multiple gyms. You are not limited to one chain or a single club.
- Transportation services: Certain plans offer transportation services to and from medical appointments, ensuring you can get the care you need even if you don’t have reliable transportation.
These additional benefits can significantly enhance your healthcare experience and provide you with comprehensive coverage tailored to your specific needs. Original Medicare does not provide these benefits. If you want additional benefits, you must purchase them at additional costs.
 Common Misconceptions about Medicare Advantage Part C
Common Misconceptions about Medicare Advantage Part C
There are several misconceptions surrounding Medicare Advantage Part C. Let’s address some of the most common ones:
- Limited provider choice: While provider networks are not an issue with the Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas, it certainly may be a concern in other places. There are typically, however, many options to choose from within most networks. Additionally, some plans offer out-of-network coverage for higher out-of-pocket costs.
- Lack of coverage for pre-existing conditions: Medicare Advantage plans cannot deny coverage based on pre-existing conditions. They must cover all services covered by Original Medicare, even if you have a pre-existing condition.
- Difficulty changing plans: Medicare beneficiaries have the opportunity to change their Medicare Advantage plans during the Annual Enrollment Period, which typically occurs from October 15th to December 7th each year. They also have a second opportunity during the Open Enrollment Period, which occurs from January 1st to March 31st, to make a one-time change to a Medicare Advantage plan.
- Higher costs: While Medicare Advantage plans have copays and coinsurance, these copays are generally small and have a cap. Medigap plans have a monthly cost that increases with age and usually exceeds annual copays on Medicare Advantage plans most of the time in most years.
Understanding these misconceptions can help you make informed decisions about Medicare Advantage Part C and ensure you have accurate information when considering your healthcare options.
Tips for Maximizing Your Medicare Advantage Part C Benefits
To make the most of your Medicare Advantage Part C benefits, consider the following tips:
- Review your plan annually: Medicare Advantage plans can change their coverage and benefits each year. Take the time to review your plan’s Annual Notice of Change (ANOC) to ensure it still meets your healthcare needs. Check the cost of medications for the coming year. We offer an annual review to our clients. However, some clients ignore our letters, emails, and phone calls to meet. We get distressed calls in the new year when plan changes catch up with some folks.
- Stay within your plan’s network: To receive full coverage and avoid higher out-of-pocket costs, use healthcare providers within your plan’s network. If you need to see a specialist or receive services outside the network, consult your plan’s guidelines for appropriate referrals or prior authorization. As I said earlier, this is generally not an issue in our area with doctors and hospitals; problems can arise with dentists and optimists who are not within the network. Double-check with the network because providers do change who they work with.
- Take advantage of additional benefits: Explore the extra benefits offered by your Medicare Advantage plan, such as vision and dental care or fitness programs. Utilizing these services can help you stay healthy and maximize the value of your plan. These Medicare Advantage Part C benefits save you money. I’m surprised when clients don’t utilize the over-the-counter benefit. In some cases, that is hundreds of dollars not coming out of your pocket.
- Understand your costs: Familiarize yourself with your plan’s copayments, deductibles, and coinsurance to avoid unexpected expenses. Knowing your costs upfront can help you budget for healthcare expenses more effectively. I always recommend clients talk with the doctor’s back office before any procedure is performed. Make sure the office received any prior approvals and find out the approximate cost to you beforehand so there are no surprises.
Following these tips can optimize your healthcare coverage and ensure you get the most out of your Medicare Advantage Part C plan.
Bottom Line: Making the Most of your Medicare Advantage Part C Benefits
Medicare Advantage Part C offers a comprehensive and flexible alternative to traditional Medicare coverage. With additional benefits such as prescription drug coverage, vision and dental care, and fitness

Christopher J. Grimmond, MA, CFP
programs, Medicare Advantage plans can provide you with comprehensive coverage tailored to your specific needs. Understanding the basics of Medicare Advantage Part C, eligibility criteria, and differences from Original Medicare is crucial in making informed decisions about your healthcare options.
By choosing the right Medicare Advantage Part C plan, exploring additional benefits, and maximizing your coverage, you can take control of your healthcare and enjoy comprehensive and cost-effective coverage.
If you’re ready to maximize your healthcare coverage and get the most out of your benefits, consider exploring the possibilities of Medicare Advantage Part C. Take charge of your healthcare journey today. Give us a call at Omaha Insurance Solutions at 402-614-3389 to view the Medicare Advantage Part C plans you are eligible for in your area to ensure a healthier and more secure future.
 Is it overwhelming to choose the best Medicare plan for your needs? With so many options available, it’s understandable. But worry not because we have your ultimate solution – the Medicare Plan Comparisons Chart.
Is it overwhelming to choose the best Medicare plan for your needs? With so many options available, it’s understandable. But worry not because we have your ultimate solution – the Medicare Plan Comparisons Chart.
The best way to compare is side-by-side. We can see each relevant benefit or cost in chart form and compare apples to apples. There is still a lot of information to comb through and remember, but a chart helps to reduce some of the confusion and the mental work of remembering what each Medicare plan offers.
Whether you’re looking for a plan that covers prescription drugs, outpatient surgeries, or dental more favorably, you can look at your options in the Medicare plan comparison chart.
By utilizing this user-friendly chart, you can easily compare different plans side by side, evaluate their features and benefits, and make an informed decision based on your unique healthcare needs.
Choosing the right Medicare plan is crucial because it directly impacts your overall health and pocketbook. At Omaha Insurance Solutions, we aim to simplify your Medicare selection process by providing all the necessary information in one place. With a Medicare Plan Comparisons Chart, you can confidently select the plan that meets your specific requirements and enjoy peace of mind knowing that you have made the best choice for your healthcare coverage.
Understanding Medicare Plans
Medicare is a federal health insurance program that provides coverage for individuals aged 65 and older and younger individuals with certain disabilities. It consists of different parts, each covering specific services and treatments.
To understand which Medicare plan is best for you, it’s essential to familiarize yourself with the different types of plans available and their respective coverage options. This knowledge will enable you to make an informed decision based on your healthcare needs.
Types of Medicare Plans
There are four main types of Medicare plans: Original Medicare (Part A and Part B), Medicare Advantage (Part C), Medicare Supplement Insurance (Medigap), and Prescription Drug Coverage (Part D).
- Original Medicare (Part A and Part B): This is the traditional Medicare plan offered by the government. Part A covers hospital stays, skilled nursing facility care, and some home health services, while Part B covers doctor visits, outpatient care, and preventive services.
- Medicare Advantage (Part C): This is Medicare offered through a private insurance company approved by Medicare. It provides all the benefits of Original Medicare, along with additional coverage for prescription drugs, dental, vision, and hearing services.
- Medicare Supplement (Medigap) plans are designed to fill the gaps in Original Medicare coverage. They help pay for out-of-pocket costs such as deductibles, coinsurance, and copayments. Private insurance companies offer Medigap plans, which are standardized across the states.
- Prescription Drug Plans (Part D): Part D plans are standalone plans offered by private insurance companies. They provide coverage for prescription drugs and can be added to Original Medicare, Medicare Advantage, and some Medicare Cost Plans.
Medicare Plan Comparison Chart
The Medicare Plan Comparisons Chart is a powerful tool that allows you to compare different Medicare plans side by side. It provides a clear and concise overview of each plan’s coverage details, costs, and additional benefits.
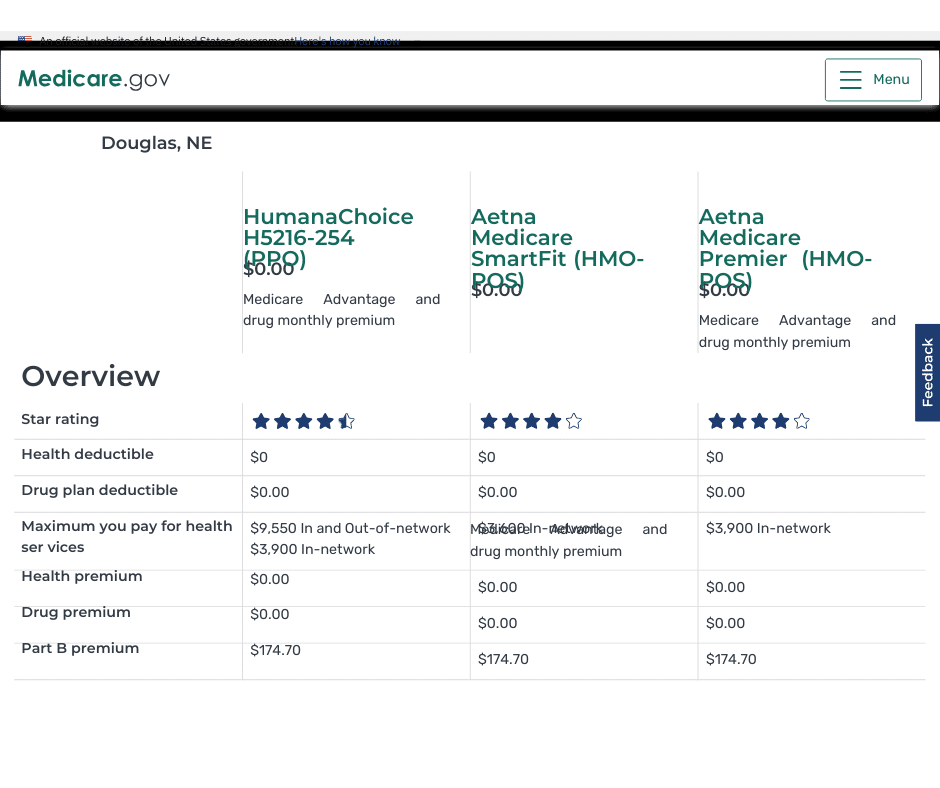
Where Can You Find A Chart?
A public tool is on the Medicare website. Type Medicare.gov in your browser address bar and hit enter. You will be taken to the official Medicare website. Click on the button for “Find health & drug plans.” You can create your own account or just type in your zip code without creating an account.
Choose the type of plans you wish to compare: Medicare Advantage Plan (Part C), Medicare drug plan (Part D), or Medigap policy.
Click the button that applies to your situation. Do you get financial help with your plan or not? If you qualify, financial help would be from Nebraska or Iowa Medicaid. Have you qualified for EXTRA HELP? Click Next.
Prescription Drug Comparison
The tool will ask if you wish to include drug costs—type in the specific medications with the dosages.
You may use various filters, but before that, scroll down and look at the plans first. You can look at each plan individually and study the benefits and pricing. There is also a box to check “Add to compare” to examine the plans side-by-side. You are limited to 3 plans at a time.
At the bottom of the screen, you can see the plans’ names and a comparison button. Click the comparison button to bring them up on the screen. The plans will be placed side by side, and all the categories will be matched up between them.
You can see the similarities and differences between the plans in one place and make your determinations. The limitation is that the Medicare.gov software does not provide great detail about the plans individually or together.
At Omaha Insurance Solutions we use a propriety software that goes into much greater detail about each plan. You can see the most common medical plan details: doctor & specialist visits, inpatient & outpatient surgeries, skilled nursing stays, MRIs, and X-rays, etc., compared side-by-side and line by line. Medications are calculated in various totals and subtotals. The provider network search tool is right there to access and find out if your doctors are in the plan or not. We run hundreds of these Medicare plan comparison charts each year for the Medicare plans in the Omaha, Lincoln, & Council Bluffs areas. Contact us for a FREE comparison at 402-614-3389.
Medicare Plan Comparison Chart Interpretation
How do you interpret and analyze the information in front of you? Information can be overwhelming when there is a lot of it, and it is new and unfamiliar. 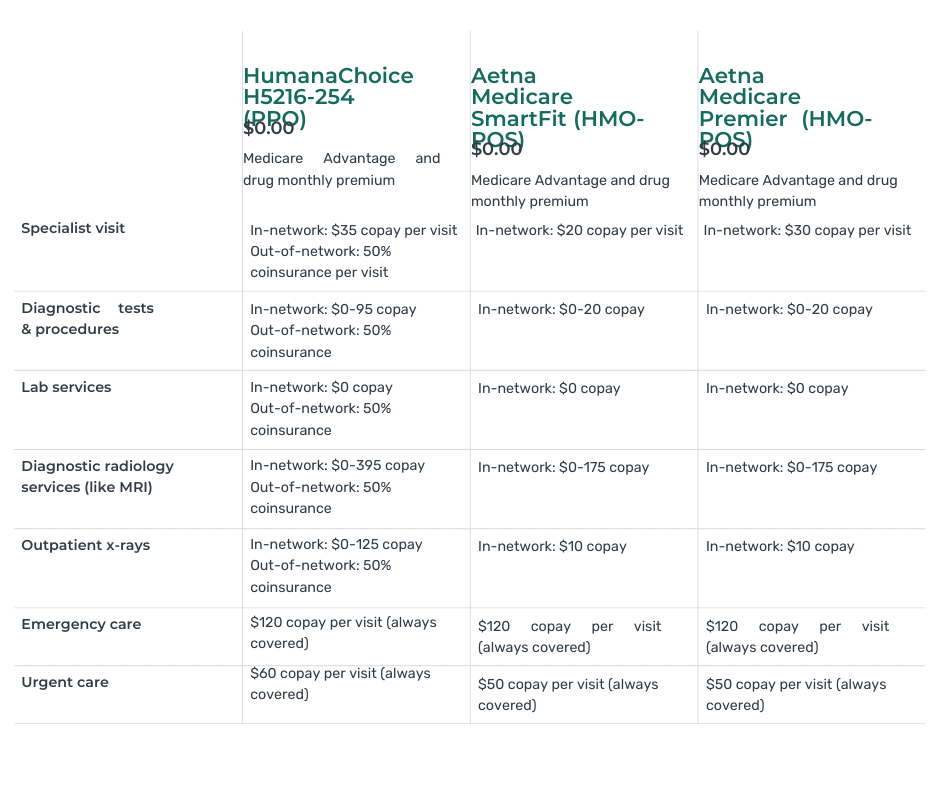
We help clients understand the information and how to weigh the various benefits, particularly in relation to their specific needs and ways of handling their health concerns.
Working with thousands of clients over many years with different health concerns that repeatedly ask many of the same questions, we have learned how to quickly assist you in evaluating and interpreting the information as it is relevant to your needs, situation, and budget.
The chart includes information such as monthly premiums, annual deductibles, coinsurance, copayments, and maximum out-of-pocket costs. It also highlights any limitations or restrictions that may apply to a plan.
By using the chart, you can quickly identify which plans offer the specific coverage you need. For example, if you require prescription drug coverage, you can quickly identify the plans that include Part D that cover your prescriptions at the most affordable prices. If you frequently travel and need coverage outside your local area, you can find plans that offer nationwide coverage.
Key Factors to Consider When Choosing a Medicare Plan
When comparing Medicare plans, there are several key factors to consider. These factors help you determine which plan best suits your needs and preferences. Here are some important considerations:
- Coverage: Evaluate each plan’s coverage options. Consider your existing health conditions and any specific treatments or services you anticipate needing in the future.
- Cost: Compare the costs associated with each plan, including premiums, deductibles, coinsurance, and copayments. Consider your budget and how much you can afford to pay for healthcare services.
- Provider Network: Check whether your preferred healthcare providers, such as doctors and hospitals, are included in the plan’s network. This ensures that you can continue receiving care from your trusted providers.
- Prescription Drug Coverage: If you take prescription medications, ensure the plan offers comprehensive coverage for the needed drugs. Review the formulary to see if your medications are included and at what cost.
- Additional benefits: Some Medicare plans offer additional benefits such as dental, vision, hearing coverage, OTC (Over-the-Counter) items, free gym memberships, and transportation. Consider whether these benefits are important to you and, whether they justify the additional cost, and which provide the maximum coverage.
How to Use the Medicare Plan Comparisons Chart Effectively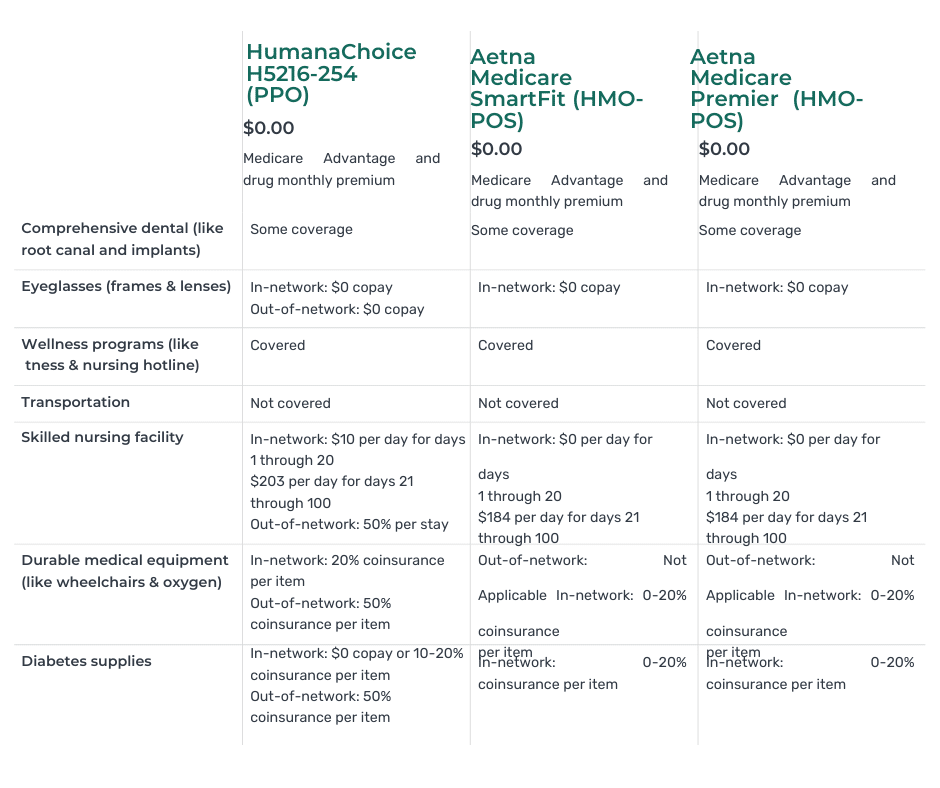
The Medicare Plan Comparisons Chart is designed to simplify choosing a Medicare plan. Here are some tips on how to use the chart effectively:
- Identify your healthcare needs: Before using the chart, take some time to assess your healthcare needs. Consider factors such as existing health conditions, prescription medications, and any specific treatments or services you anticipate needing in the future. This will help you narrow your options and focus on the plans that meet your requirements.
- Focus on relevant information: The chart provides detailed information about each Medicare plan, including coverage details, costs, and additional benefits. Focus on the information that is most relevant to your needs. For example, if you require prescription drug coverage, pay close attention to the details of Part D plans.
- Compare side by side: One of the greatest advantages of the chart is that it allows you to compare different plans side by side. This enables you to evaluate their features and benefits in a clear and concise manner. Take advantage of this feature to identify the plans that offer the specific coverage you need.
- Consider the cost: While coverage is necessary, it’s also essential to consider the cost associated with each plan. Evaluate factors such as monthly premiums, deductibles, copayments, and coinsurance. Consider your budget and how much you can afford to pay for healthcare services.
- Seek assistance if needed: If you find the process overwhelming or have specific questions about the chart or Medicare plans, don’t hesitate to seek assistance. Reach out to a licensed insurance agent or contact Medicare directly for guidance. Making an informed decision based on accurate and up-to-date information is important.
 Bottom Line: Finding the Best Medicare Plan for Your Needs
Bottom Line: Finding the Best Medicare Plan for Your Needs
Choosing the best Medicare plan for your needs is a crucial decision that directly impacts your healthcare coverage and bank account. With the help of the Medicare Plan Comparisons Chart, you can simplify this process and make an informed decision based on your unique healthcare needs.
By understanding the different types of Medicare plans, comparing their coverage options, and considering key factors such as cost, provider networks, and additional benefits, you can confidently select the plan that meets your specific requirements.
Remember to utilize the Medicare Plan Comparisons Chart effectively, focusing on relevant information, comparing plans side by side, and considering both coverage and cost. If needed, seek assistance from

Christopher Grimmond
licensed insurance agents, or contact Medicare directly for guidance.
With the right Medicare plan in place, you can enjoy peace of mind, knowing that you have made the best choice for your healthcare coverage. We take people through this process daily. At no cost to you, we will show you the plans in your area that you are eligible for, break down the information on the chart, and match up with your unique needs and concerns. Call us at 402-614-3389 for a free consultation with a licensed insurance professional.
As people age, the value of good health becomes more important than ever. When you had a bad fall in your 40s, it would take a few weeks to recover. Now, a bad fall may result in a hip injury that takes months of recovery, doctor visits, physical therapy, or even surgery. Some must go to skilled nursing facilities to recover. The contrast is stark. Seniors’ health issues increase in frequency and complexity as they age. According to the National Council on Aging, nearly 95% of older adults have at least one chronic condition, and 3 million adults aged 65 or older are treated in emergency rooms due to fall-related injuries every year. So Medicare beneficiaries ask: How long Will Medicare Pay for nursing home care and home health care? 
Navigating the Complexities of Care: Medicare’s Coverage of Long-Term Care, Skilled Nursing Facilities, and Home Health Care
While preventative care is essential–annual physicals, screenings, and regular tests–and “fall-proofing” your home is critical, you must be prepared financially for the costs associated with extensive medical care if and when that occurs. If a health event puts you in a situation requiring special care or costly in-facility admittance, your first question will probably be, “How am I going to pay for this?”
If you are a Medicare recipient, navigating care in a long-term care facility can be complex and confusing. There are so many different types of care – long-term care (LTC), skilled nursing facility (SNF), and home healthcare (HH) – that it’s hard to know how it all works and how much Medicare is willing to pay for each.
My job is to make that journey a whole lot easier. I’ll break down each of these care types and dive into what Medicare will and won’t cover so that you know your options if you’re faced with a health challenge that requires ongoing care.
The Differences: LTC vs. SNF vs. HH
Understanding the different types of care offerings can feel like a full-time job for aging adults. Terms like assisted living facilities, senior living providers, and skilled nursing facilities are often used interchangeably, but the truth is, there are subtle differences in care and what and how much Medicare pays for the different types of “nursing home care.”
The three essential categories of care for seniors are long-term care (LTC), skilled nursing facilities (SNF), and home healthcare (HH). Understanding what each one does and its purpose can be beneficial when it comes time to finding care for your specific situation.
Long Term Care (LTC)
Long-Term Care facilities are the places we think of as “nursing homes.” A person may go to a long-term care facility for several reasons and lengths of stay. Permanent residents generally go to LTC facilities primarily because they can no longer perform the activities of daily living.
The 5 activities of daily living are:
- Feeding
- Dressing
- Personal Hygiene (bathing, brushing teeth, clipping nails, etc.)
- Continence (control of bladder and bowels)
- Toileting
If you struggle with any of the above, a Long-Term Care facility may be the right choice for you.
Staffed with caregivers, such as certified nurse assistants, registered nurses, various types of therapists, and doctors–these facilities focus more on providing meals, custodial care like dressing and feeding, and offering social environments for their patients. While also providing health care, the primary focus is custodial care because residents can no longer perform those functions for themselves, their families cannot care for them, and they cannot afford to provide those services in their own homes economically.
 Skilled Nursing Facility (SNF)
Skilled Nursing Facility (SNF)
Skilled nursing facilities are often in the same physical location as long-term care facilities. The difference comes down to the reason behind your stay. If you need care because of a medical condition – such as a broken hip from a fall, car accident, stroke, or heart attack – then an SNF can provide the medical care you need–intense nursing care, physical therapy, speech pathology. Custodial care, such as feeding or toileting, comes with a stay in the skilled nursing facility, but it is secondary to the primary reason for the stay–intense and daily treatment.
Seniors needing intense physical therapy, speech therapy, occupational therapy, or continuous medical support should reside in Skilled Nursing Facilities until they are recovered, reach a certain level, or plateau. Then you return home, where home healthcare takes over. The nurses, physical & occupational therapists, and speech pathologists come to your home. Eventually, when you have progressed in your recovery and do not need treatment as often, home healthcare stops, and you go to providers’ offices for an appointment.
Home Healthcare (HH)
Home Healthcare providers allow their clients to continue living in the comfort of their homes while providing care. The person still cannot get out and go to appointments easily, so the skilled providers come to you in your home two or three times a week or less, depending upon need. Ideally, in the recovery process, you eventually leave your home and go to their offices to receive treatment until you fully recover. Again, home healthcare does not provide custodial care in the home, except on rare occasions for short periods of time.
Understanding that Medicare is health insurance. It covers and pays for doctors, nurses, tests, hospitals–all the things you associate with medical treatment and recovery. Medicare does not provide custodial care, housekeeping, meal & laundry service, or taxis.
Will Medicare Cover Long-Term Care?
When someone says “long-term care” or “nursing home,” they generally mean the person is residing permanently in a facility because she cannot take care of herself–she cannot perform the 5 activities of daily living. Medicare does not pay for nursing home care. Even when medical necessity requires admittance to a nursing home (skilled nursing facility), the length of stay is capped at 100 days. There are rules around stopping and starting this coverage, coming from a hospital stay, and restarting a stay, but essentially, Medicare will only pay for 100 days per year in a nursing home. And Medicare approval for a stay of that length is rare. Again, Medicare pays for “nursing home” care for purposes of intense but temporary medical treatment.
Will Medicare Cover Skilled Nursing Facilities?
Medicare provides “Skilled Nursing Facilities” coverage, but patients must qualify based on stringent requirements. Medicare will only cover SNF care if all of the following are true:
- You are a recipient of Medicare Part A and have days of coverage remaining in your benefit period.
- A qualifying hospital stay preceded the need for SNF. An inpatient stay of at least 3 consecutive days in the hospital followed by admission into an SNF within 30 days of leaving the hospital is required for coverage.
- A doctor must have ordered inpatient SNF care based on medical necessity.
- Your condition requires skilled care daily.
- You need skilled services for an ongoing condition that was treated during your 3-day hospital stay OR a new condition that started while you were already receiving SNF care for an ongoing condition.
- The services must be reasonable and necessary for the treatment of your condition.
- You obtain care through a Medicare-certified SNF.
Even if you qualify, your stay will not last indefinitely.
How Many Days Will Medicare Pay for Skilled Nursing Care?
After qualifying for SNF care, your progress will be closely monitored for the length of your stay, the care you are receiving, and the above requirements to ensure Medicare will continue providing coverage. At a high level, Medicare will cover up to 100 days of SNF coverage within a single benefit period. Again, approval for that length of stay is rare. Medicare wishes to move you to less costly home healthcare as soon as medically possible.
In those 100 days, Medicare will cover the cost of the following:
- A semi-private room
- Meals
- Skilled nursing care
- Medical social services
- Medications
- Medical supplies and equipment usage
- Ambulance transport when required
- Dietary counseling
- Physical therapy, occupational therapy, and speech-language pathology when required to meet your health goal
It’s important to note that while Medicare will provide coverage for 100 days, you will have to supplement the coverage starting on day 21.
- Days 1 – 20: Medicare will pay the total cost; you pay nothing.
- Days 21 – 100: You pay the daily coinsurance, which can be up to $204 per day in 2024.
- Days 101+: Medicare pays nothing; you incur the total cost of care if you remain.
A detailed breakdown of coverage details can be found in Medicare’s SNF handbook. Medicare does not pay for nursing home care unless it is tied to a treatment program while you are in residence.
Will Medicare Cover Home Health Care?
Home healthcare falls under both Medicare Part A and Part B. Home healthcare is defined as part-time or intermittent skilled care when you are “homebound.” Homebound means you cannot leave your home without assistance. Assistance could be using a walker, wheelchair, crutches, or even a cane. You may need special transportation because of your condition. Your doctor may advise you not to leave your home because of your medical condition. These all constitute reasons Medicare will accept for home healthcare.
The usual services home healthcare provides on a part-time basis are:
- physical therapy
- occupation therapy
- speech-language pathology services
- Injectable osteoporosis drugs
- durable medical equipment
A doctor must certify you need home health care through a face-to-face meeting. You need part-time or intermittent care, which may be up to 8 hours per day but with a maximum of 28 hours per week.
Home Healthcare does not include:
- 24-hour adult day care at home
- Meals delivered to the home
- Homemaker services
- Custodial (or personal) care help.
If you do attend adult day care in a facility, you can still qualify for home healthcare.
Getting the Most from Your Medicare: Which Direction?
 There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
There are two ways for you to receive Medicare: Original Medicare or Medicare Advantage.
Original Medicare
Original Medicare is Part A for inpatient hospital stays and Part B for outpatient services and doctor visits. There are no networks for Original Medicare. It is fee-for-service (FFS), which means if the doctor or facility accepts Medicare–accept assignment for Medicare is the proper terminology–then Medicare will reimburse the provider for medically necessary services rendered.
Original Medicare does not include Part D for prescriptions, and Orignal Medicare has big gaps in coverage. A quarter of people purchase some sort of supplemental insurance policy, such as Medigap, to fill in the gaps in coverage.
Medicare Advantage/Part C
The other direction is Medicare Advantage (or Part C). These plans are provided by a private insurance company that is Medicare-approved to provide health coverage that is equal to or better than Original Medicare.
The gaps in coverage are structured differently than Original Medicare. Medicare Advantage plans have a maximum out-of-pocket. Original Medicare does not. For example, the most popular Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs have a maximum out-of-pocket of less than $4,000. Original Medicare, on the other hand, does not have a maximum. The sky is the limit for your out-of-pocket costs.
Medicare Advantage is also built on provider networks. The Omaha, Lincoln, Council Bluffs metro area has four healthcare networks: CHI (Catholic Health Initiative), Nebraska Medicine, Methodist Health Systems, and Bryan Hospital. All these networks work with the Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs. Access to providers is a non-issue for us. In other places and with other Medicare Advantage plans, there can be issues and problems, but not here.
Home healthcare is zero for both Original Medicare and most Medicare Advantage plans.
Skilled nursing is zero for the first 20 days for both. On the 21st day, Original Medicare has a copay of $204 during the potential 100 days of coverage–again with no cap on expenses for Part B. Medicare Advantage plans have copays of various sizes, but the key is a limit to what you could pay– a maximum out-of-pocket.
For those who pay the additional premium for the Medigap plan, the skilled nursing facility copay will usually be covered entirely.
Medicare Part D
Medicare Part D prescription drug plans are another premium. Most Medicare Advantage plans in Omaha, Lincoln, and Council Bluffs include the prescription drug plan and are mostly at zero cost.
Neither Original Medicare with a Medigap plan nor Medicare Advantage provides long-term care, custodial care, housekeeping, or adult day care. They may cover some of these services as incidental to providing skilled nursing care in a facility or home but for short periods.
Alternative Ways to Pay for the Care You Need
In 2021, the average cost of long-term care services ranged from $20,280 to $108,405 annually. These prices are exorbitant, and they’re only going up. As you age, the best thing you can do for your health and your wallet is to ensure you have the coverage you can rely on if you need long-term care. Since Medicare doesn’t pay for many long-term care scenarios–“nursing home care”–knowing your other options for coverage is crucial.
 Private Pay
Private Pay
Although challenging, some people will pay for their nursing home care from their savings and assets. By dipping into retirement accounts, tapping into assets such as property or investments, or simply saving up over their lifetimes, some seniors pay out-of-pocket for all the care they receive. This is rare.
One major benefit to this approach is that LTC facilities often prioritize private pay clients when space is limited. With the looming senior care crisis, this will get even more important in the years to come.
Long-Term Care Insurance
A separate long-term care insurance policy can pay the cost of residing in a long-term care facility. In most scenarios, these policies require that you need help with two or more of the activities of daily living (feeding, dressing, hygiene, continence, and toileting) before they take effect. There are usually elimination periods of 30, 60, 90, and 120 days before a policy will pay. The premiums for these insurance plans are not cheap. As you age, like life insurance, the price goes up and can be beyond the budget of many people. You also need to pass underwriting when you apply for the policy, though it will be guaranteed renewal for the rest of your life, no matter your health, as long as you continue to pay the monthly premium.
Veteran Benefits
If you served in the military, you may qualify for some sort of long-term care benefits from the Department of Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Veterans Affairs. Eligibility will depend upon length of service, type of service, military-related disabilities, and even income. Then, there may be limited or no facility access in your area. Where there is a facility, availability may be limited in terms of beds. Contact the Department of Veteran Affairs to determine for what you qualify. Access is very limited in Nebraska.
Medicaid
Often confused with Medicare, Medicaid is an entirely different health program. It’s partially funded by the federal government but funded and managed by the state.
Medicaid provides low-income seniors with financial help for long-term care. Each state has its own eligibility guidelines, but you’ll need to demonstrate financial need to qualify.
Many times people will tell me that so-in-so is in a “nursing home,” and they pay nothing. That is because all their assets have been depleted, and they are on county assistance. Medicaid is paying the bill, and all their assets are gone or will be upon death. The state takes homes and any other assets to offset the loss to the taxpayer who covers the expense.
 Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
Medicare Does Not Pay for Nursing Home Care: Your Health is in Your Hands
LTC, SNF, and HH are a jungle of terms, regulations, insurance, and costs. It is even confusing for experts. Like figuring out your income tax or finances, consulting an insurance professional will be helpful. You need someone who knows Medicare, Medicare insurance, the CMS rules and regulations, and possesses years of experience dealing with Medicare. He can guide you through the maze of Medicare and help you take your health care into your own hands and plan for the best outcome.
You’re in the right place if you’re unsure where to start. Every week, I spend time helping those on Medicare just like you find the right coverage for their needs. At Omaha Insurance Solutions, we can help you figureout the best direction for you, enroll you in Medicare, choose a plan, and get all the T’s cross and I’s dotted on forms and applications. Each year, we will review your needs and the plans available to maximize your Medicare benefits.

Christopher Grimmond
Get in touch with us today at 402-614-3389 for a free, no-obligation consultation about your Medicare options.
 Is Hospice Care Covered by Medicare?
Is Hospice Care Covered by Medicare?
When a loved one receives a terminal diagnosis, they’re typically given an average of six months to live. The next step is to find a place that can meet those special needs. While this is devastating news, the next logical step is to seek out options regarding hospice care to ensure a comfortable transition as their health continues to decline. Of course, figuring out how to pay for hospice care is part of that step. For those on Medicare, how much does Medicare cover for hospice care?
Understanding Medicare’s Hospice Care Coverage
Medicare, the federal health insurance program for individuals age 65 and over, offers coverage for hospice care under Part A. This coverage is available to eligible beneficiaries who have a terminal illness and have a life expectancy of six months or less. Medicare’s hospice care coverage includes a range of services, such as medical and nursing care, pain management, counseling, and medication.
To be eligible for Medicare hospice care, individuals must also be enrolled in Medicare Part A and have their doctor certify that they have a terminal illness with a life expectancy of six months or less. Additionally, individuals must sign a statement choosing hospice care instead of other Medicare-covered benefits for their terminal illness.
How Does Medicare Pay?
Medicare provides financial assistance for hospice care through its hospice benefit under Part A. Medicare Part A covers medications, medical equipment, nursing care, and counseling. The hospice provider is reimbursed directly by Medicare, and the provider must be Medicare-approved to receive reimbursements from Medicare. Beneficiaries are not responsible for any copays.
medical equipment, nursing care, and counseling. The hospice provider is reimbursed directly by Medicare, and the provider must be Medicare-approved to receive reimbursements from Medicare. Beneficiaries are not responsible for any copays.
Medicare’s payment structure for hospice care is based on a per diem (daily) rate. This means that Medicare pays a fixed amount to the hospice provider for each day that an individual is enrolled in hospice care. The per diem rate varies depending on the level of care provided. There may be higher rates for individuals receiving continuous home care or inpatient respite care.
However, it’s important to note that Medicare’s hospice benefit does not cover room and board in a hospice facility. If a beneficiary chooses to receive hospice care in a hospice facility, they may be responsible for paying the room and board costs out of pocket. Alternatively, if a beneficiary receives hospice care at home, Medicare will cover the cost of necessary medical equipment and supplies.
 Medigap & Medicare Advantage with Hospice Care
Medigap & Medicare Advantage with Hospice Care
Medicare Part A covers everything hospice-related. Patient costs are copays for hospice-covered medications and respite care. The copay for hospice medications is no higher than $5. Medicare Part A covers 95% of respite care for persons who have taken responsibility for the dying patient. The patient would be responsible for 5% of the costs.
If an individual has a Medigap policy, the Medigap policy would cover the hospice medications and the coinsurance for respite care. Medicare Advantage would continue to cover everything as before, but it would not normally cover the hospice medication copay or respite coinsurance payment.
It is important to note that there are many other medical costs for hospice patients during their time–non-hospice doctors, hospital beds, emergency room visits, ambulances, oxygen, walkers & wheelchairs, and other non-hospice medications, etc. These expenses fall under Original Medicare and the Medigap policy or Medicare Advantage. Hospice care does not cover these other medical needs. It is important to understand this fact.
Once time the daughter of a client called me to let me know her mother was going into hospice. One of the hospice workers told her to save money by canceling her Medigap policy. I tried to explain there were other medical costs her mother would incur from doctors and other providers, but she was convinced it was an unnecessary expense. Unfortunately, they don’t find out about their mistaken decisions until after the fact and the bills roll in.
Eligibility Requirements for Medicare Covered Hospice Care
To be eligible for Medicare hospice care, individuals must meet certain requirements. First, they must be enrolled in Medicare Part A, which provides hospital insurance coverage. Second, they must have a terminal illness. Terminal is defined as a life expectancy of six months or less, as certified by their doctor. Finally, they must sign a statement choosing hospice care instead of other Medicare-covered benefits for their terminal illness.
A beneficiary can stop hospice care at any point. They are not obliged to remain in hospice once they sign the statement.
It’s important to note that individuals can still receive Medicare hospice care even if they are enrolled in a Medicare Advantage plan. Medicare Advantage plans are private health insurance plans that provide Medicare benefits. You don’t lose Part A when you enroll in a Medicare Advantage plan. It is Part A that pays for hospice, even when you are enrolled in a Medicare Advantage plan.
How Long Does Medicare Pay for Hospice Care?
Once you are certified at the terminal with approximately six months or less of life expectancy, your doctor may recertify you. There are usually two 90-day periods and then every 60 days. You do not need to recommit to hospice. The doctor determines that you are still terminal with a six-month or less time period to live. You can remain in hospice almost indefinitely if you meet the criteria.
The Bottom Line: How Long Does Medicare Cover Palliative Care?

Christopher Grimmond
A quarter of the Medicare budget each year goes to cover the last year of Medicare beneficiaries’ lives. That is an incredible number. Hospice care is an essential part of Medicare.
The practice of hospice exists to provide comfort and optimal quality of life to individuals approaching the end. Medicare provides peace of mind that medical bills will be paid and that care will be provided uninterrupted. As long as a person continues to be certified for hospice, Medicare will continue to cover hospice care. You can be assured Medicare will be there for them the entire time.
Hospice is a difficult time. I have gone through this with both of my parents and with hundreds of clients. Contact us at Omaha Insurance Solutions to speak with a caring insurance professional about your Medicare needs. We are a call away at 402-614-3389.
 Finding a Medicare approved chiropractor can be a daunting task, especially if you’re dealing with chronic pain or a specific condition requiring specialized care. Knowing where to turn for effective treatment is crucial. That’s where our comprehensive guide comes in, dedicated to helping you navigate the world of Medicare approved chiropractors near you with ease.
Finding a Medicare approved chiropractor can be a daunting task, especially if you’re dealing with chronic pain or a specific condition requiring specialized care. Knowing where to turn for effective treatment is crucial. That’s where our comprehensive guide comes in, dedicated to helping you navigate the world of Medicare approved chiropractors near you with ease.
In this article, we’ll walk you through the process of finding local chiropractors near you who are covered by Medicare. You’ll learn about the specific criteria that chiropractors need to meet to be Medicare approved, ensuring you receive the best chiropractic care near you.
We’ll also provide tips on finding chiropractors in your area who accept Medicare, saving you valuable time and energy. From understanding Medicare coverage for chiropractic services to reviewing online directories and seeking referrals, we’ll cover it all.
Whether you’re new to Medicare or simply need a chiropractor who accepts this insurance, our guide will equip you with the knowledge and resources necessary to make informed decisions about your chiropractic care. Stay tuned for valuable insights and expert advice in the pages ahead.
Understanding Medicare Coverage for Chiropractic Services
Medicare coverage for chiropractic services can be complex, and it’s essential to understand what is and isn’t covered before seeking treatment. Chiropractic care falls under Medicare Part B, which covers medically necessary services and preventive care.
To be eligible for Medicare coverage, chiropractic services must meet specific criteria. Firstly, the treatment must be considered medically necessary, meaning it is aimed at diagnosing or treating a specific health condition. Additionally, the chiropractor must be a Medicare approved provider, and they must accept assignment. This means they agree to accept the Medicare approved amount as full payment for their services.
The process with Medicare Advantage plans is similar to Original Medicare. Each plan must approve the chiropractor to be in the network. There is a credentialing process providers go through to be accepted into the plan’s network. As part of the acceptance, they agree to the plan’s payment amounts.
It’s worth noting that Medicare only covers manual manipulation of the spine to correct a subluxation. Other services, such as acupuncture or massage therapy, are not covered under Original Medicare. Some Medicare Advantage plans may cover additional benefits, like acupuncture. Understanding these limitations will help you make informed decisions about your chiropractic care and plan.
 The Importance of Choosing a Medicare Approved Chiropractor
The Importance of Choosing a Medicare Approved Chiropractor
Choosing a Medicare approved chiropractor is crucial for several reasons. Firstly, it ensures that the chiropractor meets the necessary standards and qualifications Medicare sets. This gives you peace of mind, knowing you’re receiving care from a professional vetted by a trusted authority. That is for those who are on Original Medicare, which is Medicare Part A and Part B.
professional vetted by a trusted authority. That is for those who are on Original Medicare, which is Medicare Part A and Part B.
Medicare Advantage plans are managed care plans. The insurance company that runs the Medicare plans contracts with networks of doctors, health networks, hospitals, other healthcare facilities, and health professionals, like chiropractors. Each company and Medicare plan has its own vetting process called credentialing.
Secondly, choosing a Medicare approved chiropractor or in-network provider ensures that your services will be covered by Medicare or the particular Medicare Advantage plan in your area. This is particularly important if you’re relying on Medicare or Advantage plans to help with the cost of your chiropractic care. By selecting an approved provider, you can avoid unexpected out-of-pocket expenses.
Lastly, Medicare approved chiropractors have experience working with Medicare patients and navigating the complexities of billing and reimbursement. This means they are well-equipped to handle the administrative aspects of your care, allowing you to focus on your health and well-being.
How to Find Medicare Approved Chiropractors Near You
Finding Medicare-approved chiropractors in your local area is easier than you might think. Here are a few tips to help you get started:
 Use the Medicare.gov Physician Compare tool. This online directory allows you to search for chiropractors in your area who accept Original Medicare. Simply enter your location and select “chiropractor” as the specialty to find a list of Medicare approved chiropractors near you.
Use the Medicare.gov Physician Compare tool. This online directory allows you to search for chiropractors in your area who accept Original Medicare. Simply enter your location and select “chiropractor” as the specialty to find a list of Medicare approved chiropractors near you.
If you are on a Medicare Advantage plan, you can do the same with any of the insurance companies that sponsor a Medicare Advantage plan. The three largest plans in the Omaha, Lincoln, and Council Bluffs metro areas are United Healthcare, Aetna, and Humana. Go to their provider search tools on the plan website or downloadable their app on your phone. You can find all the chiropractors near you who accept the plan in order of distance from you.
you.
Check with your primary care physician. Your primary care physician may be able to recommend chiropractors who accept Medicare. They can provide valuable insights based on their knowledge of your medical history and specific needs.
Ask for referrals. Reach out to friends, family, or colleagues who have received chiropractic care with Medicare coverage. They can provide recommendations and share their experiences, helping you make an informed decision. Then check the chiropractor on one of the provider search tools.
 Factors to consider when selecting a chiropractor
Factors to consider when selecting a chiropractor
When selecting a chiropractor, there are several important factors to consider. These include:
1. Qualifications and credentials: Ensure that the chiropractor is licensed and has the necessary qualifications to provide chiropractic care. This includes checking their educational background, certifications, and any additional training they may have undergone.
2. Experience: Look for a chiropractor with experience treating your specific condition or dealing with similar cases. This can help ensure they have the expertise necessary to provide effective care.
3. Communication and bedside manner: A good chiropractor should communicate effectively, listen to your concerns, and make you feel comfortable throughout the treatment process. Pay attention to their communication style and how well they address your questions and concerns.
4. Treatment approach: Chiropractors may use different treatment approaches, so finding one whose approach aligns with your preferences and needs is important. Some chiropractors may focus on manual adjustments, while others may incorporate additional therapies or techniques.
By considering these factors, you can select a chiropractor who not only meets the Medicare-approved criteria but also aligns with your specific needs and preferences.
Medicare Billing & Reimbursement for Chiropractic Services
Understanding Medicare billing and reimbursement for chiropractic services can be complex. Medicare typically covers 80% of the Medicare approved amount for chiropractic services after you have met your annual deductible. This means you will be responsible for the remaining 20% as well as any applicable copayments or coinsurance. Medicare Supplements will fill in the gaps with Original Medicare. Medicare Advantage plans will probably have specific copays.
To ensure proper billing and reimbursement, it’s crucial to choose a chiropractor who accepts assignment. This means they agree to accept the Medicare-approved amount as full payment for their services. If the chiropractor does not accept assignment, you may be responsible for paying the difference between the Medicare-approved amount and their actual charges.
If on a Medicare Advantage plan, make sure he accepts that particular plan. Again consult the provider search tool the plan provides and/or ask the provider.
It’s also important to keep in mind that Medicare has specific documentation requirements for chiropractic services. The chiropractor must provide documentation that supports the medical necessity of the services provided. This documentation is crucial for proper billing and reimbursement. When clients call me complaining a service was denied, mistakes, lack of documentation, or incorrect billing codes are the usual reason. The medical office needs to correct any errors to receive approval and payment.
Common Misconceptions about Medicare Coverage for Chiropractic Care
There are several common misconceptions about Medicare coverage for chiropractic care. It’s important to debunk these misconceptions to ensure you clearly understand what is and isn’t covered. Here are a few common misconceptions:
1. Chiropractic care is covered without restrictions: While Original Medicare and Medicare Advantage plans do cover chiropractic care, it is subject to specific criteria. The treatment must be medically necessary and aimed at correcting a subluxation of the spine.
2. All chiropractors accept Medicare, and all insurance companies offer Medicare Advantage. Not all chiropractors accept Medicare or every Medicare Advantage plan in the area. Verifying that the chiropractor you choose is a Medicare-approved provider and in the network is vital.
 3. Medicare covers all chiropractic services: Medicare only covers manual manipulation of the spine to correct a subluxation. Additional services, such as acupuncture or massage therapy, are not covered by Original Medicare.
3. Medicare covers all chiropractic services: Medicare only covers manual manipulation of the spine to correct a subluxation. Additional services, such as acupuncture or massage therapy, are not covered by Original Medicare.
By understanding these misconceptions, you can make informed decisions about your chiropractic care and avoid unexpected expenses.
The Bottomline: Take Control of Your Healthcare with Medicare Approved Chiropractors
Navigating the world of Medicare-approved chiropractors doesn’t have to be overwhelming. With the information and resources provided in this guide, confidently search for chiropractic care that meets your needs and is covered by Medicare near you.
Remember to understand the specific criteria for Medicare coverage, choose a Medicare approved chiropractor, and ask the right questions during consultations. By staying informed and utilizing available resources, you can take control of your healthcare and receive the quality chiropractic care you deserve. We can help you sort through the confusion at Omaha Insurance Solutions. Give us a call at 402-614-3389 to speak with an experienced and licensed insurance agent professional.

Christopher J. Grimmond
Whether seeking relief from chronic pain or improving your overall well-being, Medicare approved chiropractors near you are here to help. Take the first step towards better health by exploring your options and finding a chiropractor who meets your needs. Your journey to wellness starts now.
How Does Medicare Advantage Work In Nursing Homes?
Taking care of our loved ones is always a top priority, especially regarding their health and well-being. For many seniors, nursing home care is necessary as they require specialized medical attention, like intense physical & occupational therapy and speech-language pathology. In such situations, it’s crucial to understand the nursing home coverage options available in Medicare Advantage plans.

Medicare Advantage plans offer all that Original Medicare (Part A & Part B) offers but through a private insurance company. The insurance companies that are the biggest underwriters of Medicare Advantage are United Healthcare, Humana, Aetna, and Blue Cross. Medicare Advantage plans must offer at least as much as Original Medicare but often offer even more. Nursing home care (the proper term is skilled nursing) is essential to Medicare Advantage. Exploring the different options among the various plans is critical.
This article will delve into nursing home coverage in Medicare Advantage plans, helping you make informed decisions about your loved one’s care. We will explore the different types of nursing home services, eligibility requirements, and potential limitations or restrictions. Whether you’re just considering nursing home care or actively searching for the right plan, this article will provide valuable insights to ensure you find the best solution for your loved one’s needs.
Understanding Medicare Advantage Plans Options
It seems like every year, I get at least one phone call from someone who has moved into a skilled nursing facility. “You sold me the wrong Medicare plan!”
They discover there is a gap in what they want and what Medicare provides. Sometimes billing personnel share misleading, incomplete, or incorrect information to fuel emotion and frustration.
Medicare Advantage plans are required by CMS (Center for Medicare & Medicaid Services) to cover all the services that Original Medicare covers. However, they can offer additional benefits such as prescription drug coverage, dental and vision care, and fitness programs. These plans may also have rules, costs, and restrictions that differ from Original Medicare. It’s important to carefully review the details of each plan to understand the specific nursing home coverage options available.
What Is Nursing Home Care & Why’s It So Important?
Nursing home care, also known as skilled nursing facility (SNF) care, is provided to individuals with a medical condition requiring round-the-clock nursing care. The patient may also need assistance with activities of daily living, such as, help with bathing, dressing, and eating. Their complex medical needs prevent them from being safely cared for at home or in an assisted living facility. SNF provides a safe and supportive environment where seniors can receive the care they need to improve their health and quality of life.
Nursing Home Care vs. Home Healthcare
Home healthcare, which is an alternative to residence in a skilled nursing facility, would not be an adequate solution in some cases because patients would not be able to get the necessary therapy in a timely manner, with the same intensity, and in a safe environment. Their home lacks the equipment and personnel to ensure their therapy is conducted safely and with enough frequency.
Each Medicare Advantage plan may cover nursing home care differently. Some plans may provide full coverage for certain days in a skilled nursing facility, while others may require a copayment or coinsurance for each day of care. It’s essential to review the specific details of each plan to understand the coverage options available.
 How Long Does Medicare Pay?
How Long Does Medicare Pay?
Original Medicare covers skilled nursing facility care at 100% for the first 20 days. Days 21-100, the copay is $200 or more. Of course, if you purchase a Medicare supplement for an additional premium, you can fill in some or all of that gap. Premiums in the Omaha, Lincoln, & Council Bluff metro area are around $100-$175 for 65-year-olds.
Medicare Advantage plans vary in the extent of their coverage. I’m always surprised how quickly people pass over the skilled nursing facility section of the benefit highlights in the Medicare Advantage plan’s outline of coverage. I think the assumption is they will never be in a nursing home.
One Medicare Advantage plan in our area covers the first 20 days at zero copays. Days 21-40 (or 19 days) are $196 per day. On day 41, the copay returns to zero on that plan until day 100. Another Medicare Advantage plan in our area covers the first 20 days at zero, but day 21-100 is $196 for the entire period. The second plan has some other very enticing benefits, but that is a huge hole in coverage.
Differences like that are certainly worth considering more than other benefits like dental and vision, even if those benefits are richer. A skilled nursing facility stay can significantly dent one’s pocketbook.
 What Is Home Healthcare?
What Is Home Healthcare?
In addition to coverage for skilled nursing facility care, Medicare Advantage plans also offer home health care services. Home healthcare is the alternative to skilled nursing facility care or the logical progression from skilled nursing.
Home healthcare is, as it says, care in the home. Physical and occupational therapists come to the home. Speech pathologists perform therapy in the home. Wound nurses come to the home to change dressings.
Home healthcare is less intense. For example, in home healthcare, a patient would get by seeing a therapist thrice a week for an hour versus three hours daily in a skilled nursing facility. The person’s illness does not require custodial care, like bathing, dressing, and feeding, during the treatment process. She is independent enough to carry out these activities on her own or with the assistance of a family member.
Home healthcare is also less expensive, so it may be chosen over skilled nursing care in a facility. The high cost of SNF is why the flow is to get the patient home and out of the skilled nursing facility as soon as adequate progress is made.
Qualifying Criteria for Nursing Homes in Medicare Advantage
Individuals generally need to meet specific criteria to qualify for nursing home coverage in a Medicare Advantage plan, as well as Original Medicare. This includes a qualifying hospital stay, where they are admitted for at least three consecutive days as an inpatient before being transferred to a skilled nursing facility. In addition, individuals must require skilled nursing care or therapy services daily. It is important to understand the purpose of a skilled nursing facility is not nursing home care. The SNF is not a place of convalescence after surgery or a traumatic event. SNF is for intense therapy; the term ends when the therapy ends or can be continued as an outpatient.
 Limitations & Restrictions on Nursing Homes in Medicare Advantage
Limitations & Restrictions on Nursing Homes in Medicare Advantage
While Medicare Advantage plans may offer coverage for nursing home care, it’s important to be aware of any applicable limitations or restrictions. For example, the plan may require prior authorization to continue treatment beyond twenty days. Patients and/or family members often want the nursing home stay prolonged. The plan, however, will not approve any more days because the person has completed the treatment or has reached a plateau in her recovery.
This can cause distress because the person is not ready to be alone at home. Their home is not adequately equipped with ramps or lifts. No one can attend to the patient without significant expense or inconvenience during her continued recovery.
Medicare Advantage plans are managed care plans. They carefully monitor treatment following Medicare’s criteria. The point is to protect from waste or abuse of the limited resources from the Medicare trust fund while also providing the proper care.
Medicare Advantage Is Bad Insurance
In my experience, this situation is exasperated when SNF billing personnel complain to patients and their families that Original Medicare is not as strict as the Medicare Advantage plans in monitoring and restricting treatment. I probably get this phone call once a year. “You sold me the wrong Medicare plan!”
restricting treatment. I probably get this phone call once a year. “You sold me the wrong Medicare plan!”
Patients and families are already in extreme distress because of the medical situation of their loved ones. I find it cruel and unprofessional to burden the family with medical billing challenges, mainly because nothing can be done to change the immediate circumstances of their insurance.
Skilled Nursing Facilities are also far from impartial and unbiased. Their monetary gain is significant if they can keep patients for the full 100 days and bill for therapy versus only 20 or even 30 days.
The reality is therapy has come to an end. The patient can be cared for at home, and treatment may continue with home healthcare. Medicare is health insurance and is not designed for caretaking, food preparation, maid service, and companion care.
People, however, observe that nursing homes are full of people who are cared for in this manner. Those individuals pay for that custodial service out of their own pocket or have long-term care (LTC) insurance. Or they are indigent and on state Medicaid. The citizens then of the county where they reside are paying the monthly rate.
Tips for Choosing the Right Medicare Advantage Plan for Nursing Home Coverage
 If you choose to go the direction of Medicare Advantage instead of Original Medicare with a Medicare Supplement, understanding the place of nursing home coverage in a Medicare Advantage plan is important.
If you choose to go the direction of Medicare Advantage instead of Original Medicare with a Medicare Supplement, understanding the place of nursing home coverage in a Medicare Advantage plan is important.
Here are some tips to help you navigate the process:
1. Consider the specific nursing home coverage options offered by each plan. What are the copays for which days?
2. Review the costs associated with nursing home care in each plan. We have 22 Medicare Advantage plans in the Omaha, Lincoln, and Council Bluffs areas. Put them side-by-side.
3. Research the network of skilled nursing facilities covered by each plan. Have the agent look up the skilled nursing facilities you would be most interested in. Make sure they are in the network.
4. Consider the reputation and customer satisfaction ratings of the insurance companies offering Medicare Advantage plans. Medicare has a star rating system: 5-star is best; 1-star is worst.
5. Look at ancillary insurance products that may fill in the gaps that Original Medicare or Medicare Advantage do not cover, like Long-Term Care; Home Care; Cancer, Heart Attack, and Stroke policies.
6. Consult with an independent and impartial insurance agent who can act as a broker for both Medicare Advantage plans in your area as well as Medicare Supplements.
The Bottom Line: Making informed decisions about nursing home coverage in Medicare Advantage plans
All insurance, even Medicare, has rules, limitations, and restrictions. Healthcare, especially when it comes to critical illness, is expensive. When caring for our loved ones, understanding the nursing home coverage options in Medicare Advantage plans is essential. By exploring the different types of nursing home services covered, eligibility requirements, and potential limitations or restrictions, you can make informed decisions to ensure your loved one receives the care they need.

Christopher J. Grimmond
Omaha Insurance Solutions offers Medicare Supplements and Medicare Advantage plans from all major insurance companies. We can explain the plans, the differences, the pros & cons, so you can determine what is the best fit for you. Your health needs change over time, so we review your plan annually to ensure you have the best Medicare plan that meets your unique needs. Call us at 402-614-3389 to speak with an experienced and licensed insurance agent profession.








